Nightmare disorder is a mental health condition characterized by severe dysphoric, terrifying and well-remembered dreams resulting in abrupt awakenings. The disorder may be caused by various factors like stress, trauma, genetics and other comorbid conditions.
What Is Nightmare Disorder?
Nightmares are disturbing or upsetting dreams that may be caused or influenced by a plethora of different factors. When nightmares occur repeatedly and for extended periods of time, then it may lead to nightmare disorder. Previously known as dream anxiety disorder, the condition is a sleep disorder and a type of parasomnia. Patients experience frightening nightmares that may vary in severity and frequency.
It may cause disruptions in the sleep-wake cycle and lead to abrupt awakenings, making the sufferer instantly alert upon waking up. Hence, they may have difficulty going back to sleep. Nightmares typically tend to involve themes of threats to survival, security, or physical integrity. Although mostly, observed in children, adults may also be affected by the condition.
Understanding The Causes Of Nightmare Disorder
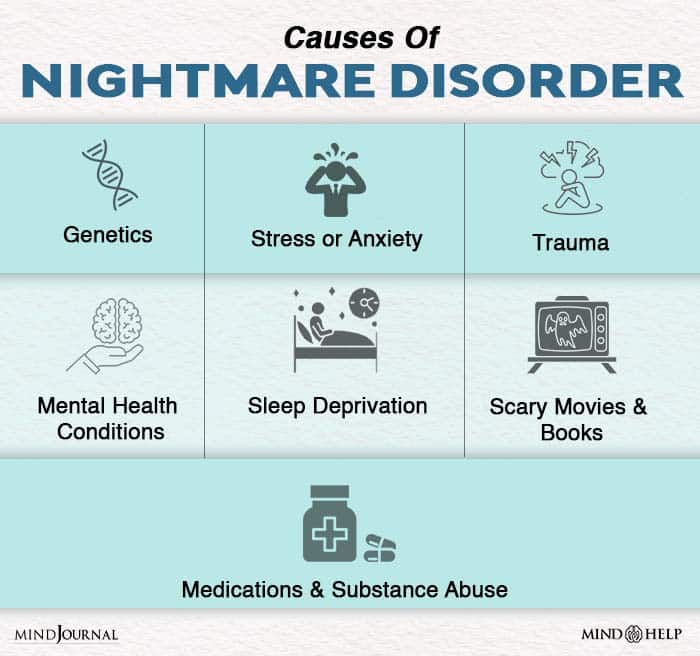
The exact cause of nightmare disorder is yet to be known. However, repeated nightmares often tend to have an underlying cause. Studies 1 Levin R, Nielsen TA. Disturbed dreaming, posttraumatic stress disorder, and affect distress: a review and neurocognitive model. Psychol Bull. 2007 May;133(3):482-528. doi: 10.1037/0033-2909.133.3.482. PMID: 17469988. reveal that “No models adequately explain nightmares nor have they been reconciled with recent developments in cognitive neuroscience, fear acquisition, and emotional memory.”
Although more research is needed to explain the precise causes of nightmares and the disorder, there may be some contributing factors that may influence its occurrence in someone. Here are some of the most common factors that may lead to the development of dream anxiety disorder:
1. Stress and anxiety
Anxiety and stress are considered as major influencing factors for nightmares. Often, normal stress experienced in daily life, such as issues at school or work, household responsibilities, relationship problems or stressful life events, can trigger nightmares. Moreover, major negative life events such as unemployment, loss of a loved one, moving to a new city can also cause disturbing dreams. As anxiety tends to increase the risk of the condition, nightmares can be a result of emotional response to stress, anxiety, fear and trauma.
Researchers believe that dreams are a way for the human mind to process emotions and integrate memories. One 2019 study 2 Scarpelli S, Bartolacci C, D’Atri A, Gorgoni M, De Gennaro L. Mental Sleep Activity and Disturbing Dreams in the Lifespan. Int J Environ Res Public Health. 2019 Sep 29;16(19):3658. doi: 10.3390/ijerph16193658. PMID: 31569467; PMCID: PMC6801786. highlights that “nightmares and bad dreams might represent an attempt to cope with adverse events, and the degrees of cognitive-brain maturation could impact on these mechanisms across the lifespan.”
