Psychiatry is a medical specialty concerned with mental health conditions. It is the branch of medicine that deals with the diagnosis, treatment, and prevention of psychiatric disorders and illnesses and improves mental, emotional and behavioral health.
What Is Psychiatry?
It is a field of medicine that involves the study, causation, diagnosis, treatment and prevention of disorders related to cognition, emotions, mood, behaviors & perceptions. A person may ask for psychiatric support for several reasons, such as minor mental, emotional or behavioral issues or serious psychological disorders.
Our mental well-being can be affected by a wide range of internal and external factors, such as personality, self esteem, experiences and our interactions with our environment. This area of medicine helps us to deal with our mental health issues, enables us to function normally and live a healthy and satisfied life.
A doctor who practices psychiatry is known as a psychiatrist. Research [mfn] Dave K. P. (2016). Field of Psychiatry: Current Trends and Future Directions: An Indian Perspective. Mens sana monographs, 14(1), 108–117. https://doi.org/10.4103/0973-1229.193069 [/mfn] reveals that psychiatry is associated with genetics, neurology, research in general medicine, large-scale treatment trials and novel treatment approaches. Psychiatric assessment typically involves an analysis of the patient’s mental status, medical history, family history etc. The diagnosis process [mfn] Krystal, J. H., & State, M. W. (2014). Psychiatric disorders: diagnosis to therapy. Cell, 157(1), 201–214. https://doi.org/10.1016/j.cell.2014.02.042 [/mfn] may involve certain physical & psychological tests, such as lab tests, neuroimaging, interviews with patients and questionnaires.
Psychiatric research and analysis of different mental health conditions is primarily based on different leading diagnostic manuals, namely American Psychiatric Association’s (APA) the Diagnostic and Statistical Manual of Mental Disorders (DSM [mfn] Regier, D. A., Kuhl, E. A., & Kupfer, D. J. (2013). The DSM-5: Classification and criteria changes. World psychiatry : official journal of the World Psychiatric Association (WPA), 12(2), 92–98. https://doi.org/10.1002/wps.20050 [/mfn] ) and World Health Organization’s (WHO) the International Classification of Diseases (ICD [mfn] Fung, K. W., Xu, J., & Bodenreider, O. (2020). The new International Classification of Diseases 11th edition: a comparative analysis with ICD-10 and ICD-10-CM. Journal of the American Medical Informatics Association : JAMIA, 27(5), 738–746. https://doi.org/10.1093/jamia/ocaa030 [/mfn] ). Both manuals are revised and updated at intervals based on current research and findings to ensure clinicians are provided with the best guidance for diagnosis and treatment.
Psychiatric treatment typically involves a combination of psychotherapy and medications, however, it may also involve other treatment approaches such as community reinforcement. Based on the patient and the severity of the condition, treatment may be provided on an outpatient or inpatient basis.
Although it is among the oldest fields of medicine, psychiatry has significantly developed over the years due to the advancement of neuroscience. A 2015 study [mfn] Wu, Y., & Duan, Z. (2015). Analysis on evolution and research focus in psychiatry field. BMC psychiatry, 15, 105. https://doi.org/10.1186/s12888-015-0482-1 [/mfn] states “With the dramatic rise in mental disorders and mental illnesses, psychiatry has become one of the fastest growing clinical medical disciplines.”
Who Is A Psychiatrist?
A psychiatrist refers to a medical doctor who specializes in psychiatry and is concerned with the diagnosis, treatment and prevention of mental illnesses and substance use disorders. In order to become a psychiatrist, a medical practitioner or medico needs to finish an obligatory medical school training for 4 years and then specialize in psychiatry. These specialists are trained and licensed for the evaluation of both psychological and physical aspects of psychiatric disorders.
Studies [mfn] Harland, R., Antonova, E., Owen, G. S., Broome, M., Landau, S., Deeley, Q., & Murray, R. (2009). A study of psychiatrists’ concepts of mental illness. Psychological medicine, 39(6), 967–976. https://doi.org/10.1017/S0033291708004881 [/mfn] have found that these mental health professionals utilize different models to understand a wide range of clinical material and mental disorders. Psychiatrists generally deal with an array of mental conditions, such as depression, anxiety disorder, post traumatic stress disorder, bipolar disorder, schizophrenia, panic disorder, personality disorders, addiction etc.
