Postpartum depression (PPD) is a form of depression that affects women after childbirth. Symptoms include anxiety, sadness, and episodes of crying. However, with the right treatment, it can be overcome effectively.
What Is Postpartum Depression?
Also known as postnatal depression, PPD is a type of mood disorder that mainly occurs in women after they give birth to a child. Although it is mostly observed in women, this type of depression can affect both men and women.
As per the Diagnostic and Statistical Manual of Mental Disorders (DSM-5 1 American Psychiatric Association. (2013). DSM-5. Psychiatry.org; American Psychiatric Association. https://www.psychiatry.org/psychiatrists/practice/dsm ), it is a type of depression that may occur within 4 to 6 weeks after childbirth. However, it may also take several months or even up to 1 year after delivery to appear. Diagnosis of this disorder is not only based on the time of onset, but also on the intensity of the depression.
People affected by this condition experience intense sadness, anxiety, low energy, sleeping problems, despair, and irritability which may affect their ability to take care of the infant and perform daily tasks. However, it should be remembered that postpartum depression is very different from “baby blues” that most women experience.
Also Read How Abortion Affects Mental Health
Baby blues vs. Postpartum depression
According to the National Institute of Mental Health (NIMH 2 National Institute of Mental Health. (2021). Perinatal Depression. Available from: https://www.nimh.nih.gov/health/publications/perinatal-depression ), since babies require constant care, it’s normal for mothers to feel tired or overwhelmed sometimes, which is known as “baby blues”.
However, if mood changes and feelings of anxiety or unhappiness are severe, or if they last longer than 2 weeks, a woman may have postpartum depression. Women with postpartum depression generally will not get better unless they receive treatment.
Read More About Baby Blues Here
Symptoms Of Postpartum Depression
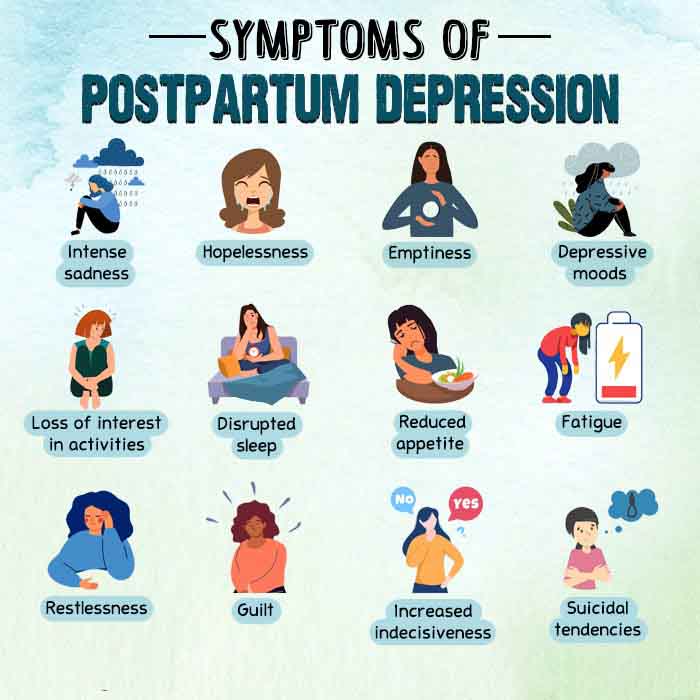
Postpartum depression can feel different for each individual. However, there are some common symptoms that can occur within the first few weeks after delivery. Here are some of the most common physical and emotional indicators of PPD (DSM-5 3 American Psychiatric Association. (2013). DSM-5. Psychiatry.org; American Psychiatric Association. https://www.psychiatry.org/psychiatrists/practice/dsm ):
A. Physical symptoms:
- Severe anxiety & panic attacks
- Loss of energy, fatigue or exhaustion
- Restlessness
- Frequent crying
- Loss of appetite or overeating
- Insomnia or sleeping too much
- Unexplained aches or pains
- Weight changes
- Headaches
- Digestive problems without any clear cause
B. Emotional & psychological symptoms:
- Intense feelings of sadness and misery
- Severe mood swings
- Feelings of hopelessness & helplessness
- Feeling detached or disconnected from the baby
- Social withdrawal
- Intense irritability and anger
- Feelings of guilt, shame & worthlessness
- Lack of interest in hobbies and enjoyable activities
- Doubts about not being a good mother
- Trouble concentrating, remembering, & making decisions
- Feelings of loss of control
- Intense need to escape
- Disinterest in the child
- Fear of being alone with the child
- Intrusive thoughts of harming self or child
- Suicidal thoughts
Case Example
Shabnam is a 25-year-old housewife who has been married for two years. Before marriage, Shabnam was quite hopeful about traveling the world with her husband and moving to a new house. Her sudden unplanned pregnancy within 3 months of marriage came as quite a shock to her.
