Obesity is a complicated medical condition related to abnormal and excessive fat buildup in the body that leads to various adverse effects on a person’s well-being. It not only affects our physical health but is also associated with several psychiatric disorders as well.
What Is Obesity?
Obesity refers to a complex physical health condition where excessive body fat accumulates in the body and can lead to severe negative health effects. A person is believed to be obese when their BMI (body mass index) is above 30 kg/m2 or more. BMI measures a person’s body size based on their height and weight. The condition is a common multifactorial disease that is found in about one third of the global population [mfn] Chooi, Y. C., Ding, C., & Magkos, F. (2019). The epidemiology of obesity. Metabolism: clinical and experimental, 92, 6–10. https://doi.org/10.1016/j.metabol.2018.09.005 [/mfn] .
According to studies [mfn] Panuganti KK, Nguyen M, Kshirsagar RK. Obesity. [Updated 2021 Aug 11]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK459357/ [/mfn] , “Obesity is the excessive or abnormal accumulation of fat or adipose tissue in the body that may impair health.” It is a serious medical concern and not simply an issue about one’s physical appearance. This disorder is associated with and can cause other diseases, such as diabetes [mfn] Leitner, D. R., Frühbeck, G., Yumuk, V., Schindler, K., Micic, D., Woodward, E., & Toplak, H. (2017). Obesity and Type 2 Diabetes: Two Diseases with a Need for Combined Treatment Strategies – EASO Can Lead the Way. Obesity facts, 10(5), 483–492. https://doi.org/10.1159/000480525 [/mfn] , heart disease [mfn] Mandviwala, T., Khalid, U., & Deswal, A. (2016). Obesity and Cardiovascular Disease: a Risk Factor or a Risk Marker?. Current atherosclerosis reports, 18(5), 21. https://doi.org/10.1007/s11883-016-0575-4 [/mfn] , cancer [mfn] De Pergola, G., & Silvestris, F. (2013). Obesity as a major risk factor for cancer. Journal of obesity, 2013, 291546. https://doi.org/10.1155/2013/291546 [/mfn] and high blood pressure. It is also related to various mental health problems such as anxiety and depression [mfn] Rajan, T. M., & Menon, V. (2017). Psychiatric disorders and obesity: A review of association studies. Journal of postgraduate medicine, 63(3), 182–190. https://doi.org/10.4103/jpgm.JPGM_712_16 [/mfn] .
There are several reasons why a person can become obese such as genetic, environmental and physiological factors. Other contributing factors that can trigger this health condition includes age, sex, ethnicity, diet, overeating, physical activity etc.The condition may develop due to multiple complex reasons, but mostly occurs when people consume more calories than they burn. However, it is not just about overeating and can be extremely difficult to manage only through dieting.
Understanding Obesity
Researchers [mfn] Hruby, A., & Hu, F. B. (2015). The Epidemiology of Obesity: A Big Picture. PharmacoEconomics, 33(7), 673–689. https://doi.org/10.1007/s40273-014-0243-x [/mfn] explain that “Obesity is typically defined quite simply as excess body weight for height, but this simple definition belies an etiologically complex phenotype primarily associated with excess adiposity, or body fatness, that can manifest metabolically and not just in terms of body size.” People with this health condition are more likely to develop several chronic and comorbid diseases which often disrupt their daily lives as well as increase the mortality risks.
A 2017 study [mfn] Razzoli, M., Pearson, C., Crow, S., & Bartolomucci, A. (2017). Stress, overeating, and obesity: Insights from human studies and preclinical models. Neuroscience and biobehavioral reviews, 76(Pt A), 154–162. https://doi.org/10.1016/j.neubiorev.2017.01.026 [/mfn] explains that being obese involves overeating that leads to consuming more calories than what is needed to maintain the ideal body weight. Several studies [mfn] Iqbal A, Rehman A. Binge Eating Disorder. [Updated 2021 Jul 25]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK551700/ [/mfn] define overeating as an eating disorder that is a type of mental illness related to abnormal or disturbed eating habits [mfn] National Collaborating Centre for Mental Health (UK). Eating Disorders: Core Interventions in the Treatment and Management of Anorexia Nervosa, Bulimia Nervosa and Related Eating Disorders. Leicester (UK): British Psychological Society (UK); 2004. (NICE Clinical Guidelines, No. 9.) Available from: https://www.ncbi.nlm.nih.gov/books/NBK49304/ [/mfn] . According to this concept, obesity can also be considered as a form of psychological dysfunction.
