Sleep paralysis is a sensation of being unable to move, which can occur at the start of sleep or when you wake up. Although it is a temporary experience, it may lead to several severe symptoms.
What Is Sleep Paralysis?
Sleep paralysis is a common sleep problem and is a form of parasomnia. It is a temporary mental state characterized by an inability to move during either falling asleep or waking up. During this experience, the person remains aware and may often hallucinate. They can see, hear or feel things which are not real leading to intense fear and anxiety. The American Psychological Association (APA) describes the condition as a “brief inability to move or speak just before falling asleep or upon awakening, often accompanied by terrifying hallucinations.”
Usually, an episode may last for a few seconds or even minutes. An individual may experience a single or multiple episodes during their lifetime. According to Harvard Medical School, the episodes may last “no more than several minutes. Like cataplexy, sleep paralysis probably is related to insufficient separation between REM sleep and the awake state.” Research indicates that around 4% to 40% of people may suffer from this condition.
However, according to The American Journal of Psychiatry[mfn] Sleep paralysis. 2006. American Journal of Psychiatry. https://ajp.psychiatryonline.org/doi/abs/10.1176/ajp.108.12.921 [/mfn], “Sleep paralysis apparently occurs more frequently than reported cases would indicate.” It has also been observed that around 7.6% of the global population experiences at least one episode in their lifetime. The condition is also found to be occurring frequently in psychiatric patients and students almost equally, reveals a 2011 study [mfn] Sharpless, B. A., & Barber, J. P. (2011). Lifetime prevalence rates of sleep paralysis: a systematic review. Sleep medicine reviews, 15(5), 311–315. https://doi.org/10.1016/j.smrv.2011.01.007 [/mfn]. Lifetime episodes of this sleep disorder are fairly common and equally affect men and women. On average, onset is usually experienced between 14 and 17 years.
Most sufferers are often reluctant to discuss the symptoms with their family and friends due to shame and fear of embarrassment. Hence, they rarely seek treatment. Sleep paralysis is usually not threatening even if the sufferer may feel otherwise. Medical intervention is usually not needed unless the patient feels extreme anxiety and fear.
Understanding Sleep Paralysis
Sleep paralysis can be observed in seemingly healthy individuals or in people with narcolepsy. According to the APA, it can also be caused by “temporary malfunction of the reticular activating system.” However, the condition may also be genetic as it may run in families. It is often caused by a variety of factors, like abnormal sleep cycles, psychological stress, panic disorder, jet lag and sleep deprivation. The condition is believed to be associated with narcolepsy, hypokalemic periodic paralysis and atonic seizure.
When the episodes take place without the presence of narcolepsy or any other condition, it is known as isolated sleep paralysis (ISP); however, recurrent isolated sleep paralysis (RISP) includes multiple episodes over time and is a more well known sleep-wake disorder. According to a 2015 scientific analysis [mfn] Gangdev, P., Dua, V., & Desjardins, N. (2015). Isolated sleep paralysis and hypnic hallucinations in schizophrenia. Indian journal of psychiatry, 57(4), 383–385. https://doi.org/10.4103/0019-5545.171834 [/mfn], isolated sleep paralysis, accompanied by hypnic hallucinations, is widespread and “because of the overlap of symptoms with schizophrenia, their identification is important but unrecognized.”
Sleep paralysis is usually not associated with any underlying mental health issues of psychiatric problems. It is simply a loss of muscle function through the daily rhythms of the sleep-wake cycle [mfn] Waterhouse, J., Fukuda, Y., & Morita, T. (2012). Daily rhythms of the sleep-wake cycle. Journal of physiological anthropology, 31(1), 5. https://doi.org/10.1186/1880-6805-31-5 [/mfn]. However, the combination of conscious awareness and inability to move smoothly during the stages of sleep can be a terrifying experience. The person may feel that they are awake yet are unable to speak or move for a few minutes or seconds.
How Sleep Paralysis Affects Us
In a study [mfn] Jalal B. (2018). The neuropharmacology of sleep paralysis hallucinations: serotonin 2A activation and a novel therapeutic drug. Psychopharmacology, 235(11), 3083–3091. https://doi.org/10.1007/s00213-018-5042-1 [/mfn], Dr. Baland Jalal, Department of Psychiatry and Behavioural and Clinical Neuroscience Institute, University of Cambridge, explains “Sleep paralysis is a state of involuntary immobility occurring at sleep onset or offsets, This is frequently accompanied by strange “ghost-like” hallucinations and extreme fear reactions.” During paralysis episodes, most sufferers are known to have multisensorial and vivid dream activity, as well as nightmares.
According to a 2016 study [mfn] Sharpless B. A. (2016). A clinician’s guide to recurrent isolated sleep paralysis. Neuropsychiatric disease and treatment, 12, 1761–1767. https://doi.org/10.2147/NDT.S100307 [/mfn], a person affected by sleep paralysis may awaken with rapid eye movement sleep-based atonia and have conscious awareness. It states “This is usually a frightening event often accompanied by vivid, waking dreams (ie, hallucinations).” Conscious nightmares and atonia can make the episodes extremely unpleasant for the patients. Some sufferers may also experience choking and a weight or pressure on top of them.
Moreover, due to vivid nightmares, sufferers may also sense an evil presence near them. As the condition is not easily explainable or understood, most people seek non-scientific explanations to understand their condition which may lead to strong supernatural or superstitious beliefs. It is not uncommon for sufferers to believe that they have experienced demonic attacks, possessions or alien abductions.
Sleep paralysis is often attributed to the development of certain paranormal and alien abduction theories due to its significant mention in history. Symptoms of the condition have been observed in different cultures over the centuries and has led to the creation of various supernatural beliefs, like aliens, shadow people [mfn] Arzy, S., Seeck, M., Ortigue, S., Spinelli, L., & Blanke, O. (2006). Induction of an illusory shadow person. Nature, 443(7109), 287. https://doi.org/10.1038/443287a [/mfn], night demons, hat man and even Shakespeare’s the old hag.