Read More About Generalized Anxiety Disorder Here
2. Trauma
Trauma is one of the most common reasons for experiencing nightmares. About 80% of people suffering from post-traumatic stress disorder (PTSD) have frequent nightmares. A 2000 study 3 Pagel JF. Nightmares and disorders of dreaming. Am Fam Physician. 2000 Apr 1;61(7):2037-42, 2044. PMID: 10779247. explains “recurrent nightmares are the most defining symptom of post-traumatic stress disorder and may be associated with other psychiatric illnesses.” Many individuals tend to have nightmares after surviving –
- Emotional, physical or sexual abuse
- An accident
- Serious injury
- Death of loved one
- Other traumatic experiences
PTSD patients often experience nightmares as intrusive/re-experiencing symptoms that may involve avoidance, arousal, dissociation and negative mood. “Post-traumatic stress disorder produces recurrent and repetitive nightmares,” explains a study 4 Pagel JF Jr. Nightmares. Am Fam Physician. 1989 Mar;39(3):145-8. PMID: 2646879. . The sufferer may have repeated nightmares about the past traumatic event and have flashbacks.
This can lead to sleep disturbance, hypervigilance and avoidance of triggers that remind them of the trauma. Another study 5 Ross RJ, Ball WA, Sullivan KA, Caroff SN. Sleep disturbance as the hallmark of posttraumatic stress disorder. Am J Psychiatry. 1989 Jun;146(6):697-707. doi: 10.1176/ajp.146.6.697. PMID: 2658624. reports “The re-experiencing of a traumatic event in the form of repetitive dreams, memories, or flashbacks is one of the cardinal manifestations of posttraumatic stress disorder (PTSD).” Nightmares can also be experienced by a person affected with acute stress disorder (ASD).
3. Hyperarousal and impaired fear extinction
A 2019 scientific analysis 6 Gieselmann A, Ait Aoudia M, Carr M, Germain A, Gorzka R, Holzinger B, Kleim B, Krakow B, Kunze AE, Lancee J, Nadorff MR, Nielsen T, Riemann D, Sandahl H, Schlarb AA, Schmid C, Schredl M, Spoormaker VI, Steil R, van Schagen AM, Wittmann L, Zschoche M, Pietrowsky R. Aetiology and treatment of nightmare disorder: State of the art and future perspectives. J Sleep Res. 2019 Aug;28(4):e12820. doi: 10.1111/jsr.12820. Epub 2019 Jan 29. PMID: 30697860; PMCID: PMC6850667. suggests that the cause for the development of nightmare disorder may be associated with hyperarousal which accumulates during daytime and is sustained at nighttime. “Elevated hyperarousal is discussed as a central pathophysiological factor in PTSD,” which can explain the aetiology of nightmares. The study also highlights that impaired fear extinction can also be an influencing factor.
The study adds that even though sleep and dreams can “enable fear extinction through a process of recombining fearful memories with novel and dissociated contexts, individuals with nightmare disorder continue to activate arousing memory fragments during sleep, reinforcing fear memories.” Hyperarousal & impaired fear extinction in people with dream anxiety disorder can be influenced by several factors, like –
- Physiological factors
- Maladaptive cognitive factors
- Trait susceptibility
- Childhood adversity
- Trauma
4. Childhood adversity
As developmental stress and adverse experiences during childhood can impair fear extinction capacity, it can also be a determining factor for the onset of the condition. Negative childhood experiences can trigger “changes in mPFC–amygdala circuits” that are related to heightened threat perception 7 Ochsner KN, Gross JJ. The cognitive control of emotion. Trends Cogn Sci. 2005 May;9(5):242-9. doi: 10.1016/j.tics.2005.03.010. PMID: 15866151. and dysphoric dreaming 8 Nielsen T, Levin R. Nightmares: a new neurocognitive model. Sleep Med Rev. 2007 Aug;11(4):295-310. doi: 10.1016/j.smrv.2007.03.004. Epub 2007 May 11. PMID: 17498981. . As a result, childhood adversity can affect the development of emotion regulation and disrupt emotional expression, which may “reinforce the development of a fear memory.”
This notion was expressed in the 2017 research paper 9 Nielsen T. The Stress Acceleration Hypothesis of Nightmares. Front Neurol. 2017 Jun 1;8:201. doi: 10.3389/fneur.2017.00201. PMID: 28620339; PMCID: PMC5451501. titled ‘The Stress Acceleration Hypothesis of Nightmares (SAH).’ Lead author and psychiatrist Tore Nielsen states “idiopathic nightmares are hypothesized to originate in early adverse experiences that lead in later life to the expression of early memories and emotions in dream content.”
