Bulimia nervosa is a complex and severe eating disorder characterized by a pattern of consuming excessive amounts of food, often referred to as binge eating, and subsequently engaging in behaviors to rid the body of the consumed food, known as purging. It is crucial to recognize that Bulimia nervosa is a serious condition with potentially life-threatening consequences.
What Is Bulimia Nervosa?
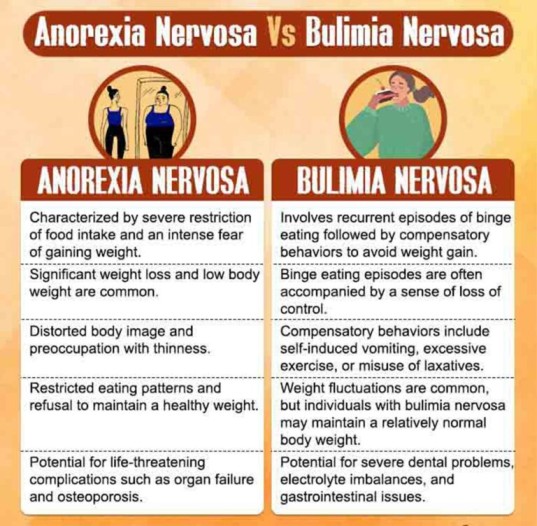
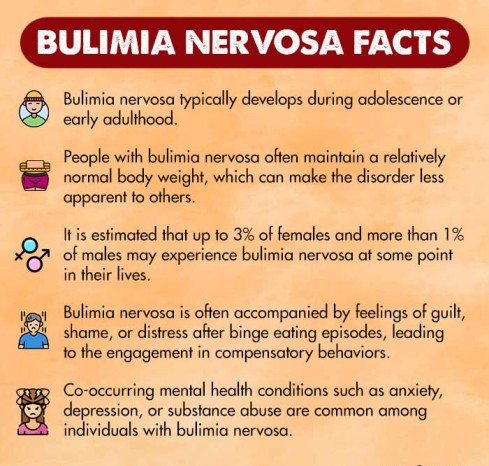
Bulimia nervosa is an eating disorder [mfn] Jain, A., & Yilanli, M. (2020). Bulimia Nervosa. PubMed; StatPearls Publishing. Available from: https://www.ncbi.nlm.nih.gov/books/NBK562178/ [/mfn] characterized by recurrent episodes of binge eating followed by compensatory behaviors to prevent weight gain. Individuals with bulimia nervosa often experience a loss of control during binge episodes, consuming large amounts of food within a short period, far exceeding what most people would eat in a similar timeframe.
They typically feel a sense of guilt, shame, or distress afterward, which leads them to engage in compensatory behaviors such as self-induced vomiting, excessive exercise, fasting, or misuse of laxatives or diuretics.
The characteristics of bulimia nervosa involve a cycle of secretive binge eating and subsequent attempts to purge the calories consumed. Binge eating episodes are often accompanied by a feeling of being out of control, while compensatory behaviors are driven by a desire to avoid weight gain or alleviate guilt.
Individuals with bulimia nervosa may place excessive importance on body shape and weight and have a distorted perception of their own bodies.
Case Example:
Rumi, a 19-year-old girl, grew up in a family where her parents compared her to her peers, especially regarding her beauty and appearance. As a result, she became increasingly self-conscious about her body and developed irregular eating patterns.
At times, she would consume large quantities of high-calorie foods within a short period, and to counterbalance this, she engaged in behaviors such as vomiting, excessive exercise, and experimented with laxatives and occasional fasting to manage her weight.
These behaviors gradually took a toll on Rumi’s physical health, leading to frequent stomach pain, acid reflux, and dental issues due to recurrent purging. Moreover, as her weight fluctuated, Rumi experienced profound feelings of guilt, shame, and a diminished sense of motivation in her daily life.
Case Analysis:
From the above case example, it can be observed that Rumi exhibits signs of uncontrollable urges to overeat by binge eating, i.e. consuming large amounts of food in a short timeframe.
She also displays secretive behaviors regarding her eating habits and follows compulsive patterns of exercise and diet, resorts to self-induced vomiting which negatively impacts her physical and emotional well-being. All of her behavior indicates that Rumi has significant symptoms of Bulimia Nervosa.