A 2018 research paper [mfn] da Luz, F. Q., Hay, P., Touyz, S., & Sainsbury, A. (2018). Obesity with Comorbid Eating Disorders: Associated Health Risks and Treatment Approaches. Nutrients, 10(7), 829. https://doi.org/10.3390/nu10070829 [/mfn] claims that obese people are more likely to develop certain symptoms of eating disorders than others. Thus, being obese can be a contributing factor in developing a psychological condition. However, it should be noted that the disease is not similar to being overweight, it involves extreme accumulation of body fat which is considered unhealthy for a person’s height.
A 2019 research paper [mfn] Inoue, Y., Qin, B., Poti, J., Sokol, R., & Gordon-Larsen, P. (2018). Epidemiology of Obesity in Adults: Latest Trends. Current obesity reports, 7(4), 276–288. https://doi.org/10.1007/s13679-018-0317-8 [/mfn] estimated that the worldwide prevalence of obesity was 12% in 2015. It is associated with a broad range of chronic health diseases [mfn] Pi-Sunyer X. (2009). The medical risks of obesity. Postgraduate medicine, 121(6), 21–33. https://doi.org/10.3810/pgm.2009.11.2074 [/mfn] , such as:
- Type 2 diabetes
- Cancer
- Cardiovascular diseases
- High blood pressure
- Stroke
- Hypertension
- Sleep apnea
- Kidney diseases
Along with certain physical health conditions, it is believed to be associated with a number of psychological and psycho-social disorders. A 2014 study [mfn] Assari S. (2014). The link between mental health and obesity: role of individual and contextual factors. International journal of preventive medicine, 5(3), 247–249. [/mfn] suggested that people with this disease often experience mild to extreme social humiliation and self-criticism that eventually take a toll on their mental well-being.
Obesity And Mental Health
The association between obesity and psychological health varies from person to person. The disease is interconnected with mental health in various significant ways. A 2013 research [mfn] Yau, Y. H., & Potenza, M. N. (2013). Stress and eating behaviors. Minerva endocrinologica, 38(3), 255–267. [/mfn] claims that psychological distress develops certain abnormal eating habits. As many people use food as a coping mechanism to deal with stress, it can lead to overeating, extreme weight gain and eventually obesity. Studies [mfn] Arab, A., Mehrabani, S., Moradi, S., & Amani, R. (2019). The association between diet and mood: A systematic review of current literature. Psychiatry research, 271, 428–437. https://doi.org/10.1016/j.psychres.2018.12.014 [/mfn] have found that our brain health and the food we eat are closely associated with each other.
It is also believed that the medicines used for treating mental health issues have a variety of side effects, including excessive weight gain. A 2010 study [mfn] Shrivastava, A., & Johnston, M. E. (2010). Weight-gain in psychiatric treatment: risks, implications, and strategies for prevention and management. Mens sana monographs, 8(1), 53–68. https://doi.org/10.4103/0973-1229.58819 [/mfn] reveals, “Many patients suffering from mental disorders, when exposed to psychotropic medications, gain significant weight with or without other side-effects.” This study suggests that psychiatric medication often increases appetite and causes extreme lethargy that hugely contributes to uncontrollable weight gain and other related conditions.