Due to these hallucinations of shadowy evil beings, the experience can lead to severe anxiety and intense feelings of fear and terror. According to a 2018 study [mfn] Jalal B. (2018). The neuropharmacology of sleep paralysis hallucinations: serotonin 2A activation and a novel therapeutic drug. Psychopharmacology, 235(11), 3083–3091. https://doi.org/10.1007/s00213-018-5042-1 [/mfn], hallucinatory experiences associated with sleep paralysis possess similar characteristics as serotonergic hallucinations. The study adds that these “are strikingly similar to perceptual and subjective states induced by hallucinogenic drugs,” and include extreme fear reactions, OBEs, mystical experiences and visual hallucinations.
Types Of Sleep Paralysis
Sleep paralysis often occurs when a person is:
- Falling asleep
- Immediately after falling asleep
- Waking up
If the episodes occur while the person is falling asleep, it is known as predormital or hypnagogic sleep paralysis. If the episode is experienced when they are waking up, then it is identified as postdormital or hypnopompic sleep paralysis.
1. Hypnagogic Sleep Paralysis
When we start falling asleep, our body and mind begins to relax. Generally, we tend to be less aware and fail to notice any change in our ability to function as it helps us to fall asleep. However, if we become or remain conscious during this process, we become aware that we are unable to move our body or speak. This may also lead to mystical visual hallucinations as well. The Harvard Medical School explains that Hypnagogic hallucinations “are dreamlike images that are seen during the awake state instead of during sleep. These terrible visions occur just as the person is about to fall asleep or wake up.
2. Hypnopompic Sleep Paralysis
Our body and mind shifts between two types of sleep:
- REM (rapid eye movement)
- NREM (non-rapid eye movement)
NREM sleep usually occurs first and comprises 75-80% of the total time we spend sleeping. However, REM sleep constitutes only 20-25% of overall sleep time. It is believed that one cycle of NREM and REM can last up to 90 minutes. Our body relaxes and rejuvenates itself during NREM sleep and when it ends, the sleep cycle transforms to REM sleep.
During this stage, our body remains calm and relaxed but we tend to see vivid dreams and our eyes move rapidly. Moreover, our muscles tend to become “inactive” during the REM stage. If a person becomes consciously aware before the REM cycle is complete, they may experience a loss of muscle function or may be unable to speak.
Read More About REM Sleep Here
Sleep Paralysis, Nightmares And Hallucinations
Sleep paralysis can result in vivid, multisensorial waking nightmares and hallucinations while transitioning from sleeping to waking and vice versa. One study [mfn] Cheyne, J. A., Rueffer, S. D., & Newby-Clark, I. R. (1999). Hypnagogic and hypnopompic hallucinations during sleep paralysis: neurological and cultural construction of the night-mare. Consciousness and cognition, 8(3), 319–337. https://doi.org/10.1006/ccog.1999.0404 [/mfn] states that “Hypnagogic and hypnopompic experiences (HHEs) accompanying sleep paralysis (SP) are often cited as sources of accounts of supernatural nocturnal assaults and paranormal experiences.” Most descriptions of such hallucinatory experiences from sufferers tend to be similar and consistent across cultures and time.
Research [mfn] McCarty, D. E., & Chesson, A. L., Jr (2009). A case of sleep paralysis with hypnopompic hallucinations. Recurrent isolated sleep paralysis associated with hypnopompic hallucinations, precipitated by behaviorally induced insufficient sleep syndrome. Journal of clinical sleep medicine : JCSM : official publication of the American Academy of Sleep Medicine, 5(1), 83–84. [/mfn] indicates that sufferers affected by sleep paralysis can experience intense fear, breathlessness, strange sensations and visual imagery of a “foreign presence in the room.” Most episodes happen due to nocturnal awakening and can be experienced at any moment during the night. Based on research and evidence, the episodes of sleep paralysis can be experienced in 3 major categories:
1. Intruders
This type of episode involves fear, sensed presence and visual & auditory hallucinations related to an intruder [mfn] Jalal, B., & Ramachandran, V. S. (2017). Sleep Paralysis, “The Ghostly Bedroom Intruder” and Out-of-Body Experiences: The Role of Mirror Neurons. Frontiers in human neuroscience, 11, 92. https://doi.org/10.3389/fnhum.2017.00092 [/mfn]. It is estimated that this is a result of a “hypervigilant state initiated in the midbrain.” The sufferer may see or hear sounds of coming from an intruder or an evil presence in the room or house. Common hallucinatory sounds heard by patients may include whispers, door-knobs turning, doors creaking, footsteps. They may even see a “shadow person” or a demonic entity watching them.
A study [mfn] Brian A. Sharpless, Monika Kliková, Clinical features of isolated sleep paralysis, Sleep Medicine, Volume 58, 2019, Pages 102-106, ISSN 1389-9457, https://doi.org/10.1016/j.sleep.2019.03.007. [/mfn] published in Sleep Medicine discovered that around 58% of sufferers tend to “sensed a presence in the room with them,” and most believe that it is a “non-human” entity. Moreover, about 22% of participants in the study claimed that they actually saw an intruder in their room, who is typically a stranger.
2. Demonic presence
The sufferer may feel a heavy pressure on their chest or abdomen leading to difficulty in breathing. It may make the patient feel like a malevolent invisible entity is sitting on top of them, leading to a feeling of being strangled, smothered or sexually assaulted. The sufferer may seriously believe that they may die. It is believed to be caused by “hyperpolarization of motoneurons on perceptions of respiration.”
These two categories largely include a supernatural or alien element that have been described in various historical and contemporary documented cases across various cultures.
3. Unusual Bodily Experiences
The sufferer may also experience certain forms of vestibular-motor hallucinations or out-of-body experiences (OBEs) [mfn] Blanke O. (2004). Out of body experiences and their neural basis. BMJ (Clinical research ed.), 329(7480), 1414–1415. https://doi.org/10.1136/bmj.329.7480.1414 [/mfn], like hovering over their own body, flying or floating away, visiting a different realm, a sense of falling or spinning etc. This category involves experiences that are physically impossible and are caused by “conflicts of endogenous and exogenous activation” associated with body movement, orientation and position.
In extreme cases, sufferers can become afraid of sleeping and may experience fatigue, memory difficulty, excessive anxiety and worry. They may be afraid of discussing their problems with others due to fear of embarrassment.