The SAH model suggests that early childhood memories are often suppressed after the infantile amnesia period. However, disruption of infantile amnesia can influence cognitions, emotions & behaviors in later life, including expression of dangers and threats in nightmares. Moreover, changes in emotion regulation processes cause reduced fear extinction in REM sleep and any disruptions causes nightmares.
Read More About Childhood Here
5. Psychiatric disorders
Nightmare disorder is often associated with a number of other mental conditions such as depression, borderline personality disorder and schizophrenia. Depression can often cause sleep disorders 10 Luca, A., Luca, M., & Calandra, C. (2013). Sleep disorders and depression: brief review of the literature, case report, and nonpharmacologic interventions for depression. Clinical interventions in aging, 8, 1033–1039. https://doi.org/10.2147/CIA.S47230 , such as nightmares, hypersomnia, and insomnia. A 2018 study 11 Don Richardson J, King L, St Cyr K, Shnaider P, Roth ML, Ketcheson F, Balderson K, Elhai JD. Depression and the relationship between sleep disturbances, nightmares, and suicidal ideation in treatment-seeking Canadian Armed Forces members and veterans. BMC Psychiatry. 2018 Jun 19;18(1):204. doi: 10.1186/s12888-018-1782-z. PMID: 29921268; PMCID: PMC6011186. shows that nightmares can often manifest as symptoms of major depressive disorder and treating depression can not only improve sleep difficulties but may also reduce suicidal thoughts as well.
Research 12 Agargun MY, Besiroglu L, Cilli AS, Gulec M, Aydin A, Inci R, Selvi Y. Nightmares, suicide attempts, and melancholic features in patients with unipolar major depression. J Affect Disord. 2007 Mar;98(3):267-70. doi: 10.1016/j.jad.2006.08.005. Epub 2006 Aug 28. PMID: 16938351. also shows that in depressed people, “Feeling worse in the morning than later in the day may be related to the intervening dream content and affect and predict suicidal tendency.” Nightmare disorder is also common among patients with dissociative disorders (DD) with a prevalence rate of about 57% of DD patients. A 2003 study 13 Agargun MY, Kara H, Ozer OA, Selvi Y, Kiran U, Ozer B. Clinical importance of nightmare disorder in patients with dissociative disorders. Psychiatry Clin Neurosci. 2003 Dec;57(6):575-9. doi: 10.1046/j.1440-1819.2003.01169.x. PMID: 14629705. revealed, “Among patients with DD, those with ND had a higher rate of self-mutilative behavior, a history of suicide attempt in the last year, and comorbidity with borderline personality disorder than those without ND.”
Another 2008 study 14 Semiz UB, Basoglu C, Ebrinc S, Cetin M. Nightmare disorder, dream anxiety, and subjective sleep quality in patients with borderline personality disorder. Psychiatry Clin Neurosci. 2008 Feb;62(1):48-55. doi: 10.1111/j.1440-1819.2007.01789.x. PMID: 18289141. reveals that patients with borderline personality disorder (BPD) experience higher levels of dream anxiety. The study states “BPD patients suffered a significantly greater rate of nightmares, elevated levels of dream anxiety, and disturbed sleep quality,” than others. Moreover in BPD patients, heightened dream anxiety is associated with higher incidences of early traumatic experiences. People with schizophrenia or psychosis are also prone to having frequent episodes of nightmares. According to a 2015 study 15 Sheaves, B., Onwumere, J., Keen, N., Stahl, D., & Kuipers, E. (2015). Nightmares in Patients With Psychosis: The Relation With Sleep, Psychotic, Affective, and Cognitive Symptoms. Canadian journal of psychiatry. Revue canadienne de psychiatrie, 60(8), 354–361. https://doi.org/10.1177/070674371506000804 , 55% of patients with psychotic symptoms reported distressing nightmares on a weekly basis. It states “Nightmares might be common in those with psychosis and are associated with increased day and nighttime impairment.”