Similar to other psychiatric disorders, it consists of certain dysfunctions [mfn] Gadde, K. M., Martin, C. K., Berthoud, H. R., & Heymsfield, S. B. (2018). Obesity: Pathophysiology and Management. Journal of the American College of Cardiology, 71(1), 69–84. https://doi.org/10.1016/j.jacc.2017.11.011 [/mfn] related to genetics, physiology, anatomy, and other environmental factors. All these impairments prevent our brain from properly regulating our behavior. This leads to the brain failing to decide whether to eat because of satiety, hunger, or any other reasons. Thus, obesity is proven to be associated with psychiatric disorders.
Additionally, many obese people suffer from low self-esteem, due to which they hesitate to participate in any positive activities. Research [mfn] Puhl, R. M., & Heuer, C. A. (2010). Obesity stigma: important considerations for public health. American journal of public health, 100(6), 1019–1028. https://doi.org/10.2105/AJPH.2009.159491 [/mfn] shows that such individuals tend to experience extreme judgment and social stigma that leads to severe self-criticism and self-hate. These conditions make them extremely vulnerable and self-conscious, followed by numerous psychological consequences.
Psychological Factors That Influence Obesity
A number of studies [mfn] Jang, H. J., Kim, B. S., Won, C. W., Kim, S. Y., & Seo, M. W. (2020). The Relationship between Psychological Factors and Weight Gain. Korean journal of family medicine, 41(6), 381–368. https://doi.org/10.4082/kjfm.19.0049 [/mfn] have found that several psychological factors play a pivotal role in the process of abnormal weight gain. Some mental conditions trigger disordered eating habits & cause excessive body fat build-up. Here are some of the most significant psychological factors that influence weight gain:
- Lower self-esteem [mfn] French, S. A., Story, M., & Perry, C. L. (1995). Self-esteem and obesity in children and adolescents: a literature review. Obesity research, 3(5), 479–490. https://doi.org/10.1002/j.1550-8528.1995.tb00179.x [/mfn]
- Poor emotional management skill
- Avoidance of emotions [mfn] Lillis, J., & Wing, R. R. (2015). The role of avoidance-based coping in the psychosocial functioning of weight loss treatment-seeking adults. Obesity science & practice, 1(1), 59–64. https://doi.org/10.1002/osp4.1 [/mfn]
- Self-doubt or self-criticism [mfn] Duarte, C., Matos, M., Stubbs, R. J., Gale, C., Morris, L., Gouveia, J. P., & Gilbert, P. (2017). The Impact of Shame, Self-Criticism and Social Rank on Eating Behaviours in Overweight and Obese Women Participating in a Weight Management Programme. PloS one, 12(1), e0167571. https://doi.org/10.1371/journal.pone.0167571 [/mfn]
- Negative self talk
- Negative thinking pattern
- Body image dissatisfaction [mfn] Makara-Studzińska, M., & Zaborska, A. (2009). Otyłość a obraz własnego ciała [Obesity and body image]. Psychiatria polska, 43(1), 109–114. [/mfn]
- Lack of self-confidence
- Binge eating habits [mfn] Burrows, T., Skinner, J., McKenna, R., & Rollo, M. (2017). Food Addiction, Binge Eating Disorder, and Obesity: Is There a Relationship?. Behavioral sciences (Basel, Switzerland), 7(3), 54. https://doi.org/10.3390/bs7030054 [/mfn]