Symptoms Of Bulimia Nervosa
The signs and symptoms of bulimia nervosa can manifest both physically and behaviorally [mfn] Balasundaram, P., & Santhanam, P. (2021). Eating Disorders. PubMed; StatPearls Publishing. Available from: https://www.ncbi.nlm.nih.gov/books/NBK567717/ [/mfn] :
- Frequent fluctuations in weight
- Evidence of binge eating and purging methods (like vomiting)
- Swollen salivary glands
- Dental problems (such as tooth decay, gum disease, etc.)
- Acid reflux or other gastrointestinal issues
- Calluses or scars on the knuckles or hands (from self-induced vomiting)
- Dehydration and electrolyte imbalances
- Irregular menstrual periods or absence of menstruation (amenorrhea) in females
- Dry skin and brittle nails
- Fatigue and weakness
- Dizziness or fainting spells
- Obsession with body shape, weight, appearance, and dieting
- Compulsive exercising, even in adverse conditions or when injured
- Excessive focus on food, calories, and dieting
- Isolation or withdrawal from social activities, especially those involving food
- Mood swings, irritability, or depression related to body image or eating habits
- Secretive behavior around food and eating habits (related to overeating, restrictive food intake, or specified feeding)
Read More About Depression Here
Types Of Bulimia Nervosa
Bulimia nervosa is generally classified as a single disorder in diagnostic criteria, but there are different subtypes or variations [mfn] Administration, S. A. and M. H. S. (2016, June 1). Table 20, DSM-IV to DSM-5 Bulimia Nervosa Comparison. Www.ncbi.nlm.nih.gov. Available from: https://www.ncbi.nlm.nih.gov/books/NBK519712/table/ch3.t16/ [/mfn] that can be observed within the condition. These include:
1. Purging type
This is the most common subtype of bulimia nervosa. Individuals engage in self-induced vomiting or misuse of laxatives, diuretics, or enemas as a means to compensate for binge eating episodes.
2. Non-purging type
In this subtype, individuals use compensatory behaviors other than purging to counteract the effects of binge eating. These behaviors may include excessive exercise or fasting.
3. Low-frequency type
This subtype refers to individuals who experience infrequent binge eating and compensatory behaviors. They may exhibit milder symptoms and engage in the behaviors less often compared to other subtypes.
4. High-frequency type
Conversely, the high-frequency subtype involves individuals who experience frequent episodes of binge eating and engage in compensatory behaviors on a regular basis. This subtype often demonstrates more severe symptoms and a greater degree of impairment.
What Causes Bulimia Nervosa?
Research [mfn] Rikani, A. A., Choudhry, Z., Choudhry, A. M., Ikram, H., Asghar, M. W., Kajal, D., Waheed, A., & Mobassarah, N. J. (2013). A critique of the literature on etiology of eating disorders. Annals of neurosciences, 20(4), 157–161. https://doi.org/10.5214/ans.0972.7531.200409 [/mfn] attributes the common causes of bulimia nervosa to the following:
- Genetic predisposition to develop an eating disorder
- Family history of eating disorders
- Psychological factors (such as low self-esteem, perfectionism, body dissatisfaction, and distorted body image)
- Sociocultural factors (including societal pressure to achieve a certain body ideal, media influence, and cultural emphasis on thinness)
- Childhood trauma, abuse, or neglect
- Personal or family history of dieting or weight-related issues
- Neurobiological factors (including imbalances in neurotransmitters related to appetite regulation and mood)
- Co-occurring mental health conditions [mfn] Convertino, A. D., & Blashill, A. J. (2022). Psychiatric comorbidity of eating disorders in children between the ages of 9 and 10. Journal of child psychology and psychiatry, and allied disciplines, 63(5), 519–526. https://doi.org/10.1111/jcpp.13484 [/mfn] (such as anxiety, depression, etc.)
- Stressful life events, transitions, or major life changes
- Peer or social influence, particularly among individuals involved in sports or activities that prioritize appearance and weight control
How Does Bulimia Affect Your Mental Health?
Bulimia nervosa can arise from untreated mental health disorders and have a negative impact on mental health and well-being. It can lead to mental health complications [mfn] Nishimura, H., Komaki, G., Ando, T., Nakahara, T., Oka, T., Kawai, K., Nagata, T., Nishizono, A., Okamoto, Y., Okabe, K., Koide, M., Yamaguchi, C., Saito, S., Ohkuma, K., Nagata, K., Naruo, T., Takii, M., Kiriike, N., Ishikawa, T., & Japanese Genetic Research Group for Eating Disorders (2008). Psychological and weight-related characteristics of patients with anorexia nervosa-restricting type who later develop bulimia nervosa. BioPsychoSocial medicine, 2, 5. https://doi.org/10.1186/1751-0759-2-5 [/mfn] like:
- Increased risk of developing other mental health disorders such as depression, anxiety disorders, or substance abuse
- Social isolation and withdrawal from relationships and other activities
- Impaired concentration, memory problems, and difficulty with decision-making
- Negative body image, low self-esteem, and poor self-worth
- Perfectionism and obsessive-compulsive tendencies around food, weight, etc.
