Drunkorexia is a disorder that involves the traits of anorexia or bulimia combined with alcohol abuse. This term is usually used to indicate the utilization of extreme weight control methods in order to compensate for planned binge drinking.
What Is Drunkorexia?
Drunkorexia [mfn] Paciorek, Kamila & Górski, Michał & Grajek, Mateusz & Ciechowska, Karolina & Polaniak, Renata. (2021). Drunkorexia – knowledge review. Psychiatria Polska. 1-11. 10.12740/PP/OnlineFirst/134748. [/mfn] is the practice of starving oneself during the day in order to make room for the calorie intake associated with planned alcohol consumption. Drunkorexia is a condition characterized by substituting meals with alcohol, excess exercising to compensate for alcohol consumption, and purging food as a means of substituting calorie intake from alcohol. The process involves a combination of starvation, binge drinking, and binge eating during the night [mfn] Hunt, T. K., & Forbush, K. T. (2016). Is “drunkorexia” an eating disorder, substance use disorder, or both?. Eating behaviors, 22, 40–45. https://doi.org/10.1016/j.eatbeh.2016.03.034 [/mfn]. Binge eating disorders can involve bulimia nervosa or anorexia nervosa.
“The term Drunkorexia has been used by the popular media to denote the use of extreme weight-control behaviours to compensate for planned binge drinking.” explains a 2013 study [mfn] Knight, A., Simpson, S. Drunkorexia: an empirical investigation of disordered eating in direct response to saving calories for alcohol use amongst Australian female university students. J Eat Disord 1, P6 (2013). https://doi.org/10.1186/2050-2974-1-S1-P6 [/mfn] . This act involves substituting food with alcohol, which can be damaging to the body since it can miss out on important nutrients. It can be dangerous and is associated with depression, suicidal tendencies, legal issues, and violence.
Drinking in a state of malnutrition can predispose individuals to a higher rate of blackouts, alcohol poisoning, alcohol-related injury, violence, and illness. The ethanol in alcohol reaches the blood system faster and raises one’s blood alcohol content at a dangerous speed. This can put the person in an alcohol-related brain injury. People with this condition often display a pattern of distorted self-perception congruent with unrealistic standards of body image. They fall prey to peer pressure to assimilate the norms of social drinking. It can also be a coping mechanism for depression and anxiety.
Understanding Drunkorexia
Researchers [mfn] Lupi, M., Martinotti, G., & Di Giannantonio, M. (2017). Drunkorexia: an emerging trend in young adults. Eating and weight disorders : EWD, 22(4), 619–622. https://doi.org/10.1007/s40519-017-0429-2 [/mfn] have found that drunkorexia is prevalent and common among young adults. There are several studies [mfn] Choquette, E. M., Rancourt, D., & Kevin Thompson, J. (2018). From fad to FAD: A theoretical formulation and proposed name change for “drunkorexia” to food and alcohol disturbance (FAD). The International journal of eating disorders, 51(8), 831–834. https://doi.org/10.1002/eat.22926 [/mfn] that suggest that up to a third of college students say they reduce the amount of food they eat before drinking in order to compensate for the calories in alcohol. Studies [mfn] Poobalan, A. S., Aucott, L. S., Clarke, A., & Smith, W. C. (2014). Diet behaviour among young people in transition to adulthood (18-25 year olds): a mixed method study. Health psychology and behavioral medicine, 2(1), 909–928. https://doi.org/10.1080/21642850.2014.931232 [/mfn] suggest that 30 percent of women between the ages of 18 and 23 diets so they can drink.
It is more prevalent in college-aged women than in men. The perpetual necessity of having alcohol in order to have a good time has led a lot of people to overindulge in substances. College-aged people are at higher risk of developing this condition. Eating a full meal and then consuming several rounds of drinks at the bar can exceed the number of calories one should have every day. This allows them to skip meals in order to compensate for their daily calorie intake.
Some research [mfn] Osborne, V., Sher, K., & Winograd, R. (2011). Disordered eating patterns and alcohol misuse in college students: Evidence for “drunkorexia”? Comprehensive Psychiatry, 52(6), e12. https://doi.org/10.1016/j.comppsych.2011.04.038 [/mfn] found that the individuals who engage in this combination of binge drinking and self-imposed malnutrition tend to avoid weight gain from alcohol, to save money from purchasing alcohol, and to facilitate alcohol intoxication. A 2009 study [mfn] Giles, S. M., Champion, H., Sutfin, E. L., McCoy, T. P., & Wagoner, K. (2009). Calorie restriction on drinking days: An examination of drinking consequences among college students. Journal of American College Health, 57(6), 603-610. https://doi.org/10.3200/jach.57.6.603-610 [/mfn] found that college students who restricted calories before drinking were more likely to get drunk. Women who avoided food before drinking reported memory loss, engaged in unprotected sex, and were at a risk for being injured or sexually assaulted. Men who restricted themselves engaged in more physical aggression. Another research [mfn] Eisenberg, M. H., Johnson, C. C., & Zucker, A. N. (2018). Starving for a drink: Sexual objectification is associated with food-restricted alcohol consumption among college women, but not among men. Women & health, 58(2), 175–187. https://doi.org/10.1080/03630242.2017.1292342 [/mfn] found that women who experience objectification are more likely to engage in this behavior.