- Negative core beliefs
Read More About Body Image Here
Psychological Disorders Associated With Obesity
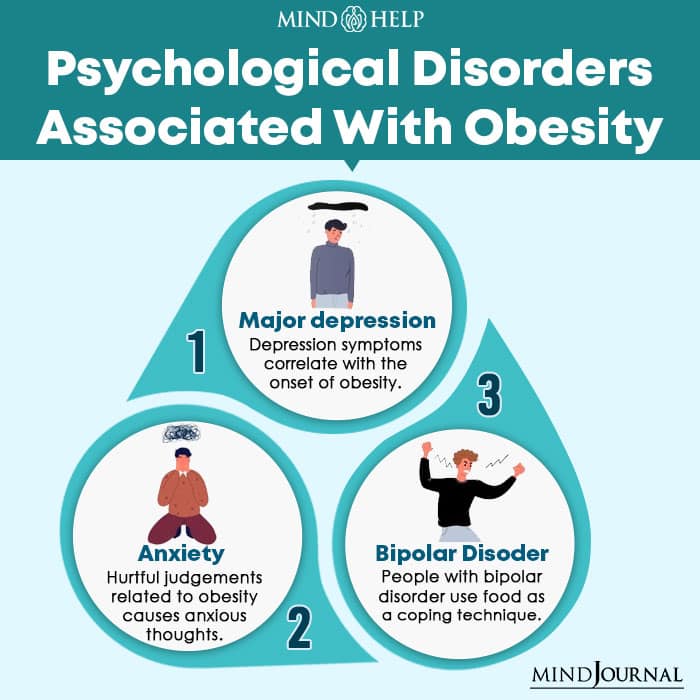
A 2007 study [mfn] Simon, G. E., Von Korff, M., Saunders, K., Miglioretti, D. L., Crane, P. K., van Belle, G., & Kessler, R. C. (2006). Association between obesity and psychiatric disorders in the US adult population. Archives of general psychiatry, 63(7), 824–830. https://doi.org/10.1001/archpsyc.63.7.824 [/mfn] suggests that obesity is interlinked with a number of chronic mental illnesses that include:
1. Major depression
Depression [mfn] Chand SP, Arif H. Depression. [Updated 2021 Jul 26]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430847/ [/mfn] refers to a kind of mood disorder that involves different symptoms, such as sadness, hopelessness, appetite changes, loss of interest, negative feelings, weight gain, etc. Studies [mfn] Needham, B. L., Epel, E. S., Adler, N. E., & Kiefe, C. (2010). Trajectories of change in obesity and symptoms of depression: the CARDIA study. American journal of public health, 100(6), 1040–1046. https://doi.org/10.2105/AJPH.2009.172809 [/mfn] have shown that depression symptoms correlate with the onset of obesity and vice-versa. That’s why depression patients, especially adolescent females [mfn] Simon, G. E., Ludman, E. J., Linde, J. A., Operskalski, B. H., Ichikawa, L., Rohde, P., Finch, E. A., & Jeffery, R. W. (2008). Association between obesity and depression in middle-aged women. General hospital psychiatry, 30(1), 32–39. https://doi.org/10.1016/j.genhosppsych.2007.09.001 [/mfn] , are more likely to be diagnosed with obesity.
A person with depression mostly develops overeating habits in order to deal with their negative feelings. Research [mfn] Targum, S. D., & Fava, M. (2011). Fatigue as a residual symptom of depression. Innovations in clinical neuroscience, 8(10), 40–43. [/mfn] explains that depression can make an individual extremely lethargic and the lack of physical activity eventually leads to weight gain. Obese people often find it very difficult to deal with their health condition that later turns into major depression.
2. Anxiety
Anxiety is considered a psychological disorder related to a feeling of stress, worry, fear, and restlessness. A 2011 study [mfn] Lykouras, L., & Michopoulos, J. (2011). Anxiety disorders and obesity. Psychiatrike = Psychiatriki, 22(4), 307–313. [/mfn] explains that obesity causes different types of anxiety disorders and other related symptoms. Due to their abnormal body weight, most obese people experience social stigma and hurtful judgments which leads to anxious thoughts. Anxiety [mfn] Blanco, C., Rubio, J., Wall, M., Wang, S., Jiu, C. J., & Kendler, K. S. (2014). Risk factors for anxiety disorders: common and specific effects in a national sample. Depression and anxiety, 31(9), 756–764. https://doi.org/10.1002/da.22247 [/mfn] and obesity also include certain similar risk factors, such as sensitivity to criticism and childhood trauma.