Read More About Nightmares And Nightmare Disorder Here
Cultural Significance Of Sleep Paralysis
Although there is some debate among psychologists, anthropologists and other researchers, sleep paralysis is strongly associated with the culture of the sufferer. According to researchers, social and cultural background can have a strong impact on a person suffering from this condition. Long-held cultural beliefs are often used to explain the hallucinations, visions, sensations and emotions experienced during an episode.
A 2019 scientific analysis states [mfn] McCleese, Kaitlyn (2019) “The Effects of Culture on Sleep Paralysis Experiences,” The Omnipedia Review: Vol. 1 : Iss. 1 , Article 5. Available at: https://digitalcommons.longwood.edu/omni/vol1/iss1/5 [/mfn] “In many cases, these episodes are explained as supernatural intervention in the lives of humans. Demons, spirits, and night hags are the most common culprits, and these are reinforced by deeply held beliefs that the supernatural exists in our own reality.”
According to a 2005 research paper [mfn] Hinton, D. E., Hufford, D. J., & Kirmayer, L. J. (2005). Culture and Sleep Paralysis [Editorial]. Transcultural Psychiatry, 42(1), 5–10. https://doi.org/10.1177/1363461505050708 [/mfn], the condition generally includes interesting similarities across cultures but also involves radical differences. As culture influences language, the description of the episodes may involve cultural differences. According to the researchers, “culturally shaped cognition during the seconds or minutes of the sleep paralysis event itself may lead to the person experiencing intense fear or specific hallucinatory experiences, including out-of-body experiences.”
Perhaps due to such cultural differences, sufferers tend to experience a variety of supernaturally-inclined hallucinations, such as spirits, ghosts, visits from aliens etc. The strange nature of this condition, along with respective cultural backgrounds, lends conviction to these far-fetched, supernatural explanations.
Here are some of the common supernatural beliefs used to explain the condition based on different cultures:
1. Incubus/Succubus
Sleep paralysis has long been associated with the phenomenon of incubus and succubus. Both incubi and succubi are demonic entities that sexually torment the sufferers, based on their genders. According to mythology and folklore, the incubus or succubus attacks innocent people while they are asleep and lies upon them to conduct sexual assault. According to traditional societies, repeated encounters with these demons can adversely affect the physical and mental health of an individual and eventually lead to death.
2. The Night Hag
The night hag is also used as a common supernatural explanation across various cultures. It is a supernatural ‘witch-like’ creature that sits at the foot of the bed or atop the person’s chest. It is also referred to as the Old Hag in Newfoundland. It is also known as the Mare, a malicious entity according to Germanic and Slavic folklore.
3. Other Supernatural Beliefs
Here are some of the common supernatural explanations used across different cultures:
- Studies [mfn] Jalal, B., Hinton, D.E. Rates and Characteristics of Sleep Paralysis in the General Population of Denmark and Egypt. Cult Med Psychiatry 37, 534–548 (2013). https://doi.org/10.1007/s11013-013-9327-x [/mfn] reveal that in Egypt, sleep paralysis is strongly associated with malevolent spirits, like the Jinn
- Canadian Eskimos believe that such episodes are caused by spells of shamans
- According to a 2005 study [mfn] Hinton, D. E., Pich, V., Chhean, D., & Pollack, M. H. (2005). ‘The ghost pushes you down’: sleep paralysis-type panic attacks in a Khmer refugee population. Transcultural psychiatry, 42(1), 46–77. https://doi.org/10.1177/1363461505050710 [/mfn], the phenomenon is identified as “the ghost pushes you down,” by Cambodians
- Sleep paralysis is referred to as a pandafeche attack [mfn] Jalal, B., Romanelli, A., & Hinton, D. E. (2015). Cultural Explanations of Sleep Paralysis in Italy: The Pandafeche Attack and Associated Supernatural Beliefs. Culture, medicine and psychiatry, 39(4), 651–664. https://doi.org/10.1007/s11013-015-9442-y [/mfn] in Italy
- Japanese traditions explain that the episodes occur due to suffocation while sleeping
- from vengeful spirits and is known as Kanashibari
- According to Nigerian culture, a female demon is believed to attack sufferers during nightmares leading to paralysis
- Brazilian folklore identifies the condition as Pisadeira [mfn] de Sá, J. F., & Mota-Rolim, S. A. (2016). Sleep Paralysis in Brazilian Folklore and Other Cultures: A Brief Review. Frontiers in psychology, 7, 1294. https://doi.org/10.3389/fpsyg.2016.01294 [/mfn], a creature that sits on a person’s chest while they sleep
- In United States, the phenomenon is commonly associated with aliens from outer space, UFOs and abductions
- Sleep paralysis is similar to the phenomenon known as kana tevoro in Fiji
- It is also associated with the Turkish folklore Karabasan, tales of demonic visitation while a person sleeps
- Thai folklore identifies the condition as Phi Am and is believed to be caused by a ghost
- Sleep paralysis is called gawi nulim in Korean culture
- Indian folklore attributes the phenomenon to supernatural events and is known by a variety of names such as shaitan, sayaa, pasikdhar, boba, Othada Thuliyodhu, Amuku Be etc.
As the sufferer often experiences a strong spiritual presence, many scientists believe that the episodes can explain certain reports of paranormal phenomena, like demons, ghosts [mfn] Jalal, B., Romanelli, A. & Hinton, D.E. Cultural Explanations of Sleep Paralysis in Italy: The Pandafeche Attack and Associated Supernatural Beliefs. Cult Med Psychiatry 39, 651–664 (2015). https://doi.org/10.1007/s11013-015-9442-y [/mfn], shadow people, the night hag and alien abductions.
