Sleep arousal disorders, also known as non-rapid eye movement (NREM) sleep arousal disorders, are characterized by repeated episodes of partial awakening from sleep, which can include activities like sleepwalking and sleep terrors.
What Is Non-Rapid Eye Movement Sleep Arousal Disorders?
The Mind Help explains, ”non-rapid eye movement (NREM) sleep arousal disorders refer to a condition marked by recurrent episodes of incomplete awakening from sleep that include behaviors such as sleepwalking and sleep-terrors”.
The episodes usually occur during the first third of the night and the concerned person will be confused or disoriented if awoken during an episode. People with this ailment have no memory of their dreams or sleep behavior in the morning. NREM sleep arousal disorders are a group of conditions listed in the most recent edition of the DSM 5 mental health professionals guidebook.
The two disorders are called sleepwalking disorder and sleep terror disorder and they are clubbed under one major condition because they both highlight unusually aroused or agitated states of mind that takes place during a segment of the nightly sleep cycle called non-rapid eye movement sleep. American Psychiatric Association has described these conditions as mental health concerns as they potentially degrade the waking psychological function of affected individuals.
NREM sleep arousal disorders vary in terms of intensity, from mild to severe. In critical cases, NREM sleep arousal disorders can leave an unfavorable impact on relationships with important people and lead to medico legal consequences, especially if the individual engages in behaviors that may put others at risk.
In general, non-rapid eye movement sleep (NREM sleep) is the common name given to four individual, consecutive stages of sleep that all people go through during every extended sleeping session. These stages get their name because they lack the classic involuntary eye movement that occurs during the fifth stage of sleep, called rapid eye movement (REM) sleep.
A 2006 study [mfn]Markov, D., Jaffe, F., & Doghramji, K. (2006). Update on parasomnias: a review for psychiatric practice. Psychiatry Edgmont (Pa. : Township), 3(7), 69–76. [/mfn] states that non-rapid eye movement sleep arousal is a common condition during childhood and becomes less frequent after the age of five. A family history of arousal disorders, in general, predisposes the patient to these parasomnias. The factors that disrupt sleep and introduce arousals into normal sleep may include pain, stress, environmental noises, shift work, periodic limb movements, sleep apneas, and a full-bladder can also trigger disorders of arousal.
Read More About REM Sleep Here
Prevalence Of Non-Rapid Eye Movement Sleep Arousal Disorders
As per a study of 2007 [mfn]Mason TB 2nd, Pack AI. Pediatric parasomnias. Sleep. 2007 Feb;30(2):141-51. doi: 10.1093/sleep/30.2.141. PMID: 17326539.[/mfn] , disorders of arousal parasomnias or NREM sleep arousal disorders are more frequent during childhood than in adolescence or adulthood. Prevalence estimates for sleep terrors in childhood range from 1% to 6%, for sleepwalking up to 17% with a peak at 8-12 years, and for confusional arousals up to 17.3%.
Based on structured telephone interviews, it was reported that the percentage of adolescents and adults (aged 15-24 years) with sleep terrors was 2.2%, sleepwalking 2%, and confusional arousals were 4.2%. However, the prevalence was observed to have notably decreased after the age of 25, and no sex differences were observed.
Non-Rapid Eye Movement Sleep Arousal Disorders Are Classified Into The Following Categories.
As mentioned previously, non-rapid eye movement sleep arousal disorder is a cluster of sleep disorders namely sleepwalking and sleep terrors (or night terrors.) Additionally, confusional arousal has also been considered to be a category of this disorder about which we will discuss in this section.
1. Sleepwalking Disorder
Sleepwalking disorder [mfn] Guilleminault C, Kirisoglu C, da Rosa AC, Lopes C, Chan A. Sleepwalking, a disorder of NREM sleep instability. Sleep Med. 2006 Mar;7(2):163-70. doi: 10.1016/j.sleep.2005.12.006. Epub 2006 Feb 3. PMID: 16459139. [/mfn] is one of the conditions clubbed under the NREM sleep arousal disorder and people with this specific condition participate in a number of simple and complicated activities. Such activities are usually connected with a conscious state of mind like walking, talking, getting dressed, fixing food, using the bathroom, or driving, all being performed while still asleep.