3. Bipolar disorder
Bipolar disorder [mfn] Jain A, Mitra P. Bipolar Affective Disorder. [Updated 2021 May 18]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK558998/ [/mfn] refers to a kind of manic depression that involves extreme mood swings and emotional outbursts. Similar to other mental conditions, bipolar disorder patients also use food as a coping technique [mfn] McElroy, S. L., & Keck, P. E., Jr (2012). Obesity in bipolar disorder: an overview. Current psychiatry reports, 14(6), 650–658. https://doi.org/10.1007/s11920-012-0313-8 [/mfn] for stress. Research [mfn] Fiedorowicz, J. G., Miller, D. D., Bishop, J. R., Calarge, C. A., Ellingrod, V. L., & Haynes, W. G. (2012). Systematic Review and Meta-analysis of Pharmacological Interventions for Weight Gain from Antipsychotics and Mood Stabilizers. Current psychiatry reviews, 8(1), 25–36. https://doi.org/10.2174/157340012798994867 [/mfn] shows that the mood stabilizers prescribed for this mental illness may have some side effects, including appetite changes and weight gain. Obese people with bipolar disorder tend to have depression symptoms, suicidal thoughts, and more manic episodes.
Read More About Bipolar Disorder Here
Psycho-Social Effects Of Obesity
Along with a few psychological consequences, obesity is related to several psycho-social effects as well. People with obesity experience some mild to severe psycho-social effects that may later result in mental health issues. The following are some of the psycho-social effects of this condition:
1. Discrimination
It is one of the primary effects that obese people suffer from because of their abnormal body weight. A recent 2020 study [mfn] Fulton M, Srinivasan VN. Obesity, Stigma And Discrimination. [Updated 2021 Mar 16]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK554571/ [/mfn] suggests that most obese adults experience discrimination in different social situations based on their body structure. They may face difficulties in pursuing education, experience humiliation at the workplace, or become the victims of bullying. Women with this disorder may face problems in dating and romantic relationships.
Read More About Discrimination Here
2. Social stigma
Experiencing social stigma is another psycho-social effect of being overweight. Studies [mfn] Wimalawansa S. J. (2014). Stigma of obesity: A major barrier to overcome. Journal of clinical & translational endocrinology, 1(3), 73–76. https://doi.org/10.1016/j.jcte.2014.06.001 [/mfn] have shown that it can be extremely damaging for obese people as it often makes them suffer from lower self-esteem. It makes them feel negative about themselves that leads to them engaging in various harmful stereotypes.
3. Low self-esteem
A 2010 study [mfn] Perrin, E. M., Boone-Heinonen, J., Field, A. E., Coyne-Beasley, T., & Gordon-Larsen, P. (2010). Perception of overweight and self-esteem during adolescence. The International journal of eating disorders, 43(5), 447–454. https://doi.org/10.1002/eat.20710 [/mfn] claims that having an abnormal body weight and experiencing lower self-esteem go hand in hand. Obese people’s weak self-esteem gradually turns into a strong feeling of shame about their body structure. Children with this disease may face bullying in school by their peers that may affect their academic performance.
According to research [mfn] Sarwer, D. B., & Polonsky, H. M. (2016). The Psychosocial Burden of Obesity. Endocrinology and metabolism clinics of North America, 45(3), 677–688. https://doi.org/10.1016/j.ecl.2016.04.016 [/mfn] , there are some other psychosocial effects of obesity that include:
- Poor life quality
- Poor body image
- Sexual abuse
- Physical abuse
- Emotional neglect
Coping With Mental Effects Of Obesity

Obesity is a multifactorial physiological disease related to excessive weight gain that has several psychological consequences. Here are some beneficial ways through which one can cope with the mental effects of obesity:
- Maintain a healthy diet [mfn] Smethers, A. D., & Rolls, B. J. (2018). Dietary Management of Obesity: Cornerstones of Healthy Eating Patterns. The Medical clinics of North America, 102(1), 107–124. https://doi.org/10.1016/j.mcna.2017.08.009 [/mfn] and limit your regular calorie intake. You can consult with a healthcare professional as they can recommend the most beneficial diet plan according to your personal details.
