Baby blues refers to a feeling of moodiness, sadness, and anger that new mothers experience after giving birth. It typically lasts for a brief period of time and goes away on its own.
What Are Baby Blues?
Baby blues refers to a common, temporary psychological state, predominated by feelings of sadness, which occurs right after childbirth. It is also known as postpartum blues (PPB).
Baby blues after pregnancy are considered normal and last for around 2 weeks during the postpartum period. Sometimes, they last for a few hours. The condition is determined by frequent mood swings in a new mother, who may suddenly feel:
- Happy
- Sad
- Angry
- Urge to cry for no reason
- Impatient
- Irritated
- Anxious
- Restless, etc.
Baby blues typically arise within a few days of giving birth. If a woman happens to experience a tough delivery, she may experience the symptoms even sooner.
According to recent research [mfn] Balaram, K., & Marwaha, R. (2022). Postpartum Blues. In StatPearls. StatPearls Publishing. Available from: https://www.ncbi.nlm.nih.gov/books/NBK554546/ [/mfn], postpartum blues are characterized by “low mood and mild depressive symptoms that are transient and self-limited and are extremely common in the perinatal period.”
The postpartum period is a crucial time for new mothers as it [mfn] Beck C. T. (2003). Postpartum depression predictors inventory–revised. Advances in neonatal care : official journal of the National Association of Neonatal Nurses, 3(1), 47–48. https://doi.org/10.1053/adnc.2003.50014 [/mfn] is associated with severe physical and emotional changes, resulting in anxiety and mood disturbances and disorders. There are three levels of postpartum mood dysfunctions:
- Baby blues
- Postpartum depression (PPD)
- Postpartum psychosis
However, baby blues stand on the least severe of the three and does not require any medical treatment, often going away on its own. Joining a group of new mothers or talking with other mothers helps in soothing the symptoms.
However, if the feelings of sadness or anxiousness persist for more than 2 weeks, one must consult their health care provider. In such cases, the new mother may be diagnosed with postpartum depression.
Read More About Postpartum Depression Here
Prevalence Of Baby Blues
According to a 2011 study [mfn] Manjunath, N. G., Venkatesh, G., & Rajanna (2011). Postpartum Blue is Common in Socially and Economically Insecure Mothers. Indian journal of community medicine : official publication of Indian Association of Preventive & Social Medicine, 36(3), 231–233. https://doi.org/10.4103/0970-0218.86527 [/mfn], around 58.5% of women worldwide tend to suffer from baby blues after birth. Research further reveals that 20% of women [mfn] Patel, V., Rodrigues, M., & DeSouza, N. (2002). Gender, poverty, and postnatal depression: a study of mothers in Goa, India. The American journal of psychiatry, 159(1), 43–47. https://doi.org/10.1176/appi.ajp.159.1.43 [/mfn] with baby blues may develop PPD, which can also adversely affect their child’s cognitive development and life experiences.
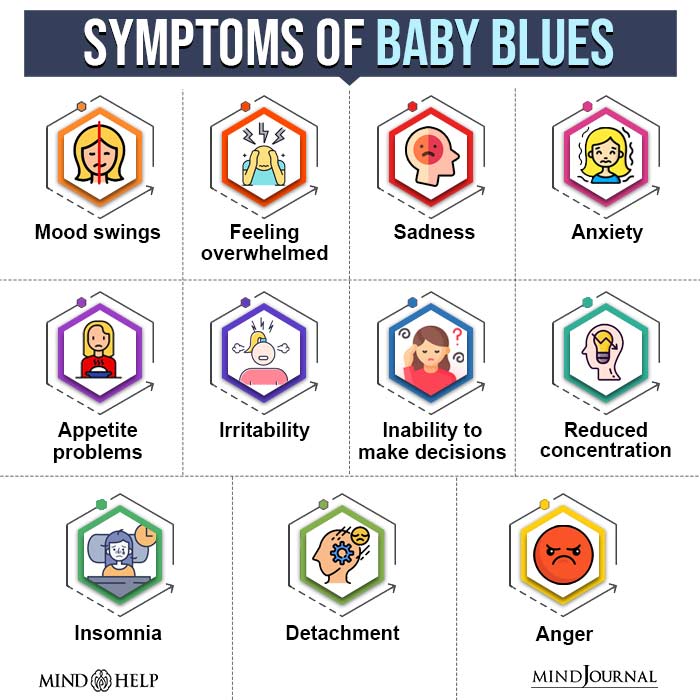
Symptoms Of Baby Blues
As mentioned previously, the symptoms of baby blues are less severe than that of postpartum depression. Here are the most common baby blues symptoms:
- Mood swings
- Feeling overwhelmed
- Sadness
- Anxiety
- Anger
- Appetite problems
- Irritability
- Inability to make decisions
- Uncontrollable crying over a small issue
- Reduced concentration
- Trouble sleeping or insomnia
- Feeling unattached from the child
- Overly worried about the child’s health
Read More About Anger Here
Baby Blues Vs Postpartum Depression (PPD)
Both baby blues and postpartum depression involve mental health problems after childbirth. Although both conditions may have certain similarities, such as mood dysfunctions and anxiety, these are not the same.