Symptoms Of Sleep Paralysis
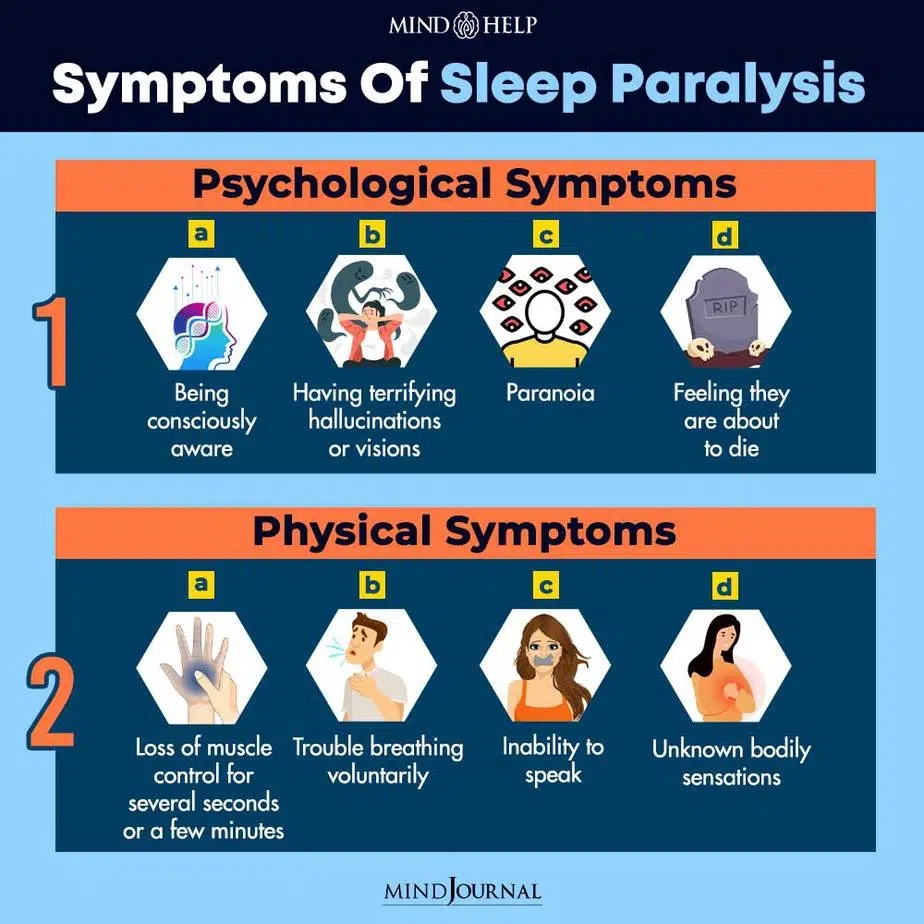
Although it is not considered as a medical emergency that requires immediate treatment, identifying the symptoms can help the sufferer to gain scientific knowledge about their condition, overcome superstitious beliefs and seek medical help, if necessary. Inability to move, breathe or speak voluntarily while falling asleep or waking up are perhaps the most common signs of sleep paralysis. Here are some other common psychological and physical symptoms of this type of parasomnia:
1. Psychological Symptoms
- Being consciously aware
- Having terrifying hallucinations or visions
- Paranoia
- Feeling they are about to die
- Feeling an evil entity is present in the room
- Seeing demonic beings, ghost or shadowy creatures
- Hearing unexplainable sounds
- Intense fears and anxiety
2. Physical Symptoms
- Loss of muscle control for several seconds or a few minutes
- Trouble breathing voluntarily
- Inability to speak
- Unknown bodily sensations
- Feeling a heavy pressure on chest
- Sweating
- Headaches
- Muscle aches
- Weakness
General sensations, sounds and stimuli, which are typically non-threatening, may become disproportionately exaggerated during an event. Episodes usually tend to end naturally or it may resolve when someone else physically touches the sufferer. The patient may also be able to remember details of the experience after the episode is over. It can even make them afraid of the dark and be afraid of falling asleep alone due to severe anxiety. However, these hallucinations are usually harmless.
Causes Of Sleep Paralysis
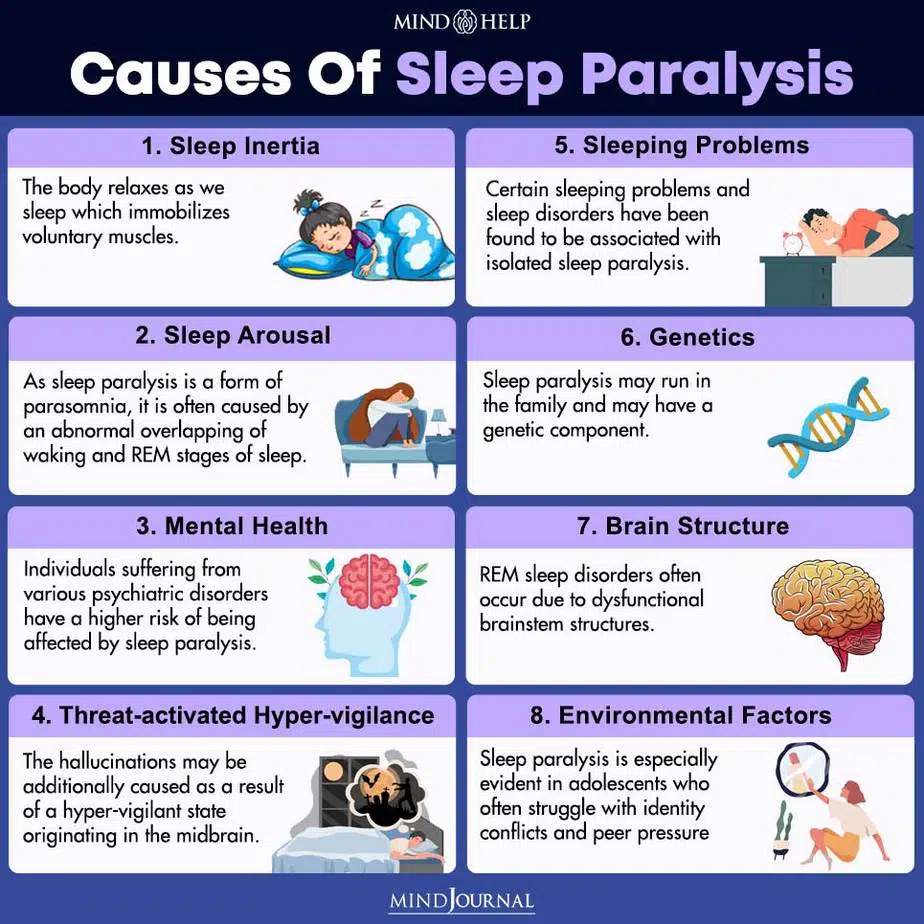
The exact causes for the development of sleep paralysis has not yet been properly identified yet. However, researchers believe there are several factors that may lead to the onset of this condition. The National Health Service (NHS) [mfn] Sleep paralysis. 2017. nhs.uk. https://www.nhs.uk/conditions/sleep-paralysis/[/mfn], UK, explains that the experience “happens when you cannot move your muscles as you are waking up or falling asleep. This is because you are in sleep mode but your brain is active.”