- Research [mfn] Makris, A., & Foster, G. D. (2011). Dietary approaches to the treatment of obesity. The Psychiatric clinics of North America, 34(4), 813–827. https://doi.org/10.1016/j.psc.2011.08.004 [/mfn] says that adding fresh fruits and vegetables, whole grains, protein and fat-free dairy to one’s regular diet can have numerous benefits for obese people.
- Avoid consuming oily, unhygienic, and processed foods as these can vigorously increase your weight [mfn] Poti, J. M., Braga, B., & Qin, B. (2017). Ultra-processed Food Intake and Obesity: What Really Matters for Health-Processing or Nutrient Content?. Current obesity reports, 6(4), 420–431. https://doi.org/10.1007/s13679-017-0285-4 [/mfn] .
- Maintain a proper sleep pattern and practice good sleep hygiene. A 2018 study [mfn] Cooper, C. B., Neufeld, E. V., Dolezal, B. A., & Martin, J. L. (2018). Sleep deprivation and obesity in adults: a brief narrative review. BMJ open sport & exercise medicine, 4(1), e000392. https://doi.org/10.1136/bmjsem-2018-000392 [/mfn] has revealed that people who sleep less than 5 hours are more likely to suffer from weight issues.
- Being physically active [mfn] Kim, B. Y., Choi, D. H., Jung, C. H., Kang, S. K., Mok, J. O., & Kim, C. H. (2017). Obesity and Physical Activity. Journal of obesity & metabolic syndrome, 26(1), 15–22. https://doi.org/10.7570/jomes.2017.26.1.15 [/mfn] and exercising regularly are one of the most effective methods to lose excessive body fat. Lifting weights or doing cardio exercises can be highly effective for managing weight and mental health.
- Engage yourself in fun activities with your family and friends. Spend more time on pursuing your interests and hobbies.
- Practice stress relief techniques, such as mindfulness, breathing exercise, and meditation. Mindfulness [mfn] Katterman, S. N., Kleinman, B. M., Hood, M. M., Nackers, L. M., & Corsica, J. A. (2014). Mindfulness meditation as an intervention for binge eating, emotional eating, and weight loss: a systematic review. Eating behaviors, 15(2), 197–204. https://doi.org/10.1016/j.eatbeh.2014.01.005 [/mfn] practice can even prevent you from binge eating or emotional eating.
- Do not have food unless you feel hungry and try to chew more while eating as it helps in digesting the food properly.
- When experiencing discrimination or social stigma, keep calm and respond positively.
- Talk to your loved ones or consult with a mental health specialist if you find it extremely difficult to deal with such issues.
- Never hesitate to seek medical help, if needed.
Overcome Obesity
Obesity is a complex physical disease that involves abnormal weight gain. It not only causes several other physiological conditions but also affects a person’s mental health. People with mental health issues often use food as a coping technique which leads to weight gain.
Being overweight is often accompanied by various mental health problems, including depression, anxiety, and bipolar disorder. Obese people often experience discrimination, social stigma, bullying, and humiliation by their family, friends, peers, and society as a whole. One should consult with a health care specialist to deal with the physical and mental effects of this disease.
Obesity At A Glance
- Obesity is a complex disease related to excessive body fat build-up that negatively affects a person’s well-being.
- Obese people often experience social stigma, bullying, humiliation, and discrimination in different social situations.
- Being overweight is associated with different psychological disorders, such as depression, anxiety, and bipolar disorder.
- People with mental disorders often engage in emotional eating to deal with their stress-related problems, leading to abnormal weight gain.
- One can maintain a healthy body weight with a balanced diet, good sleep quality, regular physical exercise, and mindfulness practice.








Leave a Reply