In fact, the differences between baby blues and postpartum depression lie in the severity of the condition and its immediate medical care.
In PPD, the mother may not be able to properly care for her child or herself. This is not necessarily the case for baby blues. PPD almost always requires medical treatment.
Read More About Postpartum Depression Here
Causes Of Baby Blues
The causes of baby blues are still being researched. According to a 2005 study, [mfn] M’Baïlara, K., Swendsen, J., Glatigny-Dallay, E., Dallay, D., Roux, D., Sutter, A. L., Demotes-Mainard, J., & Henry, C. (2005). Le baby blues : caractérisation clinique et influence de variables psycho-sociales. L’Encéphale, 31(3), 331–336. https://doi.org/10.1016/s0013-7006(05)82398-x [/mfn] they begin as a result of physiological processes and later manifest psychologically. Research has confirmed certain factors that may contribute to the development of this syndrome, including:
1. Hormonal changes after pregnancy
After birth, a woman’s body goes through extreme hormonal fluctuations to help her recover and care for her baby. These hormonal changes [mfn] Schiller, C., Meltzer-Brody, S., & Rubinow, D. (2015). The role of reproductive hormones in postpartum depression. CNS Spectrums, 20(1), 48-59. doi:10.1017/S1092852914000480 [/mfn] affect a mother’s state of mind in the postpartum period. In most cases, chemical changes in the “mom brain” are triggered, thus leading to brain fog and depression. Moreover, major lifestyle changes and inadequate sleep or nutrition can also result in the condition.
2. Gender bias about infants
A 2011 study [mfn] Institute of Medicine (US) Committee on Assessing Interactions Among Social, Behavioral, and Genetic Factors in Health; Hernandez LM, Blazer DG, editors. Genes, Behavior, and the Social Environment: Moving Beyond the Nature/Nurture Debate. Washington (DC): National Academies Press (US); 2006. 2, The Impact of Social and Cultural Environment on Health. Available from: https://www.ncbi.nlm.nih.gov/books/NBK19924/ [/mfn] observed that there is a strong link between demographic and socio-cultural variables and baby blues. Among them, the gender bias of infants is a deeply rooted cultural aspect in economically backward communities.
The study reveals that as high as 69% of mothers with baby blues[mfn] Manjunath, N. G., Venkatesh, G., & Rajanna (2011). Postpartum Blue is Common in Socially and Economically Insecure Mothers. Indian journal of community medicine : official publication of Indian Association of Preventive & Social Medicine, 36(3), 231–233. https://doi.org/10.4103/0970-0218.86527 [/mfn] are the ones who had given birth to a female child. This trend is seen mostly in countries like India, Pakistan, Bangladesh, etc.
3. Family’s financial conditions
A notable link was found between family income and baby blues. Nearly 62% [mfn] Manjunath, N. G., Venkatesh, G., & Rajanna (2011). Postpartum Blue is Common in Socially and Economically Insecure Mothers. Indian journal of community medicine : official publication of Indian Association of Preventive & Social Medicine, 36(3), 231–233. https://doi.org/10.4103/0970-0218.86527 [/mfn] of mothers suffering from baby blues belong to financially disadvantaged backgrounds. To them, the entry of a new family member into an already economically struggling family creates enormous stress, personal dissatisfaction, and circumstances for domestic violence [mfn] Bhandari, S., Bullock, L. F., Anderson, K. M., Danis, F. S., & Sharps, P. W. (2011). Pregnancy and intimate partner violence: how do rural, low-income women cope?. Health care for women international, 32(9), 833–854. https://doi.org/10.1080/07399332.2011.585532 [/mfn].