Symptoms Of Drunkorexia
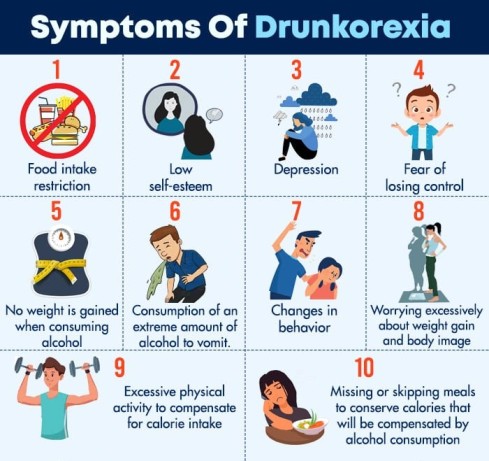
The primary symptom of this condition is avoiding food intake in order to consume alcohol. Other symptoms include:
- Food intake restriction
- Excessive physical activity to compensate for calorie intake
- Counting daily calorie intake in order to ensure that no weight is gained when consuming alcohol
- Missing or skipping meals to conserve calories that will be compensated by alcohol consumption
- Consumption of an extreme amount of alcohol to vomit previously ingested food
- Feeling guilty while drinking because of consuming the calories
- Being sick during the drinking session and then continuing to drink more even after purging to maintain the high levels of intoxication
- In a drinking session on an empty stomach, they are likely to get drunk faster. This means they are more likely to fall ill and vomit. In case, this happens on a regular basis, it can cause tooth decay.
- Changes in behavior
- Worrying excessively about weight gain and body image
- Low self-esteem
- Depression
- Poor coping skills
- Fear of losing control
Risks Of Drunkorexia

The combination of eating disorders and binge drinking can pose a lot of risks for the individual’s physical, mental, and emotional health. They are as follows:
- Drinking on an empty stomach may lead to overconsumption and an unexpected degree of intoxication that interferes with judgement and increases the risk of physical injury.
- Metabolizing alcohol requires certain nutrients [mfn] Lieber CS. The influence of alcohol on nutritional status. Nutr Rev. 1988 Jul;46(7):241-54. doi: 10.1111/j.1753-4887.1988.tb05443.x. PMID: 3045703. [/mfn] . Restricting food intake decreases the availability of necessary nutrients. This tends to increase the risk of nutrient deficiencies.
- Drinking alcohol after working out tends to inhibit protein synthesis and muscle repair. This, however, tends to slow down the recovery process and minimize potential improvements in fitness.
- Alcohol consumption limits the decision making [mfn] Goudriaan, A. E., Grekin, E. R., & Sher, K. J. (2007). Decision making and binge drinking: a longitudinal study. Alcoholism, clinical and experimental research, 31(6), 928–938. https://doi.org/10.1111/j.1530-0277.2007.00378.x [/mfn] capabilities of an individual that may lead to unhealthy eating behaviors.
Read More About Alcoholism Here
Why Drunkorexia Damaging
Drunkorexia occurs when the individual resorts to alcohol consumption as a substitute for food intake. Food avoidance is done as a replacement for calorie intake associated with alcohol intake[mfn] Barry, A. E., & Piazza-Gardner, A. K. (2012). Drunkorexia: Understanding the Co-occurrence of alcohol consumption and eating/Exercise weight management behaviors. Journal of American College Health, 60(3), 236-243. https://doi.org/10.1080/07448481.2011.587487 [/mfn]. The damage is caused due to restricting food intake since this tends to deplete the body of essential vitamins and minerals. Even though pre-drinking starvation is a tactic, it can still lead to weight gain. Alcohol reduces the fat that our body burns for energy. No matter how little a person eats before the drinking session, it can still affect the scales the next morning.
Drinking on an empty stomach can make a person drunk quicker than usual which makes them more likely to get sick as the body struggles to process the alcohol.