Nightmares are also associated with personality disorders. “Frequent nightmares were independently related to the neuroticism personality trait, irrespective of psychiatric diagnosis,” states a 2010 study 16 Li, S. X., Zhang, B., Li, A. M., & Wing, Y. K. (2010). Prevalence and correlates of frequent nightmares: a community-based 2-phase study. Sleep, 33(6), 774–780. https://doi.org/10.1093/sleep/33.6.774 . Apart from these, disturbing and terrifying dreams are associated with higher levels of paranoia, hallucinatory experiences and depersonalisation reveals further research 17 Rek, S., Sheaves, B., & Freeman, D. (2017). Nightmares in the general population: identifying potential causal factors. Social psychiatry and psychiatric epidemiology, 52(9), 1123–1133. https://doi.org/10.1007/s00127-017-1408-7 . Nightmares are also found to be linked with different medical conditions, like cancer, heart disease, restless legs syndrome, sleep apnea and other sleep disorders.
6. Genetics
It has been observed that individuals who have a first-degree relative with nightmare disorder are more likely to develop the condition. The condition may run in families 18 Hublin C, Kaprio J, Partinen M, Koskenvu M. Parasomnias: co-occurrence and genetics. Psychiatr Genet. 2001 Jun;11(2):65-70. doi: 10.1097/00041444-200106000-00002. PMID: 11525419. and indicates a role of genetic factors 19 Hublin C, Kaprio J, Partinen M, Koskenvuo M. Nightmares: familial aggregation and association with psychiatric disorders in a nationwide twin cohort. Am J Med Genet. 1999 Aug 20;88(4):329-36. doi: 10.1002/(sici)1096-8628(19990820)88:4<329::aid-ajmg8>3.0.co;2-e. PMID: 10402498. . One 2012 study 20 Bidaki, R., Zarei, M., Khorram Toosi, A., & Hakim Shooshtari, M. (2012). A review on genetics of sleep disorders. Iranian journal of psychiatry and behavioral sciences, 6(1), 12–19. has found that sleep disorders are often caused by “complex interactions between genes and the environment.” A 2019 study 21 Wang, C., Shao, X., Jia, Y. et al. Nightmare experience and family relationships in healthy volunteers and nightmare disorder patients. BMC Psychiatry 19, 297 (2019). https://doi.org/10.1186/s12888-019-2299-9 has found that nightmares are often related to parental bonding styles, but precise connections between family relationships and nightmare experiences is yet to be identified. The researchers state “Our study has demonstrated that the inappropriate family relationships were linked with different aspects of nightmare experience, especially in nightmare disorder patients.” However, more research may be required to establish this theory.
7. Medications and substance abuse
Nightmare disorder may also be influenced by different medication and misuse of alcohol and recreational drugs or withdrawal from substances. Medications which change the neurotransmitter levels of the central nervous system can cause intensely frightening dreams. Medications like beta blockers 22 Farzam K, Jan A. Beta Blockers. [Updated 2020 Nov 27]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK532906/ , antidepressants, anesthetics, antipsychotics, antiepileptic agents, blood pressure medicines, Parkinson’s disease medicines or medication to quit smoking and other non-psychological medicines can often trigger nightmares. A 2003 research 23 Pagel JF, Helfter P. Drug induced nightmares–an etiology based review. Hum Psychopharmacol. 2003 Jan;18(1):59-67. doi: 10.1002/hup.465. PMID: 12532316. found that “Pharmacological agents affecting the neurotransmitters norepinephrine, serotonin and dopamine are clearly associated with patient reports of nightmares.”
One study 24 Thompson DF, Pierce DR. Drug-induced nightmares. Ann Pharmacother. 1999 Jan;33(1):93-8. doi: 10.1345/aph.18150. PMID: 9972389. reveals that “sedative/hypnotics, beta-blockers, and amphetamines are the therapeutic modalities most frequently associated with nightmares.” Moreover, dopamine agonists may also cause this condition “with dopamine receptor stimulation as a possible pharmacologic mechanism.” Another study 25 Westerlund A. Central nervous system side-effects with hydrophilic and lipophilic beta-blockers. Eur J Clin Pharmacol. 1985;28 Suppl:73-6. doi: 10.1007/BF00543714. PMID: 2865153. found that lipophilic beta-blockers can cause nightmares and hallucinations in patients.
