Pyromania is a mental health condition characterized by the incessant urge to deliberately start fires. This act is conducted to relieve stress or for instant gratification.
What Is Pyromania?
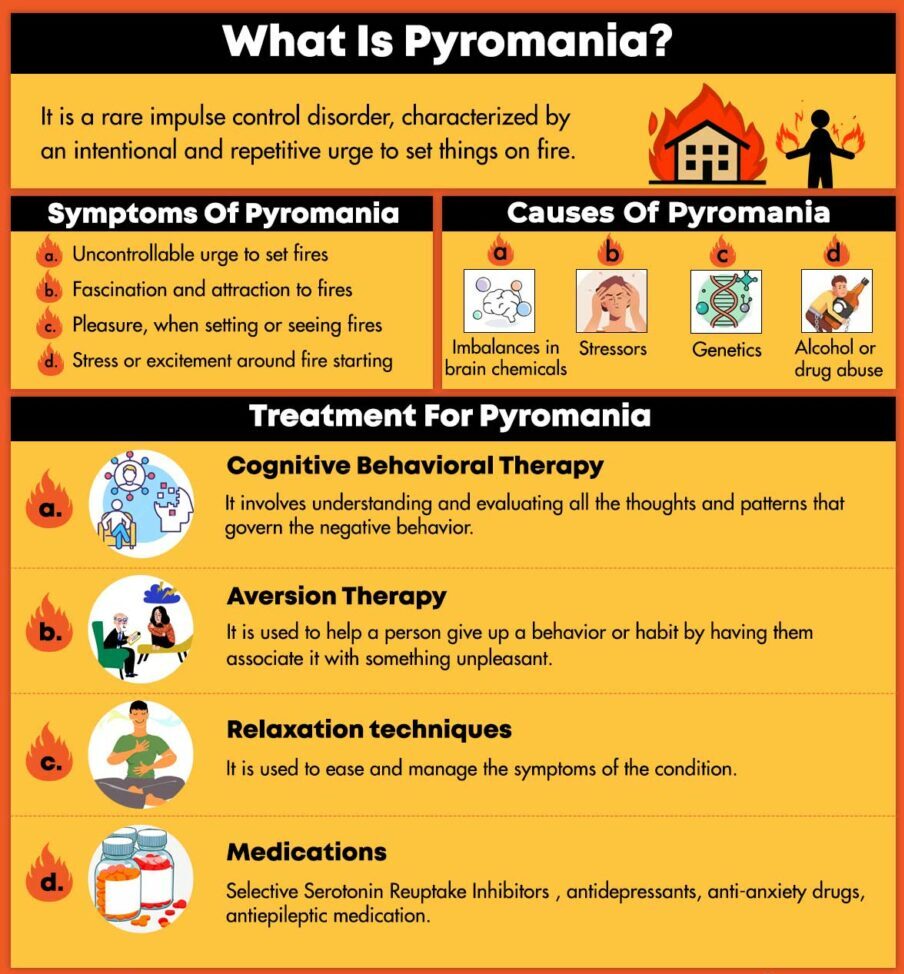
Pyromania is a rare impulse control disorder, characterized by an intentional and repetitive urge to set things on fire. The term pyromania derived from the Greek word “pyr” meaning “fire”. This condition is often confused with arson behavior. As this condition is an impulse control disorder, it may often be difficult for the sufferer to control their destructive urge or resist their impulse to set things on fire. Mindsjournal explains that people with this condition “have an exceptionally strong interest in fire and are continually unable to resist their impulse for setting things on fire & watching them burn.”
Pyromaniacs often behave in such destructive manner without any probable personal, monetary or other motivations. They tend to feel high levels of anxiety before engaging in the destructive act but experience intense gratification and pleasure after starting the fire.
Understanding Pyromania
A 2017 report (Fire Setting and the Impulse-Control Disorder of Pyromania) suggests that a person with this condition tends to start fires at a frequency of every six weeks. One 2012 study (Firesetting, Arson, Pyromania, and the Forensic Mental Health Expert) has found that 90% of people report severe distress after starting fires, and one third, having considered suicide as a way to control firesetting behavior.
Another 2009 report (Prevalence and Correlates of Fire-Setting in the United States: Results from the National Epidemiologic Survey on Alcohol and Related Conditions ) [mfn] Vaughn, M. G., Fu, Q., Delisi, M., Wright, J. P., Beaver, K. M., Perron, B. E., & Howard, M. O. (2010). Prevalence and correlates of fire-setting in the United States: results from the National Epidemiological Survey on Alcohol and Related Conditions. Comprehensive psychiatry, 51(3), 217–223. https://doi.org/10.1016/j.comppsych.2009.06.002 [/mfn] confirmed the prevalence rate of this condition to be 1% of the U.S. population. A 2013 study (Self-reported juvenile firesetting: results from two national survey datasets) found that when researchers examined people in the criminal system who had displayed fire setting behaviors found that 3.3% of that population met the criteria for pyromania.