4. Dysfunctional families
Baby blues and the mental health of new mothers go hand-in-hand. 71% of new mothers [mfn] Peng, S., Lai, X., Qiu, J., Du, Y., Yang, J., Bai, Y., Jia, Y., Meng, L., Wang, K., & Zhang, X. (2021). Living With Parents-In-Law Increased the Risk of Postpartum Depression in Chinese Women. Frontiers in psychiatry, 12, 736306. https://doi.org/10.3389/fpsyt.2021.736306 [/mfn] staying with their in-laws or in joint families experience postpartum stress and depressive symptoms.
Also, an unhealthy marital relationship is a prominent risk factor for PPB, causing 91% of cases [mfn] Manjunath, N. G., Venkatesh, G., & Rajanna (2011). Postpartum Blue is Common in Socially and Economically Insecure Mothers. Indian journal of community medicine : official publication of Indian Association of Preventive & Social Medicine, 36(3), 231–233. https://doi.org/10.4103/0970-0218.86527 [/mfn]. Lack of emotional and physical support from the family members is also a vital risk factor in baby blues.
5. Other factors
According to studies [mfn] Bloch, M., Rotenberg, N., Koren, D., & Klein, E. (2005). Risk factors associated with the development of postpartum mood disorders. Journal of affective disorders, 88(1), 9–18. https://doi.org/10.1016/j.jad.2005.04.007 [/mfn], other factors may also contribute to the development of the condition, including:
- Unfulfilled parenthood expectations
- Unplanned pregnancy
- Racial or ethnic background
- Mood fluctuations linked with pregnancy
- History of mood changes associated with the menstrual cycle
- History of dysthymia or major depression
- Family history of postpartum depression
- Higher volume of lifetime pregnancies
- History of premenstrual depression
- Degree of depressive symptoms [mfn] O’Hara, M. W., & Wisner, K. L. (2014). Perinatal mental illness: definition, description and aetiology. Best practice & research. Clinical obstetrics & gynaecology, 28(1), 3–12. https://doi.org/10.1016/j.bpobgyn.2013.09.002 [/mfn] while pregnant
It should be noted that baby blues are not necessarily caused by the following factors [mfn] Howard, L. M., Molyneaux, E., Dennis, C. L., Rochat, T., Stein, A., & Milgrom, J. (2014). Non-psychotic mental disorders in the perinatal period. Lancet (London, England), 384(9956), 1775–1788. https://doi.org/10.1016/S0140-6736(14)61276-9 [/mfn]:
- Spontaneous pregnancy or IVF
- Type of delivery (cesarean or vaginal)
- Family history of mood disorders
- Gravidity status (primiparous or multiparous)
Diagnosis Of Baby Blues
Baby blues are not clinically recognized as a separate diagnosis. However, it is identified as “depressive disorder not otherwise specified” or “adjustment disorder with depressed mood”.
There is also no specifically prescribed “baby blues treatment”. However, baby blues can develop into more severe postpartum depression or postpartum psychosis.
Still, thanks to popular clinical practice, it can be diagnosed early [mfn] Rai, S., Pathak, A., & Sharma, I. (2015). Postpartum psychiatric disorders: Early diagnosis and management. Indian journal of psychiatry, 57(Suppl 2), S216–S221. https://doi.org/10.4103/0019-5545.161481 [/mfn] at its very onset. For the proper diagnosis of baby blues, it is required that its symptoms should not meet the diagnostic criteria of postpartum depression or major depressive disorder.
One of the most crucial diagnostic criteria of PPB is that the symptoms should develop within 2-3 days after childbirth and must go away within the next 2 weeks. Women diagnosed with postpartum blues may also be screened carefully [mfn] Balaram K, Marwaha R. Postpartum Blues. [Updated 2022 Mar 9]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK554546/ [/mfn] to check whether they meet the diagnostic criteria for PPD, anxiety disorders, and/or self-harm or suicide.