Due to cultural beliefs, she had to keep the baby against her will. Her family tried their best to make it easier on her. However, Shabnam still found it quite difficult to come to terms with this new direction her life had taken and was feeling very sad and anxious about the future.
These feelings intensified after the birth of her child. Shabnam was not prepared for the huge responsibility in front of her. She started experiencing feelings of hopelessness and lost motivation to do day-to-day activities.
Her mother, sister, and husband were taking care of the baby, while she tried to do the bare minimum. She felt a sense of shame, wondering why she could not feel the same way for her child as mothers generally do.
Even a year later, Shabnam hasn’t been able to accept her new reality. She does not feed her child, give her a bath, or dress her up, letting her family take up these responsibilities.
She often gets irritated if the child comes to talk to her or play with her. Shabnam has also lost interest in things she used to like doing before, such as baking and drawing. She feels tired most of the time and experiences frequent anger outbursts and crying spells.
Shabnam finally decided to consult her gynecologist about her symptoms. After listening to her, the doctor assured her that it was common to feel this way, and referred her to a psychiatrist for treatment of postpartum depression.
Causes/Risk Factors
The exact cause for the development of PPD is not clearly known. However, it is believed that a combination of different factors lead to the development of this mood disorder. Some of the most prominent risk factors for postpartum depression include the following:
1. Physical factors
Childbirth can lead to dramatic hormonal changes 4 Schiller, C. E., Meltzer-Brody, S., & Rubinow, D. R. (2015). The role of reproductive hormones in postpartum depression. CNS spectrums, 20(1), 48–59. https://doi.org/10.1017/S1092852914000480 in the body. Changes in hormones like progesterone and estrogen can often result in PPD. During pregnancy, levels of these hormones can become higher than usual. However, within 24 hours after delivery, levels of estrogen and progesterone may drop down to their usual levels.
Such an abrupt change in hormone levels can cause depression. Moreover, various hormones generated by the thyroid gland can also change substantially that may leave a new mother feeling depressed, fatigued, and lethargic.
Here are some other physical factors that can contribute to the development of PPD:
- Lack of nutritious diet
- Sleep deprivation
- Other mental health or conditions
- Alcohol or substance abuse
2. Genetic factors
Women with a history of a mood or anxiety disorder in the family have a higher risk of developing depression after delivery. Research 5 Corwin, E. J., Kohen, R., Jarrett, M., & Stafford, B. (2010). The heritability of postpartum depression. Biological research for nursing, 12(1), 73–83. https://doi.org/10.1177/1099800410362112 ) indicates that “genetic polymorphisms can be linked theoretically to an increased risk of PPD”, however, no specific gene has been identified yet.
So if one or more family members have experienced PPD, then women from that family may also be affected by it. Moreover, women who have suffered from depression or anxiety previously, especially before or during pregnancy, are at a greater risk of developing this condition.
Read More About Generalized Anxiety Disorder Here
3. Emotional factors
Some of the emotional factors that can lead to PPD have been discussed below:
- If the pregnancy is unplanned or unwanted, then the woman is more likely to suffer from depression.
- Parents who have properly planned the pregnancy may also have difficulty with adjusting to childbirth and having a new baby.
- Parents, who are affected by some medical condition or illness and are unable to care for their child, may feel intense sadness, guilt, shame, and anger. Such negative emotions can greatly affect a new mother’s ability to cope with stress and their self-esteem.
- Some new mothers may doubt their ability to care for their baby, have difficulty with self-identity, may feel unattractive, or feel a lack of control over their lives.
- Some mothers can also have a negative attitude toward the child or have difficulty accepting the child’s gender.
- Mothers who have experienced sexual abuse during childhood may also feel depressed after childbirth.
4. Lifestyle factors
Dramatic lifestyle changes that occur after the birth of a baby can also be a significant contributing factor to this condition. Caring for a child can profoundly change the existing lifestyle of new parents causing PPD in both mothers and fathers.
While caring for the infant, parents are typically unable to get enough sleep, rest, or time to care for their own health and well-being. This can lead to:
- sleep deprivation
- changes in appetite
- exhaustion and
- limited physical activities.