Additionally, individuals also develop a subtype of this condition, namely the nocturnal eating disorder or a sleep-related eating disorder. It is defined by the consumption of high-calorie foods that do not normally play a prominent role in the patient’s daily, waking diets. Patients with sleepwalking disorder seldom remember limited phases of their sleeping behaviors the next day, but not the complete actions.
The National Sleep Foundation predicts that nearly 1 to 15% of Americans sleepwalk. While this behavior is common among younger children, it is also common to a certain extent among teens and adults. Things that tend to trigger the condition may include any infection or illness that results in high fever, use of sedative medicines, excessive alcohol use, use of specific non-sedative medications, a persistent lack of sufficient sleep, and the presence of a sleep-related condition called obstructive sleep apnea.
2. Sleep Terror Disorder
Sleep terror disorder [mfn] Leung AKC, Leung AAM, Wong AHC, Hon KL. Sleep Terrors: An Updated Review. Curr Pediatr Rev. 2020;16(3):176-182. doi: 10.2174/1573396315666191014152136. PMID: 31612833; PMCID: PMC8193803. [/mfn] or night terror disorder is a condition experienced by people when they are emotionally, extremely, and these distressing emotional states are more or less equal to those found in people who experience nightmares. However, unlike people with nightmares, people with this specific condition will tend to stay asleep throughout their experiences instead of waking up.
In addition, while individuals affected by nightmares usually recall their dreams precisely, individuals affected by sleep terrors either only hazily recall their experiences or do not recall them at all. Specific behaviours that can indicate a bout of sleep terror include unusually heavy breathing, abnormal thrashing or kicking movements, sitting upright while sleeping, shouting or making other loud noises vocalisations, leaping out of bed, assaulting a sleeping partner, and failing to wake up when prompted by others.
A number of factors, according to the Mayo Clinic, contribute to the development of sleep terror disorder. Chronic lack of sleep, sleeping in a new or odd place, sleeping in an abnormally loud or light setting, the after-effects of unusual daytime fatigue, and the after-effects of unusual nighttime exhaustion are just a few of them after-effects of daytime anxiety or stress.
Children who have fevers are at a higher risk of developing the disease. Additional potential causes or contributing factors include alcohol use, sedative use, antihistamine use, illicit drug use, obstructive sleep apnea, traumatic blows to the head, and migraine headaches. Roughly 3 percent of U.S. children suffer from sleep terrors; the condition also affects about 1 percent of U.S. adults.
3. Confusional Arousals
In this condition, the sleeper exhibits mental confusion or confusing behavior in bed. Most people who experience confusional arousals present very little autonomic arousal in the form of mydriasis (dilated pupils), tachycardia (accelerated heartbeat), tachypnea (accelerated breathing), or perspiration. Elpenor syndrome is another name for confusional arousals.
As per a 2001 study [mfn] Stores G. (2001). Dramatic parasomnias. Journal of the Royal Society of Medicine, 94(4), 173–176. https://doi.org/10.1177/014107680109400405 [/mfn], the prevalence rate of confusional arousal between the 15 to 24-year-old population is 6% and in those over the age of 65, it is 1% percent. Complex motor activity is absent in this sleep condition, although individuals may engage in instinctive activities such as picking at clothes and linens, kicking, thrashing in bed, and inappropriately handling things.
These episodes are not complemented by expressions of terror or sleepwalking. They precisely last from 1 to 10 minutes and are followed by retrograde amnesia for the event. These phenomena may occur in adults, as well, and result in cognitive abnormalities. Although different from sleep terrors and sleepwalking, confusional arousals may evolve into sleep terrors and sleepwalking.