Antidepressants can also induce or worsen sleep disorders like nightmares and REM sleep behavior disorder. “Although antidepressants are recommended for the treatment of post-traumatic sleep disorder, they can induce nightmares,” explains a 2017 study 26 Wichniak, A., Wierzbicka, A., Walęcka, M., & Jernajczyk, W. (2017). Effects of Antidepressants on Sleep. Current psychiatry reports, 19(9), 63. https://doi.org/10.1007/s11920-017-0816-4 . Moreover, withdrawal from “drugs affecting GABA and acetylcholine, can also be associated with nightmares,” according to a 2010 research paper 27 Aurora, R. N., Zak, R. S., Auerbach, S. H., Casey, K. R., Chowdhuri, S., Karippot, A., Maganti, R. K., Ramar, K., Kristo, D. A., Bista, S. R., Lamm, C. I., Morgenthaler, T. I., Standards of Practice Committee, & American Academy of Sleep Medicine (2010). Best practice guide for the treatment of nightmare disorder in adults. Journal of clinical sleep medicine : JCSM : official publication of the American Academy of Sleep Medicine, 6(4), 389–401. .
Narcotics which affect the chemicals in the brain can also influence the severity of the disorder. Withdrawal from medications, such as benzodiazepines 28 Pétursson H. The benzodiazepine withdrawal syndrome. Addiction. 1994 Nov;89(11):1455-9. doi: 10.1111/j.1360-0443.1994.tb03743.x. PMID: 7841856. and ethanol can result in REM sleep rebound and cause nightmares. Withdrawal from substances, including tranquilizers, alcohol and drugs can also have the same effect. This is why it is crucial to inform your doctor about any medication or drug you may be taking during the time of diagnosis and treatment.
8. Sleep deprivation
Changes in the sleep schedule and sleep disturbances that reduce or interrupt the quality and amount of sleep or cause abnormal sleep-wake times can also increase the risk of experiencing nightmares frequently. Studies 29 Dollander M. Etiologies de l’insomnie chez l’adulte [Etiology of adult insomnia]. Encephale. 2002 Nov-Dec;28(6 Pt 1):493-502. French. PMID: 12506261. have found that insomnia is also associated with repetitive nightmares and abrupt awakenings. The researchers state “intermittent or early waking insomnia is sometimes associated with nightmares.” However, it has not yet been confirmed whether sleep deprivation can cause nightmare disorder.
9. Disturbing fiction and scary movies, books etc.
Books, movies or video games that have scary, terrifying or disturbing themes are also linked with causing nightmare disorder. For certain individuals, watching horror movies or reading ghost stories, particularly before bed, can result in repeated nightmares. A 2013 study 30 Zisenwine T, Kaplan M, Kushnir J, Sadeh A. Nighttime fears and fantasy-reality differentiation in preschool children. Child Psychiatry Hum Dev. 2013 Feb;44(1):186-99. doi: 10.1007/s10578-012-0318-x. PMID: 22760490. found that children exposed to terrifying images showing real or fantastic situations and entities can cause nighttime fears and issues with fantasy-reality differentiation.
10. Maladaptive beliefs
A 2019 research suggests that certain maladaptive beliefs may also play a contributing role in the development of nightmare disorder. The researchers state that recent studies focusing on the “volitional attempt to suppress unwanted thoughts and feelings (thought suppression) finds that such attempts increase the likelihood that the suppressed thoughts 31 Wegner DM, Wenzlaff RM, Kozak M. Dream rebound: the return of suppressed thoughts in dreams. Psychol Sci. 2004 Apr;15(4):232-6. doi: 10.1111/j.0963-7214.2004.00657.x. PMID: 15043639. reoccur in a person’s dreams, especially those in REM sleep.” Moreover, research 32 Kramer M, Kinney L. Vigilance and avoidance during sleep in US Vietnam War veterans with posttraumatic stress disorder. J Nerv Ment Dis. 2003 Oct;191(10):685-7. doi: 10.1097/01.nmd.0000092179.74348.20. PMID: 14555872. also reveals that deliberately avoiding external and internal stimuli can lead to repeated nightmares. Hence, intentional thought suppression can trigger and influence the onset of nightmare disorder as well.
Risk Factors Of Nightmare Disorder
Apart from the reasons mentioned above, there are some other risk factors which can cause nightmare and lead to the development of dream anxiety disorder, such as:
- Eating snacks before bedtime
- Fever or illness
- Sleep disorders, like sleep terror disorder or narcolepsy
- Trouble breathing during sleep, like sleep apnea
- Jet lag
Read More About Jet lag Here
How Nightmare Disorder Can Affect You?