The most common side effects of drunkorexia are as follows:

- Impaired coordination
- Stomach pain
- Slowed brain function
- Dizziness
- Mental confusion
- Slurred speech
- Showing zero interest in things
- Mood swings
- Constipation
- High blood pressure
- Liver disease
- Cancer
- Obesity
- Anemia
- Acne-prone skin
- Brittle hair and nails
- Abdominal bloating
- Cardiac problems
- Diabetes
- Dementia
- Hypoglycemia
- Driving under the influence (DUI)
Read More About Obesity Here
Diagnosis For Drunkorexia
The Diagnostic and Statistical Manual of Mental Disorders (DSM-5) does not recognize this as a formal eating disorder or an alcohol abuse disorder. However, it is a widely recognized condition by mental healthcare and the eating disorder community. According to a 2019 study [mfn] Thompson-Memmer, C., Glassman, T., & Diehr, A. (2019). Drunkorexia: A new term and diagnostic criteria. Journal of American college health : J of ACH, 67(7), 620–626. https://doi.org/10.1080/07448481.2018.1500470 [/mfn] , “While the term drunkorexia has been used in both academic articles and popular culture, issues persist with respect to diagnosing and treating this condition.”
If an individual is not receiving calories from food intake but from alcohol consumption, there are a lot of empty calories in the body that can put the individual at risk of dehydration and vitamin depletion. In case the person is experiencing symptoms, it is important to seek medical attention. The doctor may do a physical exam to rule out any underlying conditions that have affected the patient. After evaluation, the doctor will refer them to a psychiatrist. The psychiatrist will ask questions regarding their food and alcohol intake. They will also take into account their personal and medical histories in order to diagnose this disorder.
After diagnosis, the doctor will devise a treatment plan that is designed to comfort the symptoms of the condition.
Treatment For Drunkorexia
One study [mfn] Powell‐jones, A., & Simpson, S. (2020). Drunkorexia: An investigation of symptomatology and early maladaptive schemas within a female, young adult Australian population. Australian Psychologist, 55(5), 559-571. https://doi.org/10.1111/ap.12462 [/mfn] suggested that almost 60 percent of undergraduate students have drunkorexia tendencies. So it is crucial that these individuals receive treatment. Since alcoholism and eating disorders are a form of addiction it requires a dual diagnosis treatment. The treatment method is a combination of medication and therapy.
1. Cognitive Behavioral Therapy (CBT)
This therapy involves understanding the thoughts and patterns that govern negative behavior. After understanding, these are then replaced with positive ones in order to attain the desired outcome. The doctor may also help the patient to develop coping strategies to ease or minimize the symptoms of the condition.
According to research, CBT is regarded as the leading proven treatment for all eating disorders, such as anorexia nervosa, bulimia nervosa and eating disorders not otherwise specified, like drunkorexia. In fact, an enhanced version of CBT has been found to be more beneficial and potent. “Enhanced cognitive behavior therapy (CBT‐E) is a transdiagnostic treatment suitable for the full range of eating disorders (EDs),” suggests a recent 2020 study [mfn] de Jong, M., Spinhoven, P., Korrelboom, K., Deen, M., van der Meer, I., Danner, U. N., van der Schuur, S., Schoorl, M., & Hoek, H. W. (2020). Effectiveness of enhanced cognitive behavior therapy for eating disorders: A randomized controlled trial. The International journal of eating disorders, 53(5), 447–457. https://doi.org/10.1002/eat.23239 [/mfn] .
Read More About Effectiveness Of Cognitive Behavioral Theory Here
2. Group Therapy
This therapy [mfn] Halmi K. A. (2005). The multimodal treatment of eating disorders. World psychiatry : official journal of the World Psychiatric Association (WPA), 4(2), 69–73. [/mfn] involves a group of people addressing the concerns to a team of therapists. They share their concerns regarding their eating habits and alcoholism and how they feel about it. The therapists help them to develop coping mechanisms as a group in order to ease the symptoms of the condition.
Research [mfn] Lázaro, L., Font, E., Moreno, E., Calvo, R., Vila, M., Andrés-Perpiñá, S., Canalda, G., Martínez, E., & Castro-Fornieles, J. (2011). Effectiveness of self-esteem and social skills group therapy in adolescent eating disorder patients attending a day hospital treatment programme. European eating disorders review : the journal of the Eating Disorders Association, 19(5), 398–406. https://doi.org/10.1002/erv.1054 [/mfn] has found that group therapy targeted at improving self-esteem & social skills among sufferers with eating disorders can help to manage symptoms and core features. One 2017 study [mfn] Grenon, R., Schwartze, D., Hammond, N., Ivanova, I., Mcquaid, N., Proulx, G., & Tasca, G. A. (2017). Group psychotherapy for eating disorders: A meta-analysis. The International journal of eating disorders, 50(9), 997–1013. https://doi.org/10.1002/eat.22744 [/mfn] revealed that group psychotherapy is substantially more effective and helps in improving abstinence rates and reducing the frequency of binge eating/drinking and/or purging.