A qualified medical doctor may choose to pursue different subspecialties of psychiatry, such as –
- General psychiatry
- Child and adolescent psychiatry
- Old age or geriatric psychiatry
- Forensic psychiatry
- Psychiatry of intellectual disability (PID)
- Medical psychotherapy
These physicians tend to recommend multiple treatment approaches, including medications like antidepressants, mood stabilizers & antipsychotics, and psychotherapies, such as counselling, cognitive behavioral therapy (CBT) and family or group therapy. They may also recommend hospitalization in extreme cases. However, research [mfn] Katschnig H. (2010). Are psychiatrists an endangered species? Observations on internal and external challenges to the profession. World psychiatry : official journal of the World Psychiatric Association (WPA), 9(1), 21–28. https://doi.org/10.1002/j.2051-5545.2010.tb00257.x [/mfn] reveals that currently psychiatrists are facing a crisis as there is a decline of recruitment into psychiatry observed in many countries.
Read More About Aging Here
History Of Psychiatry
According to research [mfn] Campbell’s Psychiatric Dictionary [/mfn] , the term psychiatry was originally used by German anatomist Johann Christian Reil during the 1800s in his paper. The word was derived from the Greek terms ‘psyche’, meaning the mind or soul, and ‘iatros’, meaning healer or physician.
It was initially described as a field of medicine that specializes in the prevention and treatment of different degrees and types of mental illness, regardless of how it is caused. However, this branch of medicine has advanced significantly over the past few decades to involve various other aspects of health and wellbeing beyond psychological phenomenon.
One 2008 study [mfn] Shorter E. (2008). History of psychiatry. Current opinion in psychiatry, 21(6), 593–597. https://doi.org/10.1097/YCO.0b013e32830aba12 [/mfn] explains that the history of psychiatry is a fundamental part of training for mental health professionals. The researchers of the study believe that understanding the history of this field can help trainees, specialists and senior practitioners gain psychiatric insights into treatments, alternative therapies and diagnoses that were once effective and flourished. “There is much benefit in psychiatry’s past – safe and effective therapeutic agents and diagnoses that cut nature at the joints, perhaps even better than the current crop,” adds the study.
Psychiatry Vs Psychology

Most people tend to be confused about the roles of a psychiatrist and a psychologist as both are healthcare professionals dealing with mental illnesses. Some people often use the terms psychiatrist and psychologist interchangeably, albeit mistakenly. Although both professions are associated with mental and emotional wellbeing, they are distinct and separate from each other in scope & content. Psychiatry and psychology mainly differ in terms of medical training and medical authority.
A psychiatrist is a medical doctor, while a psychologist studies our thoughts, emotions & behavior from a medical perspective and helps patients improve their behavior. Psychiatrists typically treat complex and serious mental disorders, while psychologists deal with developmental and behavioral problems. “Psychologists assess, diagnose, and treat the psychological problems and the behavioral dysfunctions resulting from, or related to physical and mental health,” explains a 2005 study [mfn] Wahass S. H. (2005). The role of psychologists in health care delivery. Journal of family & community medicine, 12(2), 63–70. [/mfn] .
Psychiatrists act as medical doctors and recommend psychotherapies & medications or pharmacological interventions for treating mental, emotional & behavioral disorders. Psychologists, however, are not qualified to prescribe medications for mental and emotional abnormalities. Even though a psychologist may have doctorate degrees, they are not considered medical doctors.
They primarily recommend psychotherapy, like cognitive & behavioral interventions for the treatment of mental health issues. Both professionals tend to perform similar roles and responsibilities at times but the context is typically different. Psychiatrists receive mandatory training to practice as physicians and hold a Doctor of Medicine (MD) or a Doctor of Osteopathic Medicine (DO).
Psychologists are graduates in psychology and receive a Doctor of Psychology (PsyD) or Doctor of Philosophy (PhD) in counseling or clinical psychology. However, a psychologist can choose to pursue psychiatry and become a psychiatrist by attending medical school, receiving the required medical training and meeting the requirements.