Recent studies [mfn] Lišková, M., Janečková, D., Klůzová Kráčmarová, L., Mladá, K., & Bušková, J. (2016). The occurrence and predictive factors of sleep paralysis in university students. Neuropsychiatric disease and treatment, 12, 2957–2962. https://doi.org/10.2147/NDT.S115629 [/mfn] have shown nightmares tend to be the strongest predictive factor to understand the frequency of episodes, while dream occurrences help to predict the intensity of fear experienced by the sufferer.
Here are some of the most common factors that may result in this condition in someone:
1. Sleep Inertia
The body relaxes as we sleep which immobilizes voluntary muscles. When we go through a REM state of sleep and dreams occur, this prevents us from acting out our dreams and prevents us from injuring ourselves. But when someone gains conscious awareness before the completion of the 90-minute REM cycle, they can experience paralysis unless the brain decides to release the muscles and make them available for voluntary movement. There is no supernatural cause for its occurrence.
2. Sleep Arousal
As sleep paralysis is a form of parasomnia, it is often caused by an abnormal overlapping of waking and REM stages of sleep. A 2014 [mfn] Fleetham, J. A., & Fleming, J. A. (2014). Parasomnias. CMAJ : Canadian Medical Association journal = journal de l’Association medicale canadienne, 186(8), E273–E280. https://doi.org/10.1503/cmaj.120808 [/mfn] review shows that sleep paralysis, along with sleep terrors, sleep talking and sleepwalking, are behavioral manifestations related to the “partial arousals from sleep known as parasomnias – a group of sleep disorders defined as undesirable physical events or experiences that occur during the initiation of sleep, during sleep or during arousal from sleep.”
Research [mfn] Walther, B.W., Schulz, H. Recurrent isolated sleep paralysis: Polysomnographic and clinical findings. Somnologie 8, 53–60 (2004). https://doi.org/10.1111/j.1439-054X.2004.00017.x [/mfn] also reveals that sufferers tend to have shorter REM sleep recesses than usual. Moreover, they also experience disturbed REM sleep as well as shorter REM and NREM sleep cycles. This indicates that fragmentation of normal sleeping patterns may trigger an episode of this condition. Researchers now believe that fragmented REM sleep occurs along with sleep paralysis.
Daniel Denis, a postdoctoral scholar in psychiatry, explains, “We know the amygdala is highly active in REM, which is important to fear and emotional memory. You have a part of the brain that is actively responding to fear or something emotionally charged, but there is nothing in the environment to account for it. So the brain devises a solution to the paradox. ” However, the cause of hallucinations is unknown.
3. Mental Health
A 2018 study [mfn] Singh, S., Kaur, H., Singh, S., & Khawaja, I. (2018). Parasomnias: A Comprehensive Review. Cureus, 10(12), e3807. https://doi.org/10.7759/cureus.3807 [/mfn] discovered that specific mental health conditions can be associated with sleep paralysis. Individuals suffering from various psychiatric disorders have a higher risk of being affected by this condition and experiencing multiple episodes. These may include conditions like –
- Narcolepsy
- Post-traumatic stress disorder (PTSD)
- Major depression
- Bipolar disorder
- Generalized Anxiety Disorder
- Anxiety disorders
- Panic disorder
- Hypertension
- Seizure disorders
Apart from these, childhood abuse, sexual abuse and emotional and physical distress can also be contributing factors. “Stopping alcohol or antidepressants can also cause REM rebound, which can result in sleep paralysis,” explains the SleepFoundation. Moreover, experiences related to daydreaming, dissociation from the present environment or being creative and imaginative can also lead to the development of this condition. Sleep paralysis may also be associated with lucid dreaming [mfn] Denis, D., & Poerio, G. L. (2017). Terror and bliss? Commonalities and distinctions between sleep paralysis, lucid dreaming, and their associations with waking life experiences. Journal of sleep research, 26(1), 38–47. https://doi.org/10.1111/jsr.12441 [/mfn] and vivid nightmares.
Read More About Post-Traumatic Stress Disorder (PTSD) Here
4. Threat-activated Hyper-vigilance
The hallucinations may be additionally caused as a result of a hyper-vigilant state [mfn] J.Allan Cheyne, Steve D. Rueffer, Ian R. Newby-Clark, Hypnagogic and Hypnopompic Hallucinations during Sleep Paralysis: Neurological and Cultural Construction of the Night-Mare, Consciousness and Cognition, Volume 8, Issue 3, 1999, Pages 319-337, ISSN 1053-8100, https://doi.org/10.1006/ccog.1999.0404. [/mfn] originating in the midbrain. When someone awakens in a paralyzed state, the emergency response gets triggered as they feel threatened. This sense of being vulnerable can augment the impact of the threat response [mfn] Hypnagogic and hypnopompic hallucinations during sleep paralysis: Neurological and cultural construction of the nightmare. (n.d.). ScienceDirect.com | Science, health and medical journals, full-text articles and books. https://www.sciencedirect.com/science/article/abs/pii/S105381009990404X?via%3Dihub [/mfn]. This can influence dreams and make visions feel so vivid during an episode. This vigilance system activated by threats is primarily a defensive mechanism that distinguishes threatening situations and regulates the fear response.
The process can also help to explain the feelings of an evil presence trying to strangle or suffocate the victim. From a neurological perspective, muscle paralysis combined with a threat vigilance activation system during sleep paralysis can explain such terrifying and supernatural experiences as it affects the voluntary control of our breathing. This is also associated with the feelings of a demonic entity sitting on their abdomen or chest and suffocating them. This may result in feelings of entrapment making the sufferer struggle harder to overcome the episode.