“Frequent nightmares can pose a serious clinical problem,” explains a 2017 study 33 Sandman, N., Valli, K., Kronholm, E., Vartiainen, E., Laatikainen, T., & Paunio, T. (2017). Nightmares as predictors of suicide: an extension study including war veterans. Scientific reports, 7, 44756. https://doi.org/10.1038/srep44756 . When left untreated, repeated nightmares can adversely impact your mental and physical well being. Nightmares awaken the sufferer from rapid eye movement sleep 34 Paul, F., Schredl, M., & Alpers, G. W. (2015). Nightmares affect the experience of sleep quality but not sleep architecture: an ambulatory polysomnographic study. Borderline personality disorder and emotion dysregulation, 2, 3. https://doi.org/10.1186/s40479-014-0023-4 (REM sleep or REMS) and cause chronic sleep disturbances leading to insomnia. Studies show that 2-8% of people have recurrent nightmares while 50-85% of people have at least one nightmare occasionally.
Nightmare disorder can “cause clinically significant distress or impairment in social, occupational or other important areas of functioning,” as per a 2019 study 35 Gieselmann, A., Ait Aoudia, M., Carr, M., Germain, A., Gorzka, R., Holzinger, B., Kleim, B., Krakow, B., Kunze, A. E., Lancee, J., Nadorff, M. R., Nielsen, T., Riemann, D., Sandahl, H., Schlarb, A. A., Schmid, C., Schredl, M., Spoormaker, V. I., Steil, R., van Schagen, A. M., … Pietrowsky, R. (2019). Aetiology and treatment of nightmare disorder: State of the art and future perspectives. Journal of sleep research, 28(4), e12820. https://doi.org/10.1111/jsr.12820 . It can also cause severe anxiety and depression in some people along with other psychological ill effects. In extreme cases, nightmares can also cause suicidal ideation 36 Nadorff, M. R., Pearson, M. D., & Golding, S. (2016). Explaining the Relation between Nightmares and Suicide. Journal of clinical sleep medicine : JCSM : official publication of the American Academy of Sleep Medicine, 12(3), 289–290. https://doi.org/10.5664/jcsm.5564 and behaviour. Moreover, sleep avoidance and deprivation, usually caused by nightmare disorder, can result in different conditions, including heart disease, obesity etc. When left untreated, the condition can significantly affect your personal, professional and social life.
Hence if you are experiencing frequent nightmares, then make sure to consult a doctor or a mental health professional to diagnose your symptoms and receive medical care immediately.
References:
- 1Levin R, Nielsen TA. Disturbed dreaming, posttraumatic stress disorder, and affect distress: a review and neurocognitive model. Psychol Bull. 2007 May;133(3):482-528. doi: 10.1037/0033-2909.133.3.482. PMID: 17469988.
- 2Scarpelli S, Bartolacci C, D’Atri A, Gorgoni M, De Gennaro L. Mental Sleep Activity and Disturbing Dreams in the Lifespan. Int J Environ Res Public Health. 2019 Sep 29;16(19):3658. doi: 10.3390/ijerph16193658. PMID: 31569467; PMCID: PMC6801786.
- 3Pagel JF. Nightmares and disorders of dreaming. Am Fam Physician. 2000 Apr 1;61(7):2037-42, 2044. PMID: 10779247.
- 4Pagel JF Jr. Nightmares. Am Fam Physician. 1989 Mar;39(3):145-8. PMID: 2646879.
- 5Ross RJ, Ball WA, Sullivan KA, Caroff SN. Sleep disturbance as the hallmark of posttraumatic stress disorder. Am J Psychiatry. 1989 Jun;146(6):697-707. doi: 10.1176/ajp.146.6.697. PMID: 2658624.
- 6Gieselmann A, Ait Aoudia M, Carr M, Germain A, Gorzka R, Holzinger B, Kleim B, Krakow B, Kunze AE, Lancee J, Nadorff MR, Nielsen T, Riemann D, Sandahl H, Schlarb AA, Schmid C, Schredl M, Spoormaker VI, Steil R, van Schagen AM, Wittmann L, Zschoche M, Pietrowsky R. Aetiology and treatment of nightmare disorder: State of the art and future perspectives. J Sleep Res. 2019 Aug;28(4):e12820. doi: 10.1111/jsr.12820. Epub 2019 Jan 29. PMID: 30697860; PMCID: PMC6850667.