Regardless, psychiatrists and psychologists often work with each other in treating patients. While a psychologist may refer a patient to a psychiatrist for prescribing medications, a psychiatrist may refer a patient to a psychologist for specific therapy after an initial diagnosis. “Psychiatrists and clinical psychologists share an inevitable, if rather uneasy, relationship. So very much like a modern marriage. Can’t do without it, can’t get out of it,” states a 2006 study [mfn] Singh, A., & Singh, S. (2006). Psychiatrists and clinical psychologists. Mens sana monographs, 4(1), 10–13. https://doi.org/10.4103/0973-1229.27599 [/mfn] .
What Psychiatrists Do
The branch of psychiatry is concerned with the treatment of psychological conditions. Psychiatrists not only have an excellent understanding of psychiatric concepts, they are also knowledgeable about basic psychology and are trained in psychotherapy skills as well.
These specialists are required to possess high levels of empathy, compassion, patience, emotional intelligence and communication skills so that they can clearly understand what the patient is experiencing and offer effective and satisfactory treatment. After analyzing the mental, emotional, behavioral and physical symptoms, they make an accurate diagnosis and create a treatment and management plan for successful recovery of the patient.
A 2016 study [mfn] Maung H. H. (2016). Diagnosis and causal explanation in psychiatry. Studies in history and philosophy of biological and biomedical sciences, 60, 15–24. https://doi.org/10.1016/j.shpsc.2016.09.003 [/mfn] has found that a proper diagnosis by a medical doctor trained in psychiatry can explain the patient’s symptoms by specifying the causes of onset of the disorder(s). “Diagnoses in psychiatry are also sometimes presented in clinical texts as if they pick out pathological processes that cause sets of symptoms,” adds the study. Usually, when dealing with patients, a psychiatrist can –
- Reduce critical symptoms and improve patient’s quality of life
- Help to overcome impairments in daily functioning due to mental problems
- Deliver urgent care in cases of emergency or sudden mental disorders
- Help patients to cope with any personal challenges or life struggles, like abuse or trauma
- Help to regulate and relieve long-term mental illnesses
- Recommend essential lifestyle changes for better & faster recovery
- Empower caregivers, family members or partner to provide better care to the patient
- Offer advice & second opinions to patients and health professionals
- Refer patient to other more appropriate doctors
- Recommend hospitalization, if needed
They can also help a patient struggling with trauma, abuse, neglect or violence, having relationship or career problems, experiencing family issues, financial stress, emotional dysregulation, mood swings, personality issues or abnormal behavior. Psychiatry enables the practitioners to diagnose an individual considering their mental, physical and social wellbeing. Psychiatrists are qualified to offer best treatment & care for a wide range of mental disorders such as –
- Anxiety
- Depression [mfn] Davidsen, A. S., & Fosgerau, C. F. (2014). What is depression? Psychiatrists’ and GPs’ experiences of diagnosis and the diagnostic process. International journal of qualitative studies on health and well-being, 9, 24866. https://doi.org/10.3402/qhw.v9.24866 [/mfn]
- Hallucinations
- Panic attacks
- Phobias
- Post-traumatic stress disorder (PTSD [mfn] Smith, P., Dalgleish, T., & Meiser‐Stedman, R. (2018). Practitioner review: Posttraumatic stress disorder and its treatment in children and adolescents. Journal of Child Psychology and Psychiatry, 60(5), 500-515. https://doi.org/10.1111/jcpp.12983 [/mfn] )
- Alzheimer’s disease & dementia
- Obsessive compulsive disorder (OCD [mfn] Janardhan Reddy, Y. C., Sundar, A. S., Narayanaswamy, J. C., & Math, S. B. (2017). Clinical practice guidelines for Obsessive-Compulsive Disorder. Indian journal of psychiatry, 59(Suppl 1), S74–S90. https://doi.org/10.4103/0019-5545.196976 [/mfn] )
- Schizophrenia [mfn] Frese, F. J., 3rd, Knight, E. L., & Saks, E. (2009). Recovery from schizophrenia: with views of psychiatrists, psychologists, and others diagnosed with this disorder. Schizophrenia bulletin, 35(2), 370–380. https://doi.org/10.1093/schbul/sbn175 [/mfn]
- Bipolar disorder [mfn] Cerimele, J. M., Halperin, A. C., Spigner, C., Ratzliff, A., & Katon, W. J. (2014). Collaborative care psychiatrists’ views on treating bipolar disorder in primary care: a qualitative study. General hospital psychiatry, 36(6), 575–580. https://doi.org/10.1016/j.genhosppsych.2014.07.013 [/mfn]
- Paranoia
- Personality disorders [mfn] Tyrer, P., & Simonsen, E. (2003). Personality disorder in psychiatric practice. World psychiatry : official journal of the World Psychiatric Association (WPA), 2(1), 41–44. [/mfn]
- Sleep disorders
- Eating disorders
- Substance use disorders & addictions
- Suicidal thoughts
Read More About Phobia Here
These medical doctors also deliver psychological support to patients suffering from debilitating or terminal long-term physical health conditions. Although psychiatrists deal with conditions associated with the brain, they do not treat structural and organic conditions like brain cancers, epilepsy etc. However, they may help to reduce the psychiatric symptoms of different physical health conditions.