5. Sleeping Problems
Certain sleeping problems and sleep disorders have been found to be associated with isolated sleep paralysis. Around 38% of people [mfn] Hsieh, S. W., Lai, C. L., Liu, C. K., Lan, S. H., & Hsu, C. Y. (2010). Isolated sleep paralysis linked to impaired nocturnal sleep quality and health-related quality of life in Chinese-Taiwanese patients with obstructive sleep apnea. Quality of life research: an international journal of quality of life aspects of treatment, care and rehabilitation, 19(9), 1265–1272. https://doi.org/10.1007/s11136-010-9695-4 [/mfn] with obstructive sleep apnea (OSA), a condition resulting in persistent breathing problems during sleep, experience higher levels of sleep paralysis. Moreover, individuals suffering from nighttime leg cramps are also more likely to experience this condition.
Most symptoms associated with insomnia or excessive daytime sleepiness are also observed in people suffering from this condition. According to the SleepFoundation, sufferers “whose circadian rhythms are not aligned with their local day-night cycle, such as people with jet lag and shift workers,” are also more likely to experience such episodes.
6. Genetics
Recent research [mfn] Suni, E. (2020, August 6). What you should know about sleep paralysis. Sleep Foundation. https://www.sleepfoundation.org/parasomnias/sleep-paralysis [/mfn] shows that sleep paralysis may run in the family and may have a genetic component. Individuals with a family history of the condition are more likely to experience it. As parasomnias have a heritable element regarding the fragmentation of REM sleep, hypnagogic and hypnopompic hallucinations, it is believed that sleep paralysis can also be genetic.
The research also reveals that twin studies conducted on identical twins found evidence that if one twin experiences the condition then the other twin has an extremely high chance of experiencing an episode as well. The genetic nature of the disorder indicates that a physiological dysfunction may be a significant contributing factor. However, researchers are yet to identify a specific genetic basis for this.
7. Brain Structure
According to one study [mfn] Olunu, E., Kimo, R., Onigbinde, E. O., Akpanobong, M. U., Enang, I. E., Osanakpo, M., Monday, I. T., Otohinoyi, D. A., & John Fakoya, A. O. (2018). Sleep Paralysis, a Medical Condition with a Diverse Cultural Interpretation. International journal of applied & basic medical research, 8(3), 137–142. https://doi.org/10.4103/ijabmr.IJABMR_19_18 [/mfn], REM sleep disorders often occur due to dysfunctional brainstem structures [mfn] Iranzo, A., Graus, F., Clover, L., Morera, J., Bruna, J., Vilar, C., Martínez-Rodriguez, J. E., Vincent, A., & Santamaría, J. (2006). Rapid eye movement sleep behavior disorder and potassium channel antibody-associated limbic encephalitis. Annals of neurology, 59(1), 178–181. https://doi.org/10.1002/ana.20693 [/mfn]. Moreover, brainstem activation of the amygdala may also result in sensing the presence of an intruder in the room and exaggerated awareness of danger.
The study states “The lateral amygdala sends impulses to the rest of the basolateral complexes. This is preceded by activation of the amygdala via projections from the thalamus, anterior cingulate, and pons structures. This gives the individual the idea that an intruder is in the room.” The limbic system can also play a crucial role in REM dreams.
8. Environmental Factors
Sleep paralysis is especially evident in adolescents who often struggle with identity conflicts and peer pressure. This, along with the pressures of academic performance, can lead to severe anxiety and depression during the developmental phase. About 70% of Czech students [mfn] Cheyne, J. A., & Pennycook, G. (2013). Sleep Paralysis Postepisode Distress: Modeling Potential Effects of Episode Characteristics, General Psychological Distress, Beliefs, and Cognitive Style. Clinical Psychological Science, 1(2), 135–148. https://doi.org/10.1177/2167702612466656 [/mfn] experience this phenomenon.
Studies [mfn] Otto, M. W., Simon, N. M., Powers, M., Hinton, D., Zalta, A. K., & Pollack, M. H. (2006). Rates of isolated sleep paralysis in outpatients with anxiety disorders. Journal of anxiety disorders, 20(5), 687–693. https://doi.org/10.1016/j.janxdis.2005.07.002 [/mfn] have also observed that African Americans are more likely to experience the condition as compared to other ethnic groups. Another study [mfn] Jalal, B., & Hinton, D. E. (2013). Rates and characteristics of sleep paralysis in the general population of Denmark and Egypt. Culture, medicine and psychiatry, 37(3), 534–548. https://doi.org/10.1007/s11013-013-9327-x [/mfn] revealed that people of Asian and African descent experienced the highest rate of episodes.
9. Other Factors
There may be some other general factors that may increase a person’s chances of experiencing an episode. These may include factors like –
- Unhealthy sleeping habits
- Poor sleep hygiene
- Changes in sleep schedule
- Sleep disorders, such as narcolepsy or sleep apnea
- Sleeping on the back
- Sleep related leg cramps
- Mental stress
- Migraines
- Poor physical health
- Other medical conditions
- Substance abuse
- Medication use
- Traumatic life events
- Student status and occupation
Further research is required to properly understand the numerous and exact causes of the condition and these correlations.
Is Sleep Paralysis A Serious Condition?
Generally, it is not a serious medical condition as sleep paralysis is usually harmless. The phenomenon is not experienced too frequently by sufferers to result in serious health issues. Hence, it is categorized as a benign condition. However, around 10% of sufferers tend to have repetitive and difficult episodes that can make the whole experience distressing and lead to intense stress, anxiety and even depression.
These patients may have a negative perspective about sleeping and may avoid sleeping alone or staying in the dark during bedtime. They may also avoid sleeping or sleep for a limited period of time. Moreover, anxiety may also make it harder for them to fall asleep and adversely affect their quality of sleep. Anxiety and sleep deprivation may lead to several significant mental and physical health risks and problems.
Diagnosis Of Sleep Paralysis
Medical tests are usually not required to diagnose this condition. However, a healthcare professional may conduct a clinical interview or some lab tests to determine if the symptoms are caused by any other physical or mental health condition. There are a number of reliable screening tests available, like the Munich Parasomnia Screening (MUPS) [mfn] Fulda, S., Hornyak, M., Müller, K. et al. Development and validation of the Munich Parasomnia Screening (MUPS). Somnologie 12, 56–65 (2008). https://doi.org/10.1007/s11818-008-0336-x [/mfn] questionnaire, for the diagnosis of recurrent isolated sleep paralysis (RISP).