Read More About Group Therapy Here
3. Medications
Medications may be prescribed to the patient to ease the symptoms. However, there is no medicinal cure for alcoholism. There are medications that can make drinking less enjoyable so you don’t intake as much. They include Disulfiram [mfn] Center for Substance Abuse Treatment. Incorporating Alcohol Pharmacotherapies Into Medical Practice. Rockville (MD): Substance Abuse and Mental Health Services Administration (US); 2009. (Treatment Improvement Protocol (TIP) Series, No. 49.) Chapter 3—Disulfiram. Available from: https://www.ncbi.nlm.nih.gov/books/NBK64036/ [/mfn] (it makes them feel sick or throw up), Acamprosate [mfn] Kalk, N. J., & Lingford-Hughes, A. R. (2014). The clinical pharmacology of acamprosate. British journal of clinical pharmacology, 77(2), 315–323. https://doi.org/10.1111/bcp.12070 [/mfn] (it helps with the cravings), and Naltrexone (this blocks the high they get from drinking).
The doctor will assess the condition and prescribe medications accordingly. As per a 2014 study [mfn] Skinner, M. D., Lahmek, P., Pham, H., & Aubin, H. J. (2014). Disulfiram efficacy in the treatment of alcohol dependence: a meta-analysis. PloS one, 9(2), e87366. https://doi.org/10.1371/journal.pone.0087366 [/mfn] , disulfiram is “a safe and efficacious treatment compared to other abstinence supportive pharmacological treatments” for problems of alcohol abuse or dependence. Another 2012 study [mfn] Witkiewitz, K., Saville, K., & Hamreus, K. (2012). Acamprosate for treatment of alcohol dependence: mechanisms, efficacy, and clinical utility. Therapeutics and clinical risk management, 8, 45–53. https://doi.org/10.2147/TCRM.S23184 [/mfn] shows that acamprosate is an effective and well tolerated treatment for alcohol dependence, while another 2017 study [mfn] Canidate, S. S., Carnaby, G. D., Cook, C. L., & Cook, R. L. (2017). A Systematic Review of Naltrexone for Attenuating Alcohol Consumption in Women with Alcohol Use Disorders. Alcoholism, clinical and experimental research, 41(3), 466–472. https://doi.org/10.1111/acer.13313 [/mfn] found that “naltrexone may lead to modest reductions in quantity of drinking and time to relapse.”
4. Nutrition and Diet
It is important to follow a strict diet in order to ensure that your body receives all the necessary nutrition to be healthy. Due to skipping meals, the body can be negatively affected. Hence, it is essential to follow a diet. Practicing meal planning and developing a healthy eating pattern can go a long way to lead a normal and healthy life.
5. Finding A Balanced Lifestyle
Studies [mfn] Wu, X. Y., Yin, W. Q., Sun, H. W., Yang, S. X., Li, X. Y., & Liu, H. Q. (2019). The association between disordered eating and health-related quality of life among children and adolescents: A systematic review of population-based studies. PloS one, 14(10), e0222777. https://doi.org/10.1371/journal.pone.0222777 [/mfn] show that there is a strong association between eating disorders and health-related quality of life (HRQOL). A person suffering from drunkorexia must resort to a healthy balance of lifestyle in order to ease the symptoms. This means that there have to be certain lifestyle changes. They can include:
- Practicing eating moderate portions throughout the day
- Knowing the limits to your alcohol intake
- Choosing drinks that have lower calories in order to avoid the anxiety associated with the calorie intake
- Exercising regularly in order to ensure heart health and stress management
- Seeking support from family members or group therapy
Recovery From Drunkorexia
A dual diagnosis can be scary and it is possible to manage and treat the symptoms. Treatment and recovery from drunkorexia is a gradual process so it is important to be patient. With therapy and medications, it is possible to lead a healthy lifestyle free from binge drinking and eating.
Drunkorexia At A Glance
- Drunkorexia is a disorder that involves the traits of anorexia or bulimia combined with alcohol abuse.
- The combination of eating disorders and binge drinking can pose a lot of risks for the individual’s physical, mental, and emotional health.
- Researchers have found that drunkorexia is prevalent and common among young adults.
- The primary symptom of this condition is avoiding food intake in order to consume alcohol.
- Drunkorexia occurs when the individual resorts to alcohol consumption as a substitute for food intake.
- A dual diagnosis can be scary and it is possible to manage and treat the symptoms.







Leave a Reply