Subspecialties In Psychiatry
According to a 2006 report [mfn] Trivedi, J. K., & Goel, D. (2006). What psychiatry means to us. Mens sana monographs, 4(1), 166–183. https://doi.org/10.4103/0973-1229.27613 [/mfn] , this field of medicine involves a number of subspecialties, such as –
1. General adult psychiatry
This subspeciality refers to general psychiatry where a physician has received general psychiatric training in this branch of medicine for treating adult patients. When a specialist talks about practicing psychiatry, this is what they typically mean.
2. Child and adolescent psychiatry
The subspeciality is focused on the mental wellbeing of children, adolescents and teens. As the mindset of children is very different from adults, special psychiatric training is required for specialists to understand their thought and behavior patterns, identify the triggers and the symptoms of the mental conditions. Moreover, the treatment for children & adolescents also tends to vary.
3. Geriatric psychiatry
Although a recent discipline, this form of psychiatric diagnosis and treatment focuses on the mental illnesses of the elderly. “Like children, the elderly also have different pharmacokinetics of drugs, different presentations of disorders, and also disorders exclusively seen in this age group,” explains the 2006 report. As the mental health requirements of the elderly are different from other age groups, special attention is needed.
4. Emergency psychiatry
This subspeciality is important as it can often be difficult for improperly and hastily trained psychiatrists to cope with or diagnose emergency cases. “Psychiatric emergencies can be disruptive not only for the patient but also for society, family or for national property,” adds the report.
5. Forensic psychiatry
This speciality is needed as psychiatric patients often experience abuse and maltreatment. Hence, specialists need to be aware of specific rules and laws associated with the treatment of mentally challenged individuals and the legal implications of psychiatry for both the caregivers and the doctors.
6. Addiction and substance abuse psychiatry
The report states “it is always challenging to deal with substance abuse related problems and emphasis on rigorous training in this subspeciality is being given.”
7. Consultation-liaison psychiatry
Surgeons, general physicians and other healthcare professionals often find it challenging to recognize the psychological signs and symptoms of physical disorders and other comorbid psychiatric disorders. This subspeciality focuses on training specialists to work with other doctors and be a part of their expert team.
Apart from these, there can be many other subspecialties in this branch of medicines, some of which are mentioned below:
- Military psychiatry
- Neuropsychiatry
- Perinatal psychiatry
- Occupational psychiatry
- Psychotherapy
- Sleep specialists
- Learning disabilities
- Psychosomatic medicine
- Brain Injury Medicine
- Clinical neurophysiology
- Evolutionary Psychiatry
- Biological psychiatry
- Community and social psychiatry
- Sexology
- Hospice and palliative medicine
However, it should be noted that for some of these subspecialities, no formal certification may be provided. “It is desirable that psychiatrists attempt to define the social and environmental conditions under which the individual thrives or breaks down,” adds the 2006 report. Further research [mfn] Firth, J., Solmi, M., Wootton, R. E., Vancampfort, D., Schuch, F. B., Hoare, E., Gilbody, S., Torous, J., Teasdale, S. B., Jackson, S. E., Smith, L., Eaton, M., Jacka, F. N., Veronese, N., Marx, W., Ashdown-Franks, G., Siskind, D., Sarris, J., Rosenbaum, S., Carvalho, A. F., … Stubbs, B. (2020). A meta-review of “lifestyle psychiatry”: the role of exercise, smoking, diet and sleep in the prevention and treatment of mental disorders. World psychiatry : official journal of the World Psychiatric Association (WPA), 19(3), 360–380. https://doi.org/10.1002/wps.20773 [/mfn] indicates that multiple lifestyle factors should also be considered by psychiatrists when diagnosing and treating patients with mental health issues and psychological disorders.