The International Classification of Sleep Disorders (ICSD)-3[mfn] Sharpless B. A. (2016). A clinician’s guide to recurrent isolated sleep paralysis. Neuropsychiatric disease and treatment, 12, 1761–1767. https://doi.org/10.2147/NDT.S100307 [/mfn] identifies the condition as a formal diagnosis. But there is no specific diagnostic code for this phenomenon. Moreover, the International Statistical Classification of Diseases and Related Health Problems (ICD) [mfn] The international statistical classification of diseases and related health problems [/mfn] and the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) also lack any diagnostic criteria for sleep paralysis. However, RISP can be categorized and diagnosed as an unspecified sleep-wake disorder or other specified sleep-wake disorder.
As it is often difficult to differentiate between sleep paralysis and cataplexy [mfn] Mirabile VS, Sharma S. Cataplexy. [Updated 2021 Jun 26]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK549782/ [/mfn] caused by narcolepsy, doctors should be careful while diagnosing and treating patients. Differential diagnosis may also include certain similar conditions like –
- Sleep terrors (STs)
- Nightmare disorder (ND)
- Nocturnal panic attacks (NPAs)
- Exploding head syndrome (EHS)
- Posttraumatic stress disorder (PTSD)
When To See A Doctor
As sleep paralysis is usually not regarded as a medical diagnosis, medical attention may not be required in most cases. However, if the symptoms become too severe or if it leads to intense anxiety, fear and depression, then consulting a doctor for a formal diagnosis can be a good idea. A healthcare professional can provide helpful advice on how to manage the symptoms and overcome the condition.
Seeing a doctor may be important when:
- Episodes occur almost on a daily basis
- The sufferer is afraid or feel anxious about going to sleep
- They suffer from insomnia or have trouble falling asleep
- They suddenly fall asleep during the day
- They feel chronic fatigue
Falling asleep suddenly may indicate the development of narcolepsy. It may also be important to seek treatment for stress and anxiety associated with the condition. The doctor may interview the patient about their medical history and sleeping patterns. The sufferer may also be asked to journal their episodes to document them properly. In rare cases, the doctor may also conduct an overnight sleep study to diagnose the patient effectively.
Treatment Of Sleep Paralysis
Most individuals experiencing isolated episodes of sleep paralysis do not usually need any treatment as symptoms tend to resolve within minutes. Isolated episodes don’t result in any lasting trauma or physical effects, even though it may be exceptionally frightening and unsettling for the sufferer. However, repeated episodes may require medical attention to treat any underlying conditions, such as narcolepsy.
This is especially important if the experiences affect the person’s education, career, relationships and personal life. But most sufferers often feel hesitant about seeking help. “There is limited scientific evidence about the optimal treatment for sleep paralysis. Many people are unaware that the condition is relatively common, and as a result, they perceive themselves as crazy or shameful after episodes,” explains the SleepFoundation.
Educating the patient about sleep stages and atonia [mfn] Berger A. J. (2008). What causes muscle atonia in REM?. Sleep, 31(11), 1477–1478. https://doi.org/10.1093/sleep/31.11.1477 [/mfn] during REM sleep is the first and most crucial phase of medical treatment. Adopting healthier sleeping habits and lifestyle is highly recommended for overcoming the symptoms. However, for more severe cases, the following treatment options may be prescribed by healthcare professionals:
1. Therapy
Cognitive-behavioral therapy (CBT) can substantially help in treating patients with sleep paralysis. A culturally adapted form of CBT (CA-CBT) for PTSD can help in improving terrifying situations related to attacks by emphasizing psycho-education. Culturally Adapted CBT (CA-CBT) [mfn] Adaptation of CBT for traumatized egyptians: Examples from culturally adapted CBT (CA-CBT). (n.d.). ScienceDirect.com | Science, health and medical journals, full text articles and books. https://www.sciencedirect.com/science/article/abs/pii/S1077722916300049?via%3Dihub [/mfn] has previously proven to be effective in treating traumatized Egyptian patients with this condition. Research [mfn] Sharpless B. A. (2016). A clinician’s guide to recurrent isolated sleep paralysis. Neuropsychiatric disease and treatment, 12, 1761–1767. https://doi.org/10.2147/NDT.S100307 [/mfn] also indicates that CBT can also help to prevent and disrupt episodes in sufferers. CBT may include –
- Sleep paralysis specific sleep hygiene
- Relaxation techniques for RISP episodes
- In vivo episode disruption methods
- Coping strategies for frightening hallucinations
- Disputation of terrifying thoughts
- Imaginary rehearsal of effective resolutions
Treatment may also include the following cognitive-behavioral techniques [mfn] Galbiati, A., Rinaldi, F., Giora, E., Ferini-Strambi, L., & Marelli, S. (2015). Behavioural and Cognitive-Behavioural Treatments of Parasomnias. Behavioural neurology, 2015, 786928. https://doi.org/10.1155/2015/786928 [/mfn] –
- Imagery rehearsal therapy (IRT)
- Exposure techniques
- Exposure, relaxation, and rescripting therapy (ERRT)
- Lucid dreaming therapy (LDT)
- Hypnosis
- Eye movement desensitization and reprocessing (EMDR)
Apart from these, cognitive-behavior therapy for isolated sleep paralysis (CBT-ISP) may also be recommended for psychoeducation, cognitive restructuring of thoughts and self-analysis of symptoms. Moreover, a new psychotherapeutic approach involving relaxation and meditation has also been found to be helpful in relieving symptoms. A recent study on the effectiveness of Focused-Attention Meditation Combined with Muscle Relaxation (MR Therapy [mfn] Jalal B. (2016). How to Make the Ghosts in my Bedroom Disappear? Focused-Attention Meditation Combined with Muscle Relaxation (MR Therapy)-A Direct Treatment Intervention for Sleep Paralysis. Frontiers in psychology, 7, 28. https://doi.org/10.3389/fpsyg.2016.00028 [/mfn] ) has yielded “positive preliminary results.”