- Emotional instability, mood swings, and irritability
- Suicidal thoughts or behaviors
Read More About Self-Esteem Here
Impact Of Bulimia Nervosa On Physical Health
Bulimia nervosa can have a drastic impact [mfn] Mond J. M. (2013). Classification of bulimic-type eating disorders: from DSM-IV to DSM-5. Journal of eating disorders, 1, 33. https://doi.org/10.1186/2050-2974-1-33 [/mfn] on an individual’s physical health [mfn] Sato, Y., & Fukudo, S. (2015). Gastrointestinal symptoms and disorders in patients with eating disorders. Clinical Journal of Gastroenterology, 8(5), 255–263. https://doi.org/10.1007/s12328-015-0611-x [/mfn] , linked to:
- Electrolyte imbalances (like imbalances in potassium, sodium, and magnesium)
- Esophageal inflammation, irritation, or rupture due to repeated vomiting
- Dental problems, including tooth decay and gum disease
- Gastrointestinal issues (such as acid reflux, bloating, constipation, or gastric rupture)
- Dehydration and fluid imbalances
- Malnutrition and vitamin deficiencies
- Hormonal imbalances
- Weakened immune system
- Kidney problems (including kidney stones or kidney failure)
Diagnosis Of Bulimia Nervosa
The criteria [mfn] Marilov, V. V., & Sologub, M. B. (2006). Zhurnal nevrologii i psikhiatrii imeni S.S. Korsakova, 106(6), 20–25. [/mfn] for bulimia nervosa diagnosis have been outlined in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5). The process typically includes an initial assessment of the individual’s medical history and medical symptoms, diagnostic criteria evaluation, laboratory tests (like blood tests), and psychological assessment [mfn] Bryant, E., Miskovic-Wheatley, J., Touyz, S. W., Crosby, R. D., Koreshe, E., & Maguire, S. (2021). Identification of high risk and early stage eating disorders: first validation of a digital screening tool. Journal of eating disorders, 9(1), 109. https://doi.org/10.1186/s40337-021-00464-y [/mfn] with clinical tools like:
- Eating Disorder Examination (EDE)
- Structured Clinical Interview for DSM-5 (SCID)
- Eating Disorder Inventory (EDI)
Treatment For Bulimia Nervosa
Bulimia nervosa treatment typically involves a comprehensive approach [mfn] Hay, P. J., & Bacaltchuk, J. (2001). Extracts from “Clinical evidence”: Bulimia nervosa. BMJ (Clinical research ed.), 323(7303), 33–37. https://doi.org/10.1136/bmj.323.7303.33 [/mfn] that addresses both the physical and psychological aspects of the disorder. The common treatment methods include:
1. Psychotherapies
Psychotherapies play a crucial role in bulimia nervosa treatment, offering individuals a safe and supportive environment to address the underlying psychological factors contributing to the disorder.
These therapies empower individuals to develop healthy coping strategies, challenge distorted beliefs, and cultivate self-compassion as they work towards lasting recovery. Common psychotherapies [mfn] Vaidyanathan, S., Kuppili, P. P., & Menon, V. (2019). Eating Disorders: An Overview of Indian Research. Indian journal of psychological medicine, 41(4), 311–317. https://doi.org/10.4103/IJPSYM.IJPSYM_461_18 [/mfn] used in the treatment of bulimia nervosa include:
- Cognitive-behavioral therapy (CBT)
- Enhanced cognitive-behavioral therapy (CBT-E)
- Dialectical behavior therapy (DBT)
- Interpersonal psychotherapy (IPT)
- Psychodynamic therapy
Read More About Cognitive Behavioral Therapy (CBT) Here
2. Family-based treatment (FBT)
Particularly for adolescents, FBT involves the active involvement of the family in the treatment process. It focuses on restoring healthy eating patterns, improving communication, and addressing family dynamics that may contribute to the eating disorder.
3. Nutritional counseling
Working with a registered dietitian who specializes in eating disorders can help individuals develop a balanced and flexible approach to eating, normalize eating patterns, and establish a healthy relationship with food.