Causes Of Non-Rapid Eye Movement Sleep Arousal Disorders
It is assumed that NREM sleep arousal disorder has a genetic component, whereby people with the sleepwalking disorder also have a family history of sleepwalking or sleep terrors. There are several other factors that play a significant role in the development of episodes, such as sedative use, sleep loss, sleep schedule disturbances, exhaustion, and physical or emotional stress.
As per a study [mfn] Mason TB 2nd, Pack AI. Pediatric parasomnias. Sleep. 2007 Feb;30(2):141-51. doi: 10.1093/sleep/30.2.141. PMID: 17326539. [/mfn], disorders of arousal are assumed to develop due to a faulty “switch” that blocks normal sleep cycle progression. The transition from sleep wave sleep (SWS) to lighter sleep, just before the onset of rapid-eye-movement (REM) sleep is abnormal. In this case, the patient is neither fully asleep nor fully awake. Additionally, there are other causes of NREM sleep arousal disorder as well. The study considers age as a significant issue as most of the parasomnias are likely to develop during childhood rather than later in life.
Another contributing factor involves the homeostatic drive to sleep, a specific situation where frequent or more critical parasomnia episodes are associated with prolonged sleep deprivation. Other factors that play a prominent role in triggering non-rapid eye movement sleep arousal disorder medications (e.g., neuroleptics, sedative-hypnotics, stimulants, and antihistamines), a loud or stimulating sleep environment, stress, fever, and inherent sleep disorders such as obstructive sleep apnea and periodic limb movements in sleep.
The study also mentions that genetic predisposition also results in arousal parasomnias. Some evidence drawn from the studies of sleep terrors states that the possible autosomal dominant disorder was observed in a 3-generation family. It was also reported that the prevalence of sleep terrors and sleepwalking in first-degree relatives of individuals with sleep terrors was 10 times greater than in the general population. It was estimated that a child has a 60% chance of being affected by this condition if both parents were affected.
Symptoms Of Non-Rapid Eye Movement Sleep Arousal Disorders
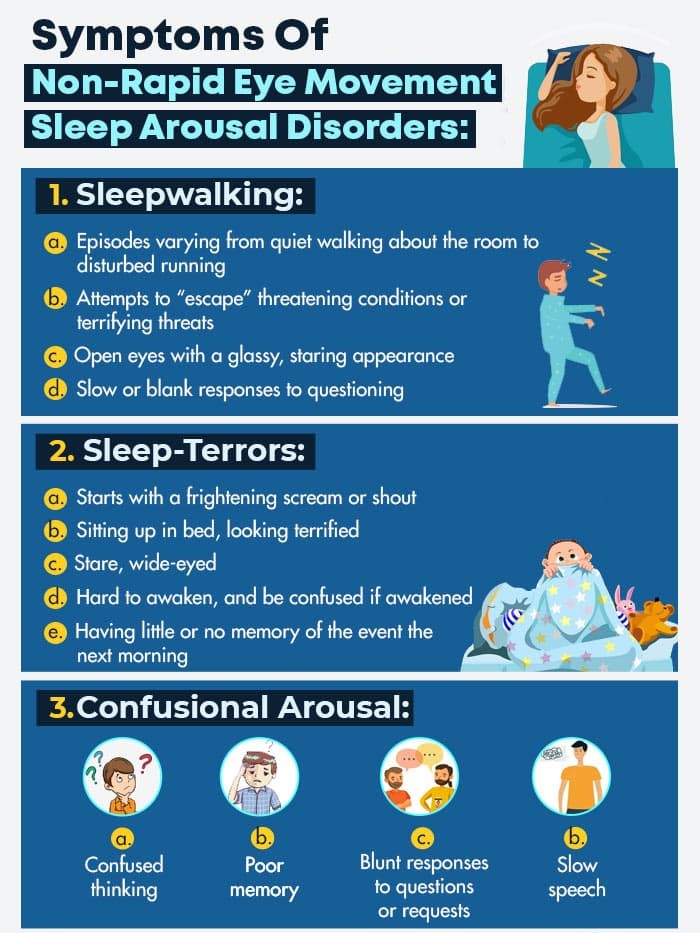
The symptoms of non-rapid eye movement sleep arousal disorders are divided into three categories, for three different conditions. These symptoms are as follows.