But if the depressive symptoms continue even after 2 weeks, it may meet the criteria for postpartum depression. In such cases, it is crucial to consult a healthcare professional and seek medical treatment. In extreme cases, the symptoms of psychosis may also be present—indicating the onset of postpartum psychosis.
Self-Help Tips For Baby Blues
Baby blues are temporary and naturally resolved in 1-2 weeks, it is a less severe condition that usually subsides without any professional treatment.
Reassurance, education, validation, and psychosocial support can also help in the recovery process [mfn] Seyfried, L. S., & Marcus, S. M. (2003). Postpartum mood disorders. International review of psychiatry (Abingdon, England), 15(3), 231–242. https://doi.org/10.1080/0954026031000136857 [/mfn]. Regardless, a regular self-care routine can help you fight this condition successfully.
Some helpful self-care ways to overcome baby blues include:

1. Rest
As a new mother, you must take a rest or get enough sleep when the baby is sleeping. During this time, try not to entertain visitors and also keep your phone away.
2. Body care
Take good care of your body, by eating healthy, doing gentle exercises, and drinking plenty of fluids.
3. Spend time outdoor
You should also spend some time outdoors with your baby. Indulge in strategies like taking walks with the baby, engaging in baby-mother play, etc. This can not only strengthen your motherly bond but will also keep you mentally fresh.
4. Seeking help
Sharing your concerns with your family and trusted friends can also help you deal with them better. Try expressing yourself honestly and seek help with household chores and errands and taking care of the baby whenever required.
5. Availing support groups
For both new mothers and fathers, it is a wise decision to join a support group and talk to other new parents. This will help you understand and process your parental experiences better. Mingling in such groups also means receiving advice, suggestions, and tips about parenting your newborn.
How To Help Mothers Manage Baby Blues
If your partner is experiencing baby blues, consider the following helpful and effective tips:
1. Ask her to share her feelings
Make sure to actively listen to her with patience, without judging or offering solutions. Rather than trying to fix things, simply be her shoulder to lean on.
2. Offer help with household activities
Try to take up housework and childcare responsibilities, even before she asks for the same.
3. Make sure she spends time with herself
Help her to take rest and give her the scope to relax. Urge her to take breaks, hire a doula or a babysitter, or schedule some date nights. Restrict visitors to your house and try to take on parenting at both your and your partner’s own pace.
4. Be patient if she’s not up for physical intimacy
Depression changes sex drive and it may take a while for the new mother to get ready for physical intimacy. Give her physical comfort, and understand if she is not ready for sex yet.
5. Enjoy walks with her
Regular light workout sessions can create a big dent in depression. However, with baby blues, it is hard to get motivated for the same. Help her by making walks a daily ritual for both of you. Indulge in other similar tiny interactive rituals that make both of you feel happy and relaxed.
Takeaway
Welcoming a child and entering into motherhood is a whole new experience in a woman’s life. As much as you may look forward to these moments in life, having a baby is stressful.
With the changes in lifestyle, sleep deprivation, new responsibilities, and lack of time for themselves, new mothers are bound to feel overwhelmed. Baby blues are common among many new parents transitioning into a newer, more responsible life.
Many women feel confused about their emotions and often do not talk about them. However, talking about these emotions, changes, and difficulties is one of the best ways to cope with the condition. Fortunately, baby blues go away on their own after some time.
At A Glance
- Baby blues are feelings of moodiness, sadness, and anger that new mothers experience after giving birth.
- It is the least severe of postpartum mood disorders.
- The condition typically lasts for 1 to 2 weeks after delivery.
- Baby blues symptoms include mood swings, anger, sadness, impatience, anxiety, and restlessness.
- Baby blues are self-restricted and transient.
- It can be easily addressed with self-help coping strategies and, in severe cases, therapy and medication.
Frequently Asked Questions (FAQs)
1. How long do baby blues last?
Baby blues last up to 2 weeks and usually go away on their own. If they persist beyond the 2-week period, consider seeking medical help.
2. What to say to a mother experiencing baby blues?
If you know someone going through baby blues, be supportive. Make the moment about her and not her baby. Try not to give advice or solve her problems. Check on her and ask if she wants to avail medical help. If she does, offer to go to doctor’s appointments with her or recommend someone who can help her.
3. Do you get baby blues after your second baby?
Yes, if you had gotten baby blues after your first pregnancy, chances are you can get baby blues again after your second baby.