As pyromania is a rare disorder, it is often difficult to determine the prevalence and incidence. However, a 2015 research [mfn] Palermo, G. B. (2015). A look at Firesetting, arson, and pyromania. International Journal of Offender Therapy and Comparative Criminology, 59(7), 683-684. https://doi.org/10.1177/0306624×15586217 [/mfn] indicates that around 3%-6% of individuals in inpatient psychiatric hospitals tend to meet the diagnostic criteria. Moreover, the condition is more common in males than in females. Since it is a rare disorder, treatment for pyromania varies according to the individual. Certain medications do not respond well, especially in comorbid conditions. If an individual is experiencing symptoms, it is important to seek immediate treatment.
Pyromaniacs Vs Arsonists
Although most people tend to confuse arsonists with pyromaniacs, there is a huge difference between the two. Arsonists tend to set fire to things and properties for personal, monetary, or political gain. Pyromaniacs start fires for the euphoria that comes with it. Pyromania is a psychiatric condition that interferes with impulse control. On the other hand, arson is a criminal act that is done intentionally.
Although pyromania and arson are both intentional, the former is strictly pathological or compulsive while the latter isn’t. An arsonist can have pyromania but vice versa may not be true. They may have other diagnosable mental health conditions. Pyromaniacs may not commit an act of arson. However, they may start fires in a way that isn’t considered a criminal offense.
There are also specific symptoms that separate pyromaniacs from arsonists. Someone suffering from pyromania tends to set fire for more than one occasion. They feel extreme stress before conducting the act and relief of stress after setting the fire. When seeing fires, the person with this condition gains intense interest or fascination. Pyromaniacs may also experience pleasure, gratification, or relief after conducting the act. The most essential feature of pyromania is the presence of multiple episodes of intentional and purposeful fire setting.
Pyromania In Children
Reports (Impulse Control Disorders: Intermittent Explosive Disorder, Kleptomania, and Pyromania) suggest that the onset of this condition can occur as early as age 3. This condition is often diagnosed around the age of 18. Fire starting behavior can occur in children for various reasons that may not be related to pyromania. In most cases, children or adolescents tend to experiment or are curious about lighting fires or playing with matches. It is known as a “curiosity fire setting” and is considered a normal part of development.
In case setting fires becomes an issue or they have an intention to cause serious damage, it’s often found to be a symptom of another condition such as attention deficit hyperactivity disorder (ADHD) or conduct disorder and not pyromania.
Read More About Post-Traumatic Stress Disorder In Children Here
Symptoms Of Pyromania
The symptoms usually start during puberty and can last until adulthood. Someone with pyromania seems to be obsessed with fire and fire fighting, frequently visiting fire departments, watching fires, helping out after a fire, and even setting off false fire alarms.
The signs and symptoms of this debilitating condition include:
- An uncontrollable urge to set fires
- Fascination and attraction to fires and its paraphernalia
- Pleasure, a rush or relief when setting or seeing fires
- Stress or excitement around fire starting
- Purposely setting more than one fire
- Burning holes in fabrics and rugs
- Burnt pieces of paper or other material in garbage cans or near a sink or stove
Moreover, fires are not set due to monetary gains or improving one’s circumstances, ideological reasons, to cover up criminal activity, express anger or revenge, as a result of a delusion, hallucination, or impaired judgement
Causes Of Pyromania
The exact cause of this condition is unknown. It may be related to certain mental health conditions or related to imbalances in brain chemicals, stressors, or genetics. Research on the influence of genetic factors is limited. Impulsivity is considered to be heritable. A study [mfn] Bezdjian, S., Baker, L. A., & Tuvblad, C. (2011). Genetic and environmental influences on impulsivity: a meta-analysis of twin, family and adoption studies. Clinical psychology review, 31(7), 1209–1223. https://doi.org/10.1016/j.cpr.2011.07.005 [/mfn] reports that researchers have been motivated to attain a deeper understanding of underlying genetic predispositions that affect impulsivity.
Impulsivity is an essential component in normal varying personality as well as pathological behaviors. This means that there may be a genetic component involved in developing this disorder. The neurotransmitters, dopamine, and serotonin that are responsible for impulse control may be influenced by genes.