2. Medications
Although there are no specific medicines [mfn] Stores G. (2003). Medication for sleep-wake disorders. Archives of disease in childhood, 88(10), 899–903. https://doi.org/10.1136/adc.88.10.899 [/mfn] for the treatment of this condition, certain medications may help to relieve some of the symptoms. Antidepressant medication can help with managing depression and regulating sleep cycles. According to the NHS, UK “You might be given medicine usually used to treat depression.
Taking this type of medicine at a lower dose can also help with sleep paralysis.” For severe cases, selective serotonin reuptake inhibitors (SSRIs) and tricyclic antidepressants may also be prescribed as these help in the suppression of REM sleep.
Studies have found that Gamma-Hydroxybutyric acid (GHB) can help reduce episodes in people with narcolepsy. Moreover, Pimavanserin [mfn] Jalal, B. The neuropharmacology of sleep paralysis hallucinations: serotonin 2A activation and a novel therapeutic drug. Psychopharmacology 235, 3083–3091 (2018). https://doi.org/10.1007/s00213-018-5042-1 [/mfn] has also shown promise in treating the symptoms; however, future research may be required. It should be noted that even though these medications may help in relieving symptoms, currently there is no medication that can interrupt episodes completely.
3. Sleep Study
In some cases of sleep paralysis, a sleep study may be recommended by the doctor. Known as polysomnography (PSG), it is primarily a systematic procedure that helps in assimilating physiologic parameters during the stages of sleep. The process uses pulse oximetry, electrooculogram, electrocardiogram, electroencephalogram, electromyogram and respiratory effort to analyze if there are any underlying factors resulting in sleep disturbances. According to a recent 2019 study [mfn] Rundo, J. V., & Downey, R., 3rd (2019). Polysomnography. Handbook of clinical neurology, 160, 381–392. https://doi.org/10.1016/B978-0-444-64032-1.00025-4 [/mfn], “PSG is considered to be the gold standard for diagnosing sleep-related breathing disorders,” such as –
- Narcolepsy
- Obstructive sleep apnea (OSA)
- Central sleep apnea
- Rapid eye movement sleep behavior disorder
- Periodic limb movement disorder
- Nocturnal seizures
- Sleep-related hypoventilation/hypoxia
The results of the sleep study can enable doctors to make a more accurate diagnosis for sleep paralysis and narcolepsy. It may require the patient to stay overnight at a sleep center or hospital to conduct the polysomnography. The study usually measures brain waves, muscle activity, breathing rate, heart rate and movements during sleep.
Prevention For Sleep Paralysis
Sleep paralysis can be prevented once the causes and contributing factors are identified. By identifying these factors, a sufferer can remove the triggers and start reducing the symptoms and episodes. Moreover, by incorporating self-help strategies and sleep hygiene improvement practices, a patient can successfully overcome the condition and the symptoms may disappear eventually. For people suffering with other mental health conditions along with sleep paralysis, medical treatment can prove to be highly effective.
Self-help Strategies To Improve Sleep Hygiene
Although sleep paralysis episodes can be terrifying, you can overcome them by improving your sleeping habits and taking certain steps at home. According to SleepFoundation, because of the “connection between sleep paralysis and general sleeping problems, improving sleep hygiene is a common focus in preventing sleep paralysis.”
Sleep hygiene is a term that refers to certain daily habits and bedroom settings that impact your sleep quality. Here are some self-help strategies that can significantly help in improving sleep hygiene, relieving symptoms and coping with the condition:
1. Things To Do:
- Learn about the physiology of sleep and the sleep paralysis mechanism
- Get enough, good quality sleep for at least 6-8 hours of sleep every day
- Create a relaxing environment at home
- Wear comfortable clothing at night
- Maintain a proper sleep schedule on a daily basis, including a consistent bedtime and wake-up time
- Maintain a low room temperature during bedtime
- Sleep on a comfortable mattress and pillow
- Create a calming bedtime ritual, like listening to relaxing music or reading
- Make sure to leave your devices, like smartphones and laptops, outside your bedroom
- Exercise regularly but not before bedtime
- Take steps to manage and reduce stress in life
- Learn about the medications you take and their potential side effects
- Get adequate daylight exposure during waking hours
- Practice mindfulness meditation regularly
- Focus on managing your anxiety or depression, if any
2. Things To Avoid:
- Avoid sleeping on your back
- Avoid blue light (e.g. smartphones or TV) before bedtime
- Avoid studying or working in the bedroom
- Avoid eating heavy dinners or evening meal at least 2 hours before sleep
- Avoid using any gadgets or social media at least 1 hour before sleeping
- Avoid strong lights before bedtime and use night-lights for bathroom trips
- Avoid siestas or mid-day naps over 90 minutes, especially after 3pm
- Avoid consuming alcohol, nicotine or caffeine before sleeping
“Getting enough sleep may reduce the likelihood of experiencing sleep paralysis,” explains Healthdirect, Australia. It adds “Keeping to a regular sleeping pattern by going to bed around the same time each night may also help.” However, if the above-mentioned self-help strategies do not improve the symptoms, then it is best to consult a doctor.
Sleep Paralysis Is Curable
Contrary to cultural beliefs, sleep paralysis is not about demonic attacks or alien abductions. It is a type of parasomnia and sleep problem that is often associated with narcolepsy. With proper treatment, medications and better sleep hygiene practices you can prevent paralysis from occurring during sleep and get good quality rest.
Understanding the condition and seeking professional help is necessary for managing the symptoms and improving your overall health and wellness.
Sleep Paralysis At A Glance
- Sleep paralysis is a feeling of being unable to move
- This is a common sleep problem and is a form of parasomnia.
- This can be observed in seemingly healthy individuals or in people with narcolepsy.
- This can result in vivid, multisensorial waking nightmares and hallucinations while transitioning from sleeping to waking and vice versa.
- Medical tests are usually not required to diagnose this condition.
- Sleep paralysis can be prevented once the causes and contributing factors are identified.
- Understanding the condition and seeking professional help is necessary for managing the symptoms and improving your overall health and wellness.





Leave a Reply