In the aftermath of war, the most visible injuries—missing limbs, burned skin, shattered bones—often draw the greatest sympathy and attention. But a new report from army rehabilitation centers reveals another, quieter crisis: more than 55% of disabled Gaza war veterans undergoing treatment are also grappling with serious mental health issues. Beneath the scars and prosthetics, many veterans are fighting battles of the mind—struggles that can be just as debilitating as any physical wound. These struggles affect so many veterans long after the physical pain subsides.
Physical Wounds, Psychological Pain
For countless veterans, recovery has become a lifelong journey shadowed by emotional distress. Every day, they learn to navigate a new world—one where simple actions like walking, dressing, or hugging a child can become feats of determination. But behind the grit and perseverance lies a darkness often left unspoken. Many disabled veterans experience nightmares, flashbacks, anxiety, and profound sadness. The trauma isn’t erased by the end of conflict; it lingers, resurfacing in quiet moments or startling them awake at night, hallmark symptoms of persistent psychological challenges.
It’s not uncommon for the pain of a lost limb or injury to be compounded by post-traumatic stress disorder (PTSD), depression, or substance abuse. The physical and psychological wounds feed each other, deepening the cycle. Frustration with slow progress, constant hospital visits, and the pressures of adjusting to civilian life can fuel emotional pain and a deep sense of isolation, making daily life a struggle for many.
The Challenge of Holistic Healing
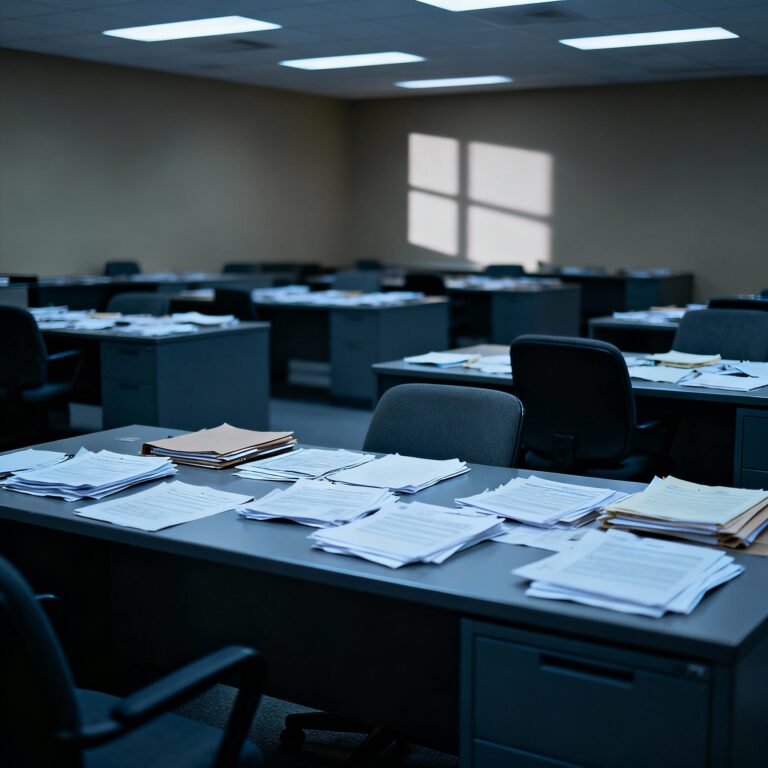
Rehabilitation centers strive to provide comprehensive care, offering cutting-edge prosthetics, physiotherapy, and medical surgeries. Yet doctors, nurses, and counselors quickly learn that no device or drug can fully mend what’s broken inside. Many veterans require ongoing therapy, counseling, and support for years after their bodies have begun healing. The emotional scars must be addressed with as much diligence as physical injuries.
The shift toward a holistic approach in army rehab facilities is a hard-won lesson about addressing psychological well-being. Mental health screenings and treatments are now cornerstones of recovery programs. Peer support groups, individual counseling, and group therapy all give veterans safe spaces to talk about their anxieties, grief, and hopes—essential for overcoming inner struggles. It’s in these rooms, sometimes more than the gym or operating table, that true healing can begin.
Families: The Hidden Front Line
War wounds rarely impact only the veterans themselves. Partners, parents, and children become caregivers, cheerleaders, and often, silent sufferers. Many family members describe the challenge of dealing with sudden mood swings, flashbacks, or withdrawal in their loved ones, all linked to inner battles. They may feel helpless or overwhelmed by their new roles, worrying constantly for the veteran’s future as emotional challenges persist.
Community and family support become crucial defenses. Specialist organizations offer workshops, group therapy, and educational sessions designed for families, helping them recognize warning signs and build resilient coping strategies. The journey toward recovery from both physical injuries and emotional scars is rarely walked alone.
Breaking the Stigma, Embracing Hope
The statistic—55% struggling with psychological issues—can feel overwhelming. But the increased recognition of this crisis is already changing lives. Every veteran who shares their story or seeks counseling sends a powerful message: You are not alone, and help is available for these challenges. Society, too, is slowly learning to recognize invisible wounds and to value mental well-being as much as physical health, working to dispel the stigma around psychological adversity.
There is still so much work left to do. Governments must invest in more accessible, ongoing support; communities need to open their arms; and families and professionals must ensure compassion drives every interaction. Healing is not only possible, but achievable—if we acknowledge the journey is both physical and deeply emotional, particularly in the battle with inner wounds.
Frequently Asked Questions –
What mental health issues are most common among disabled Gaza war veterans?
The most common issues are PTSD, depression, anxiety, substance use, and difficulty adjusting to civilian life after injury—each contributing to ongoing mental health issues.
Why is the rate of mental health issues so high among this group?
he combination of traumatic combat experiences and life-changing physical injuries creates complex, overlapping emotional struggles leading to mental health issues.
What kind of treatment do army rehab centers offer for mental health issues?
Rehab centers provide physiotherapy, medical care, counseling, therapy groups, and mental health screenings as part of a comprehensive program addressing mental health issues.
How can families help veterans recover from mental health issues?
Staying supportive, learning about mental health issues, encouraging regular counseling, and avoiding stigma can all make a big difference.
What can society do to support disabled veterans facing mental health issues?
Advocate for better funding, raise awareness about invisible wounds, and foster empathy by listening to veterans’ stories, thus supporting those facing mental health issues.