When To Seek Psychiatric Help
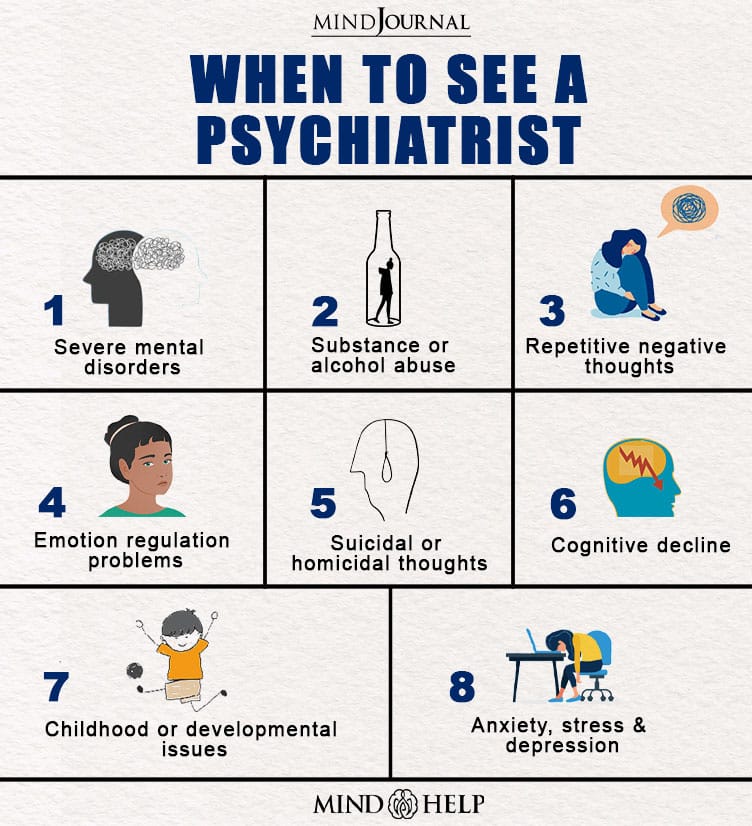
As psychiatry is a vast field, a person may consult a psychiatrist for a number of different reasons. Some of the most common reasons to see a specialist in this field may include –
- Complex mental disorders
- Childhood or developmental issues, like autism
- Excessive worry, constant fear or anxiety
- Extreme stress or trauma after major life events
- Cognitive decline or intellectual disability
- Inability to relax
- Repetitive obsessive, intrusive or negative thoughts
- Emotion regulation problems
- Chronic low mood or depression
- Problems with memory, attention, concentration or hyperactivity
- Sleep disorders or difficulties
- Experiencing paranoia, hallucinations or delusions
- Substance or alcohol abuse
- Behavioral addictions such as gambling
- Issues with self-esteem or body image
- Anger management issues or violent outbursts
- Suicidal thoughts or self-injurious behavior
- Homicidal tendencies or thoughts about hurting others
It can also be important to see a psychiatrist when a patient doesn’t successfully respond to the standard treatment under the guidance of a general physician. Another major reason is when a patient requires certain medicines that only a qualified specialist in psychiatry can prescribe.
How Psychiatrists Treat Patients
Physicians trained and qualified in psychiatry can perform a complete diagnosis of the patient. Apart from conducting interviews with patients and caregivers, they can also perform psychological examinations and lab tests to gain better understanding of the patient’s condition. However, diagnosis typically relies on the criteria established in APA’s Diagnostic and Statistical Manual of Mental Disorders (DSM-5 [mfn] Substance Abuse and Mental Health Services Administration. DSM-5 Changes: Implications for Child Serious Emotional Disturbance [Internet]. Rockville (MD): Substance Abuse and Mental Health Services Administration (US); 2016 Jun. Available from: https://www.ncbi.nlm.nih.gov/books/NBK519708/ [/mfn] ).