- 7Ochsner KN, Gross JJ. The cognitive control of emotion. Trends Cogn Sci. 2005 May;9(5):242-9. doi: 10.1016/j.tics.2005.03.010. PMID: 15866151.
- 8Nielsen T, Levin R. Nightmares: a new neurocognitive model. Sleep Med Rev. 2007 Aug;11(4):295-310. doi: 10.1016/j.smrv.2007.03.004. Epub 2007 May 11. PMID: 17498981.
- 9Nielsen T. The Stress Acceleration Hypothesis of Nightmares. Front Neurol. 2017 Jun 1;8:201. doi: 10.3389/fneur.2017.00201. PMID: 28620339; PMCID: PMC5451501.
- 10Luca, A., Luca, M., & Calandra, C. (2013). Sleep disorders and depression: brief review of the literature, case report, and nonpharmacologic interventions for depression. Clinical interventions in aging, 8, 1033–1039. https://doi.org/10.2147/CIA.S47230
- 11Don Richardson J, King L, St Cyr K, Shnaider P, Roth ML, Ketcheson F, Balderson K, Elhai JD. Depression and the relationship between sleep disturbances, nightmares, and suicidal ideation in treatment-seeking Canadian Armed Forces members and veterans. BMC Psychiatry. 2018 Jun 19;18(1):204. doi: 10.1186/s12888-018-1782-z. PMID: 29921268; PMCID: PMC6011186.
- 12Agargun MY, Besiroglu L, Cilli AS, Gulec M, Aydin A, Inci R, Selvi Y. Nightmares, suicide attempts, and melancholic features in patients with unipolar major depression. J Affect Disord. 2007 Mar;98(3):267-70. doi: 10.1016/j.jad.2006.08.005. Epub 2006 Aug 28. PMID: 16938351.
- 13Agargun MY, Kara H, Ozer OA, Selvi Y, Kiran U, Ozer B. Clinical importance of nightmare disorder in patients with dissociative disorders. Psychiatry Clin Neurosci. 2003 Dec;57(6):575-9. doi: 10.1046/j.1440-1819.2003.01169.x. PMID: 14629705.
- 14Semiz UB, Basoglu C, Ebrinc S, Cetin M. Nightmare disorder, dream anxiety, and subjective sleep quality in patients with borderline personality disorder. Psychiatry Clin Neurosci. 2008 Feb;62(1):48-55. doi: 10.1111/j.1440-1819.2007.01789.x. PMID: 18289141.
- 15Sheaves, B., Onwumere, J., Keen, N., Stahl, D., & Kuipers, E. (2015). Nightmares in Patients With Psychosis: The Relation With Sleep, Psychotic, Affective, and Cognitive Symptoms. Canadian journal of psychiatry. Revue canadienne de psychiatrie, 60(8), 354–361. https://doi.org/10.1177/070674371506000804
- 16Li, S. X., Zhang, B., Li, A. M., & Wing, Y. K. (2010). Prevalence and correlates of frequent nightmares: a community-based 2-phase study. Sleep, 33(6), 774–780. https://doi.org/10.1093/sleep/33.6.774
- 17Rek, S., Sheaves, B., & Freeman, D. (2017). Nightmares in the general population: identifying potential causal factors. Social psychiatry and psychiatric epidemiology, 52(9), 1123–1133. https://doi.org/10.1007/s00127-017-1408-7
- 18Hublin C, Kaprio J, Partinen M, Koskenvu M. Parasomnias: co-occurrence and genetics. Psychiatr Genet. 2001 Jun;11(2):65-70. doi: 10.1097/00041444-200106000-00002. PMID: 11525419.
- 19Hublin C, Kaprio J, Partinen M, Koskenvuo M. Nightmares: familial aggregation and association with psychiatric disorders in a nationwide twin cohort. Am J Med Genet. 1999 Aug 20;88(4):329-36. doi: 10.1002/(sici)1096-8628(19990820)88:4<329::aid-ajmg8>3.0.co;2-e. PMID: 10402498.
- 20Bidaki, R., Zarei, M., Khorram Toosi, A., & Hakim Shooshtari, M. (2012). A review on genetics of sleep disorders. Iranian journal of psychiatry and behavioral sciences, 6(1), 12–19.