1. Sleepwalking
The symptoms for NREM sleep arousal disorder for the sleepwalking type are:
- Episodes varying from quiet walking about the room to disturbed running
- Attempts to “escape” threatening conditions or terrifying threats
- Open eyes with a glassy, staring appearance
- Slow or blank responses to questioning
- In the absence of awakening, failure to remember the event while with awakening comes possible embarrassment
2. Sleep-Terrors
The symptoms for NREM sleep arousal disorder for the sleep-terror type are:
- Starts with a frightening scream or shout
- Sitting up in bed, looking terrified
- Stare, wide-eyed
- Sweating, breathing heavily, and having a racing pulse, flushed face, and dilated pupils
- Kick and thrash
- Hard to awaken, and be confused if awakened
- Discouraged
- Having little or no memory of the event the next morning
- Possibly, getting out of bed and running around the house or showing aggressive behavior if restrained
3. Confusional Arousal
The symptoms for NREM sleep arousal disorder for the confusional arousal type are:
- Confused thinking
- Poor memory
- Slow speech
- Blunt responses to questions or requests
Diagnosis Of Non-Rapid Eye Movement Sleep Arousal Disorders
The diagnosis of NREM sleep arousal disorder is divided into three categories, each curated for the specific types. These are as follows,
1. Sleepwalking
To diagnose sleepwalking, the doctor will evaluate a patient’s medical history and symptoms. The evaluation may include:
- Physical Examination: The doctor will perform a physical examination to identify the presence of any condition that may be confused with sleepwalking, such as nighttime seizures, other sleep disorders, or panic attacks.
- Discussing the Symptoms: Unless a patient is staying alone, unaware of his/her condition, he/she will be informed by others about the sleepwalking behavior. The doctor may also question the patient’s sleep partner about this condition. Additionally, the doctor may also ask the patient and his/her partner to fill out a questionnaire about the patient’s sleep behaviors. Also, the person must inform the doctor about his/her family history of sleepwalking.
- Nocturnal sleep study (polysomnography): In some cases, the doctor may suggest an overnight study in a sleep lab. Sensors are placed on the patient’s body to record and monitor the brain waves, the oxygen level in the blood, heart rate, and breathing along with eye and leg movements while asleep. The patient may be videotaped to document his/her behavior during sleep cycles.
2. Sleep-Terror
To diagnose sleep terrors, the doctor may examine the patient’s medical history and symptoms. The evaluation may include:
- Physical Exam: The doctor may do a physical exam to identify any condition that may be contributing to the sleep terrors.
- Discussion of the Symptoms: Sleep terrors are usually diagnosed by the doctor based on the patient’s description of the events. The doctor may inquire about the family history of sleep problems. The doctor may also ask the patient or his/her partner to fill a questionnaire revolving around the person’s sleep behaviors.
- Nocturnal Sleep Study (polysomnography): Just like in sleepwalking, in some cases, the doctor may recommend an overnight study in the sleep lab. As mentioned previously, sensors are placed on the patient’s body to record and monitor the brain waves, the oxygen level in the blood, heart rate, and breathing along with eye and leg movements while the patient is asleep. The patient may also be videotaped to document his/her behavior during sleep cycles.
3. Confusional Arousal
To diagnose confusional arousal, the patient will have to see a sleep specialist as this sleep disorder may result in other severe problems. The doctor will tell you to complete a sleep diary for two weeks. This will give the doctor evidence as to what might be causing the problems. The patient can also rate his/her sleep with the Epworth Sleepiness Scale. This will display how the patient’s sleep is affecting his/her daily life.
Additionally, the doctor will ask questions to learn about the patient’s complete medical history. Thus, the patient must inform the doctor of his/her past or present drug and medication use. The doctor may also recommend an in-lab sleep study, where the patient’s brain waves, heartbeat, and breathing will be monitored while he/she is asleep.