Other causes can include:
- Getting diagnosed with another mental health condition such as a conduct disorder
- A history of abuse or neglect during childhood
- Alcohol or drug abuse
- Deficits in social skills or intelligence
Comorbid Conditions Associated Pyromania
A 2007 study (Clinical characteristics and psychiatric comorbidity of pyromania [mfn] Grant JE, Won Kim S. Clinical characteristics and psychiatric comorbidity of pyromania. J Clin Psychiatry. 2007 Nov;68(11):1717-22. doi: 10.4088/jcp.v68n1111. PMID: 18052565. [/mfn] ) has found high comorbid rates associated with pyromania. They are as follows
- Mood disorders (61.9%)
- Substance use disorders(33.3%)
- Anxiety disorders (33.3%)
- Impulse control disorders (66.7%)
- Gambling disorder
- Antisocial personality disorder
Diagnosis Of Pyromania
The Diagnostic and Statistical Manual of Mental Disorders (DSM 5) recognized this condition as an “impulse control disorder”. Impulse control disorder is a condition characterized by the inability to resist a destructive or impulsive urge. This condition is rarely diagnosed. In order to be diagnosed with pyromania, the individual must:
- Purposefully sets fires on more than one occasion
- Experiencing tension before setting fires and a release after conducting the act
- Having an intense attraction to fire and its paraphernalia
- Experiencing pleasure from setting or seeing fires
- Having symptoms that aren’t better explained by another mental disorder such as Conduct disorder, Manic episode, Antisocial personality disorder
A person can only be diagnosed with this condition when they don’t set fires:
- For any external motivations like money
- For ideological reasons
- To express anger or vengeance
- To cover up another criminal act
- To improve one’s circumstances (for instance getting insurance money to buy a better house)
- In response to hallucinations or delusions
- Impaired judgment such as being intoxicated
Treatment For Pyromania
If left untreated, this condition can be chronic. Immediate treatment is the key to avoid injury, property damage, jail time, or even death. Treatment can vary according to the severity of the symptoms. The treatment options can be a combination of medication and therapy.
Some of the common treatment options available for pyromania include:
1. Cognitive Behavioral Therapy
Cognitive Behavioral Therapy (CBT) involves understanding and evaluating all the thoughts and patterns that govern the negative behavior. These thoughts and patterns are then replaced with positive thoughts and patterns to reach the desired outcome. The therapist can also help to develop coping strategies to ease the symptoms of the condition. Evidence [mfn] Hofmann, S. G., Asnaani, A., Vonk, I. J., Sawyer, A. T., & Fang, A. (2012). The Efficacy of Cognitive Behavioral Therapy: A Review of Meta-analyses. Cognitive therapy and research, 36(5), 427–440. https://doi.org/10.1007/s10608-012-9476-1 [/mfn] suggests the efficacy of CBT in multi sessions vs single sessions and a lower drop out rate as compared to other forms of therapy.
Read More About Cognitive Behavioral Therapy Here
2. Aversion Therapy
This is a type of behavioral therapy that involves pairing an unwanted behavior with discomfort. During this therapy, the patient is exposed to experiencing the pleasure of lighting fires in controlled settings while simultaneously being subjected to some form of discomfort. The goal is to associate unwanted behaviors in unpleasant situations. A 2006 study [mfn] Grant, J. E., & Potenza, M. N. (2006). Compulsive aspects of impulse-control disorders. The Psychiatric clinics of North America, 29(2), 539–x. https://doi.org/10.1016/j.psc.2006.02.002 [/mfn] indicated that aversion therapy showed significant improvements in patients suffering from this condition.
3. Relaxation techniques
Relaxation techniques may be used to ease and manage the symptoms of the condition. These relaxation techniques include deep breathing exercises, mindful meditation, guided imagery, or progressive relaxation. A 2019 study [mfn] Ju, W., Ren, L., Chen, J., & Du, Y. (2019). Efficacy of relaxation therapy as an effective nursing intervention for post-operative pain relief in patients undergoing abdominal surgery: A systematic review and meta-analysis. Experimental and therapeutic medicine, 18(4), 2909–2916. https://doi.org/10.3892/etm.2019.7915 [/mfn] on relaxation therapy has been shown to provide pain relief by decreasing anxiety, lowering muscle tension and distracting attention. As skills in releasing tension in the local parts of the body is developed, the relaxation of the entire body becomes easier.
4. Medications
The doctor can prescribe medications to treat underlying conditions such as anxiety or depression. These medications can include Selective Serotonin Reuptake Inhibitors (SSRIs) or antidepressants, anti-anxiety drugs, antiepileptic medication, atypical antipsychotics, lithium, or anti-androgens. A 2007 study [mfn] Naltrexone in the treatment of pyromania. ClinicalTrials.gov. https://clinicaltrials.gov/ct2/show/record/NCT00467454?view=record [/mfn] evaluated the efficacy of naltrexone in patients with pyromania. The goal is to study the effectiveness of reducing the urges to set fires in patients with this disorder.
Recovery From Pyromania
This condition is rarely diagnosed. Although research is limited, the DSM 5 does recognize this condition as an impulse control disorder with specific diagnostic criteria. With therapy and medications, it is possible to treat and manage the symptoms of this disorder.






Leave a Reply