- 21Wang, C., Shao, X., Jia, Y. et al. Nightmare experience and family relationships in healthy volunteers and nightmare disorder patients. BMC Psychiatry 19, 297 (2019). https://doi.org/10.1186/s12888-019-2299-9
- 22Farzam K, Jan A. Beta Blockers. [Updated 2020 Nov 27]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK532906/
- 23Pagel JF, Helfter P. Drug induced nightmares–an etiology based review. Hum Psychopharmacol. 2003 Jan;18(1):59-67. doi: 10.1002/hup.465. PMID: 12532316.
- 24Thompson DF, Pierce DR. Drug-induced nightmares. Ann Pharmacother. 1999 Jan;33(1):93-8. doi: 10.1345/aph.18150. PMID: 9972389.
- 25Westerlund A. Central nervous system side-effects with hydrophilic and lipophilic beta-blockers. Eur J Clin Pharmacol. 1985;28 Suppl:73-6. doi: 10.1007/BF00543714. PMID: 2865153.
- 26Wichniak, A., Wierzbicka, A., Walęcka, M., & Jernajczyk, W. (2017). Effects of Antidepressants on Sleep. Current psychiatry reports, 19(9), 63. https://doi.org/10.1007/s11920-017-0816-4
- 27Aurora, R. N., Zak, R. S., Auerbach, S. H., Casey, K. R., Chowdhuri, S., Karippot, A., Maganti, R. K., Ramar, K., Kristo, D. A., Bista, S. R., Lamm, C. I., Morgenthaler, T. I., Standards of Practice Committee, & American Academy of Sleep Medicine (2010). Best practice guide for the treatment of nightmare disorder in adults. Journal of clinical sleep medicine : JCSM : official publication of the American Academy of Sleep Medicine, 6(4), 389–401.
- 28Pétursson H. The benzodiazepine withdrawal syndrome. Addiction. 1994 Nov;89(11):1455-9. doi: 10.1111/j.1360-0443.1994.tb03743.x. PMID: 7841856.
- 29Dollander M. Etiologies de l’insomnie chez l’adulte [Etiology of adult insomnia]. Encephale. 2002 Nov-Dec;28(6 Pt 1):493-502. French. PMID: 12506261.
- 30Zisenwine T, Kaplan M, Kushnir J, Sadeh A. Nighttime fears and fantasy-reality differentiation in preschool children. Child Psychiatry Hum Dev. 2013 Feb;44(1):186-99. doi: 10.1007/s10578-012-0318-x. PMID: 22760490.
- 31Wegner DM, Wenzlaff RM, Kozak M. Dream rebound: the return of suppressed thoughts in dreams. Psychol Sci. 2004 Apr;15(4):232-6. doi: 10.1111/j.0963-7214.2004.00657.x. PMID: 15043639.
- 32Kramer M, Kinney L. Vigilance and avoidance during sleep in US Vietnam War veterans with posttraumatic stress disorder. J Nerv Ment Dis. 2003 Oct;191(10):685-7. doi: 10.1097/01.nmd.0000092179.74348.20. PMID: 14555872.
- 33Sandman, N., Valli, K., Kronholm, E., Vartiainen, E., Laatikainen, T., & Paunio, T. (2017). Nightmares as predictors of suicide: an extension study including war veterans. Scientific reports, 7, 44756. https://doi.org/10.1038/srep44756
- 34Paul, F., Schredl, M., & Alpers, G. W. (2015). Nightmares affect the experience of sleep quality but not sleep architecture: an ambulatory polysomnographic study. Borderline personality disorder and emotion dysregulation, 2, 3. https://doi.org/10.1186/s40479-014-0023-4
- 35Gieselmann, A., Ait Aoudia, M., Carr, M., Germain, A., Gorzka, R., Holzinger, B., Kleim, B., Krakow, B., Kunze, A. E., Lancee, J., Nadorff, M. R., Nielsen, T., Riemann, D., Sandahl, H., Schlarb, A. A., Schmid, C., Schredl, M., Spoormaker, V. I., Steil, R., van Schagen, A. M., … Pietrowsky, R. (2019). Aetiology and treatment of nightmare disorder: State of the art and future perspectives. Journal of sleep research, 28(4), e12820. https://doi.org/10.1111/jsr.12820
- 36Nadorff, M. R., Pearson, M. D., & Golding, S. (2016). Explaining the Relation between Nightmares and Suicide. Journal of clinical sleep medicine : JCSM : official publication of the American Academy of Sleep Medicine, 12(3), 289–290. https://doi.org/10.5664/jcsm.5564