4. Pharmacotherapy
Pharmacotherapy [mfn] Gorla, K., & Mathews, M. (2005). Pharmacological treatment of eating disorders. Psychiatry (Edgmont (Pa. : Township[/mfn], 2(6), 43–48. [/mfn] in bulimia nervosa treatment is central to the medical monitoring and management of physical complications associated with bulimia nervosa, such as electrolyte imbalances, gastrointestinal issues, and nutrient deficiencies.
Moreover, medications like selective serotonin reuptake inhibitors (SSRIs) [such as fluoxetine] may be prescribed to help manage associated mood disorders like depression or anxiety.
5. Group therapy
Participating in group therapy or support groups with individuals who have similar experiences can provide a sense of community, support, and understanding.
Read More About Group Therapy Here
6. Residential or inpatient treatment programs
For individuals with severe symptoms or those who have not responded to outpatient treatment, a higher level of care such as residential treatment or inpatient hospitalization may be necessary. These programs offer intensive, round-the-clock support and a structured environment.
How To Cope With Bulimia Nervosa
Coping with bulimia nervosa can be challenging, but there are strategies [mfn] Chakraborty, K., & Basu, D. (2010). Management of anorexia and bulimia nervosa: An evidence-based review. Indian journal of psychiatry, 52(2), 174–186. https://doi.org/10.4103/0019-5545.64596 [/mfn] that can help individuals navigate their respective bulimia nervosa treatment and recovery journeys:
- Seek professional help and reach out to healthcare professionals, therapists, or counselors who specialize in eating disorders.
- Build a support network and surround yourself with supportive individuals who can provide encouragement and empathy.
- Prioritize self-care that promotes physical and emotional well-being, such as engaging in hobbies, practicing relaxation techniques, etc.
- Challenge negative thoughts about body image, food, and self-worth. Replace them with positive and realistic affirmations.
- Recognize triggers and develop healthy self-help strategies for coping during emergencies.
- Establish a structured eating routine to promote a healthier relationship with food. Aim for regular meals and snacks, as well as avoid the consumption of alcohol, tobacco, etc.
- Educate yourself about the facts and myths surrounding bulimia nervosa to gain a better understanding of your condition and foster self-compassion.
- Set realistic goals, celebrate each milestone reached, and acknowledge progress along the way.
- Practice self-acceptance. Embrace and accept yourself as you are, recognizing that your worth is not determined by your appearance or the number on the scale.
- Engage in pleasurable activities that bring you happiness and fulfillment (such as hiking, spending time with loved ones, etc.)
Takeaway
Bulimia nervosa is a complex eating disorder that necessitates immediate medical treatment and empathetic consideration of individual circumstances. While improvement is possible with appropriate treatment and medication, it’s important to recognize that the recovery process can be intricate, and relapses may occur.
Understanding the underlying causes is crucial for developing an effective treatment plan, and open and honest communication with healthcare professionals is essential. Seeking professional help is a courageous step towards healing and can lead to long-term recovery, where individuals regain control of their lives and experience improved well-being.
At A Glance
- Bulimia nervosa is a complex eating disorder characterized by recurrent episodes of excessive food consumption followed by compensatory behaviors to prevent weight gain.
- The disorder involves a cycle of secretive binge eating and subsequent attempts to purge the consumed food.
- Prevalence rates show that it is more commonly diagnosed in females than males.
- Bulimia nervosa can be classified into subtypes—including purging type, non-purging type, low-frequency type, and high-frequency type.
- The causes of bulimia nervosa are multifactorial, including genetic, psychological, sociocultural, and neurobiological factors.
- The disorder can negatively impact mental health, leading to an increased risk of other mental health disorders, social isolation, and emotional instability.
- Recovery from bulimia nervosa is possible with appropriate treatment, support, and a commitment to overall well-being.
Frequently Asked Questions (FAQs)
1. What are the 5 signs of bulimia nervosa?
Five signs of bulimia nervosa include frequent weight fluctuations, evidence of binge eating and purging methods, dental problems, preoccupation with body shape and weight, and secretive behavior around food and eating habits.
2. What is bulimia nervosa characterized by?
The characteristics of bulimia nervosa include recurrent episodes of binge eating followed by compensatory behaviors to prevent weight gain (such as self-induced vomiting, excessive exercise, or fasting).
3. What are the 3 effects of bulimia?
The three effects of bulimia include physical health consequences (like electrolyte imbalances and dental problems), mental health complications (such as the increased risk of other mental health disorders and social isolation), and potential long-term damage to overall well-being.