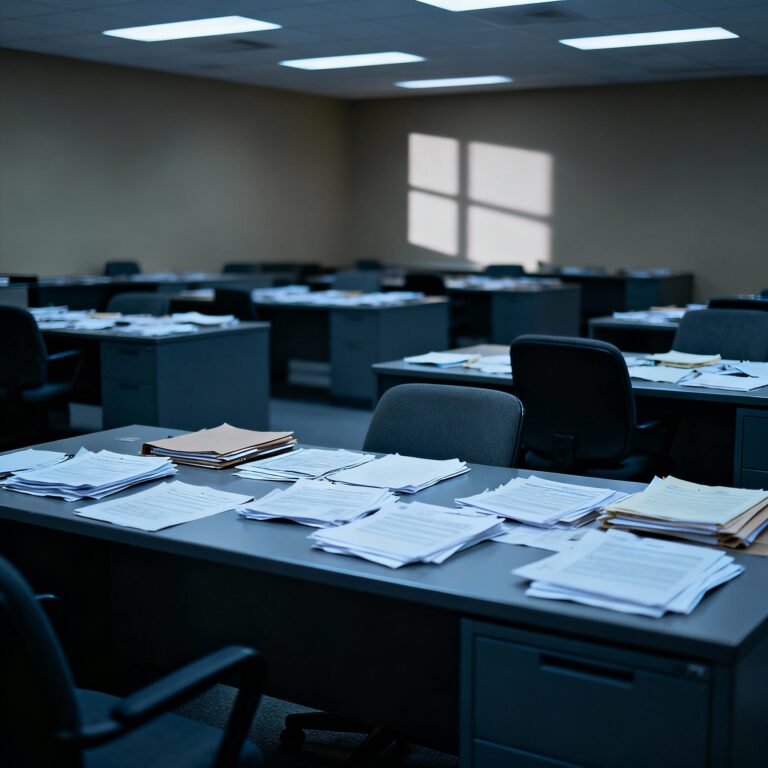
Across the United States, sweeping changes in federal policy are putting Mental Health Care accessibility at risk for millions. Recent moves to cut Medicaid funding, roll back mental health parity regulations, and restructure critical public health agencies are sparking concern among advocates, medical professionals, and affected families. These policy shifts come at a time when the nation’s Health Care system is already under tremendous strain, with demand for services consistently outpacing supply.
Rising Barriers to Mental Health Care
One of the most pressing concerns is the potential cutback in Medicaid—a lifeline for low-income individuals and families who rely on Mental Health Care. The reductions will likely result in fewer covered services, longer wait times, and increased financial strain on those seeking support. Additionally, changes to mental health parity regulations, which require insurers to treat Health Care on equal footing with physical health, threaten to deepen disparities in coverage and service quality.
Advocates warn that these federal changes will disproportionately impact vulnerable populations. Youths, communities of color, rural residents, and those with substance use disorders are expected to feel the most severe effects. With fewer resources, community clinics and crisis centers face the possibility of cutbacks or closures—directly limiting Mental Health Care options nationwide.
Agency Restructuring and Its Impact
Another major concern is the restructuring of essential agencies such as the Substance Abuse and Mental Health Services Administration (SAMHSA) and the Health Resources and Services Administration (HRSA). These institutions play a vital role in policy direction, resource allocation, and local program funding. As they undergo changes, there is uncertainty about continued support for Mental Health Care research, grants, and community services.
Mental Health Care providers fear that reduced federal oversight and funding will stifle prevention efforts, limit innovation, and create bureaucratic barriers to care. Front-line workers signal that agencies tasked with helping the most vulnerable must have stable, strong support if Health Care accessibility is to improve—not decline.
Immediate and Long-term Consequences
Experts say these federal policy changes are coming at precisely the wrong moment. The United States is facing an unprecedented rise in anxiety, depression, and suicide rates—emerging from the pandemic with heightened awareness of Mental Health Care needs but insufficient infrastructure to meet them. Limiting access could mean more people left untreated, higher rates of emergency room visits, and increased pressure on law enforcement and social service agencies.
Additionally, Mental Health Care disruptions could hinder efforts to build resilience in communities hit hardest by the opioid epidemic and economic hardship. Long-term consequences may include sharp increases in untreated mental illness, disability claims, lost productivity, and public safety challenges.
What Can Be Done?
Mental Health Care advocates are urging Congress and federal agencies to reconsider these policy changes before lasting damage is done. Suggested solutions include maintaining or increasing funding for Medicaid, protecting parity laws, and ensuring continued support for agencies like SAMHSA and HRSA. Community engagement, transparent policymaking, and data-driven reforms are all seen as critical for strengthening the Mental Health Care landscape in America.
Frequently Asked Questions –
How will federal policy changes affect Mental Health Care?
They may reduce access, funding, and insurance coverage, making it harder for millions to receive Mental Health Care.
Who is most at risk from reduced Mental Health Care accessibility?
Vulnerable groups—like low-income families, youth, rural communities, and people with substance use disorders—will be most affected.
What agencies are involved in supporting Mental Health Care?
Key agencies include SAMHSA and HRSA, both under review for restructuring that could impact research, funding, and services.
What actions can improve Mental Health Care accessibility?
Maintaining Medicaid funding, enforcing parity laws, supporting federal agencies, and engaging communities in decision-making are crucial.