Once a patient has been accurately diagnosed, a psychiatrist will devise a customized treatment plan based on the severity of the disorder and the patient’s recovery needs. Depending on the condition and symptoms, the doctor may recommend an array of treatment approaches involving medications, psychotherapy, psychosocial interventions and other approaches like brain stimulation therapies, such as electroconvulsive therapy (ECT [mfn] Singh, A., & Kar, S. K. (2017). How Electroconvulsive Therapy Works?: Understanding the Neurobiological Mechanisms. Clinical psychopharmacology and neuroscience : the official scientific journal of the Korean College of Neuropsychopharmacology, 15(3), 210–221. https://doi.org/10.9758/cpn.2017.15.3.210 [/mfn] ).
The doctor may prescribe certain medications, such as antidepressants, mood stabilizers, antipsychotic drugs, anti-anxiety medications, hypnotics, stimulants, anxiolytics and sedatives for threatening different mental disorders. However, as certain medications can have adverse side-effects [mfn] Ramic, E., Prasko, S., Gavran, L., & Spahic, E. (2020). Assessment of the Antidepressant Side Effects Occurrence in Patients Treated in Primary Care. Materia socio-medica, 32(2), 131–134. https://doi.org/10.5455/msm.2020.32.131-134 [/mfn] , patients need to consult the psychiatrist at regular intervals so that the effectiveness of the drugs and any probable side effects can be monitored.
The specialist can also recommend psychotherapy approaches, such as cognitive behavioral therapy (CBT [mfn] Hofmann, S. G., Asnaani, A., Vonk, I. J., Sawyer, A. T., & Fang, A. (2012). The Efficacy of Cognitive Behavioral Therapy: A Review of Meta-analyses. Cognitive therapy and research, 36(5), 427–440. https://doi.org/10.1007/s10608-012-9476-1 [/mfn] ), as it is considered as the first-line treatment [mfn] Persons, J. B., Thase, M. E., & Crits-Christoph, P. (1996). The role of psychotherapy in the treatment of depression: review of two practice guidelines. Archives of general psychiatry, 53(4), 283–290. https://doi.org/10.1001/archpsyc.1996.01830040013003 [/mfn] for a number of mental health conditions, like depression and anxiety. Psychotherapy can help to relieve symptoms for a wide range of mental, emotional and behavioral conditions, improve the patient’s ability for daily functioning and enhance their quality of life. Depending on the disorder and the severity of the symptoms, the number of sessions may vary from a few weeks to a few years.
A person can consult a psychiatrist in a number of settings, such as public and private hospitals, psychiatric institutes, clinics, private consulting rooms, emergency rooms, community mental health services, nursing homes, rehabilitation programs etc.
Takeaway
Psychiatry is regarded as a diverse medical discipline as mental health tends to exist on a spectrum. Although not all mental health issues may require a psychiatric consultation, most complex and severe mental illnesses necessitate treatment under the supervision of a psychiatrist.
A patient can either directly consult a psychiatrist or they may be referred to one by a general physician or a family doctor. The psychiatrists may recommend a variety of treatment options and the type of treatment depends on the illness and the individual. Regardless of the treatment approach, these specialists can help patients effectively manage the condition, recover successfully and live a healthier life.
Psychiatry At A Glance
- Psychiatry is a branch of medicine that deals with the diagnosis, treatment and prevention of mental health conditions.
- A psychiatrist is a practitioner of psychiatry and a medical doctor who diagnoses and treats an array of mental illnesses and substance use disorders.
- Psychiatry is different from psychology in terms of medical training and medical authority. Psychiatrists can prescribe medications for treatment but psychologists are not qualified to do so.
- Psychiatry includes a number of subspecialties, such as general psychiatry, child and adolescent psychiatry, geriatric psychiatry, forensic psychiatry, psychiatry of intellectual disability (PID) and medical psychotherapy.
- Psychiatrists are qualified to deal with an array of mental disorders, like anxiety, depression, hallucinations, phobias, PTSD, OCD, schizophrenia, bipolar disorder, personality disorders, addictions, suicidality etc.
- After diagnosis, the psychiatrist devises a treatment plan based on the disorder and the patient’s needs.






Leave a Reply