It will record the movement of arms and legs move. An in-lab study will show whether there are other disorders, such as sleep apnea or a movement disorder that are causing sleep problems. A patient may also get videotaped to check for any unusual activities while the patient is asleep.
Treatment Of Non-Rapid Eye Movement Sleep Arousal Disorder
Treatment for NREM sleep arousal disorder depends on the severity of the condition. While most of the children will grow out of this condition with time, it may be frightening for the parents and the child will not be aware of their nighttime behavior. It is suggested to develop good habits around sleep as it may help reduce the frequency of episodes. For adults, it is recommended to reduce alcohol use to further reduce the symptoms.
It is also suggested to create a safe sleeping environment if the episodes are frequent or create a dangerous situation for the person and his/her bed partner. Such changes can include:
- Padding the floor around the bed with a mattress or pillows
- Window protection
- Padding corners of nearby furniture
- Removing dangerous objects from around the bedroom area
- Locking doors and windows
- Sleeping in a separate room from the bed partner until symptoms are under control
In severe cases, medication is also prescribed to reduce the frequency of episodes. Clinical research suggests that the following treatments for reducing the occurrence of episodes.
- Benzodiazepines, specifically diazepam and clonazepam, may reduce the symptoms of the condition.
- Triazolam and flurazepam have also been reported to be used with success.
- Antidepressant medications, specifically paroxetine and imipramine, have shown some benefit in case studies.
- Hypnosis has exhibited some positive effects in several case series
Read More About Antidepressants Here
As per a 2001 study [mfn] Stores G. (2001). Dramatic parasomnias. Journal of the Royal Society of Medicine, 94(4), 173–176. https://doi.org/10.1177/014107680109400405 [/mfn], the parents are first reassured that the episodes are often frightening events, however, the child is expected to grow out of them. Second, the patient must get regular and adequate sleep routines, to prevent sleep loss or disruption. Third, it is essential to make the sleep environment as safe as possible. Fourth, the parents should not try to wake or restrain a child during the episode.
It is suggested to wait until the episode subsides and calmly help him back to quiet sleep (the same applies to adults). Fifth, if the patient is unable to recall the episodes, there is no point in recounting them as it may lead to anxiety. Sixth, if sleepwalking or sleep terrors are persistent and constant in the time they occur, `scheduled waking’ can be helpful.
The treatment consists of gently and briefly waking the patient 15-30 minutes before the episode is due. The procedure is repeated for up to a month and initial reports suggest that improvement can be maintained for several months. Seventh, medication (e.g. low-dose clonazepam) is suggested for particularly worrying, embarrassing, or dangerous arousals where other measures have failed. Last, if there is evidence of an underlying psychological or physical disorder, special inquiries and help are needed.
An On-Time, Persistent Treatment Can Enhance the Symptoms
As noted previously, non-rapid eye movement sleep arousal disorder can be distressing, defined by episodes, for both the patient and bed partner. However (and fortunately), most disturbances resolve automatically by adolescence. For the residual and late-onset sleep arousal disorders, precise identification and management are vital.
Effective healthcare intervention includes appropriate referrals to specialists and clinics. Since NREM parasomnias can arise as secondary manifestations of underlying conditions, differentials must be eliminated. Again, this is best accomplished by pharmacy consultations, referrals to the appropriate specialists, and timely, persistent treatment with complete commitment.
Non-Rapid Eye Movement (NREM) Sleep Arousal Disorders At A Glance
- Non-rapid eye movement (NREM) sleep arousal disorders refer to a condition marked by recurrent episodes of incomplete awakening from sleep that include behaviors such as sleepwalking and sleep-terrors.
- NREM sleep arousal disorders vary in terms of intensity, from mild to severe.
- People with this ailment have no memory of their dreams or sleep behavior in the morning.
- Non-rapid eye movement sleep arousal disorder can be distressing, defined by episodes, for both the patient and bed partner.
- NREM sleep arousal disorder has a genetic component, whereby people with the sleepwalking disorder also have a family history of sleepwalking or sleep terrors.







Leave a Reply