5. Social factors
A lack of support from family members, friends, and others may cause postpartum depression as well. Moreover, certain stressful experiences and life events like a family illness, loss of a loved one, domestic violence, physical, emotional or sexual abuse, or moving to a new location may also act as causative factors.
Apart from these, there may be some other risk factors for postpartum depression, such as:
- Difficulty getting pregnant
- Complicated pregnancy or childbirth
- Excessive worry about child
- Giving birth to twins, triplets, or multiple births
- A child with health issues or special needs
- Trouble breast-feeding
- Teenaged, young or older motherhood
- Relationship problems or marital conflict
- Financial problems or poverty
- Smoking or drinking during pregnancy
- Loneliness or single parenthood
- Previously diagnosed with bipolar disorder
Read More About Bipolar Disorder Here
Effects of PPD
This condition can adversely affect the mother-child bond and affect the mother’s ability to care for the infant. Moreover, this can also cause family issues and marital conflict. You should know about the following effects of postpartum depression.
1. Development of chronic depression
Postpartum depression can persist for several months or even longer if left untreated. Without professional help and care, PPD can lead to a chronic depressive disorder. However, it can also lead to higher risks of major depression in the future, even when it is treated.
Read More About Major Depressive Disorder Here
2. Effect on the father
New fathers may experience emotional distress and strain due to a ripple effect of depression in mothers. PPD in mothers can greatly increase the risk of depression in fathers. Moreover, PPD can also affect fathers, irrespective of the condition in the mother.
3. Complications for children
When postpartum depression is left untreated in mothers, then the child has a higher risk of experiencing behavioral problems and emotional issues. These may include:
- excessive crying
- sleeping problems
- eating disorders
- shorter height 6 Surkan, P. J., Ettinger, A. K., Hock, R. S., Ahmed, S., Strobino, D. M., & Minkovitz, C. S. (2014). Early maternal depressive symptoms and child growth trajectories: a longitudinal analysis of a nationally representative US birth cohort. BMC pediatrics, 14, 185. https://doi.org/10.1186/1471-2431-14-185
- difficulties in language development
- higher risk of obesity 7 Benton, P. M., Skouteris, H., & Hayden, M. (2015). Does maternal psychopathology increase the risk of pre-schooler obesity? A systematic review. Appetite, 87, 259–282. https://doi.org/10.1016/j.appet.2014.12.227 in preschoolers
- difficulties coping with stress and adjusting socially 8 Korhonen, M., Luoma, I., Salmelin, R., & Tamminen, T. (2014). Maternal depressive symptoms: associations with adolescents’ internalizing and externalizing problems and social competence. Nordic journal of psychiatry, 68(5), 323–332. https://doi.org/10.3109/08039488.2013.838804 , especially in school during adolescence, etc.
Read More About Eating Disorders Here
Diagnosis Of Postpartum Depression
Most new mothers are at risk of developing postpartum depression, and other mood disorders. If you think you, your partner or a loved one is suffering from PPD then it is important to consult an obstetrician–gynecologist (ob-gyn) or a mental health professional immediately. Typically, you should not delay visiting a doctor till the postpartum checkup.
The Diagnostic and Statistical Manual of Mental Disorders (DSM-5 9 American Psychiatric Association. (2013). DSM-5. Psychiatry.org; American Psychiatric Association. Available from: https://www.psychiatry.org/psychiatrists/practice/dsm ) identifies this condition as “depressive disorder with peripartum onset.” According to the American Psychiatric Association 10 Torres, F. (2016). What Is Postpartum Depression? Psychiatry.org. Available from: https://www.psychiatry.org/patients-families/postpartum-depression/what-is-postpartum-depression , peripartum depression is “depression occurring during pregnancy or after childbirth”. The use of the term peripartum recognizes that depression associated with having a baby often begins during pregnancy.
As no distinction is made between depression experienced during pregnancy or after delivery, PPD is diagnosed as depression occurring anytime during the first year after childbirth.
The criteria for diagnosing postpartum depression are similar to that of major depression or any other non-childbirth-related depression. However, at least 5 symptoms from the following should be present within 2 weeks of onset:
- Feelings of intense sadness, hopelessness, or emptiness almost every day, most of the time or depressive mood identified by others
- Loss of interest or lack of pleasure in activities
- Changes in sleep patterns
- Reduced appetite or weight loss
- Loss of energy
- Restlessness
- Feelings of guilt or worthlessness
- Increased indecisiveness or loss of concentration
- Suicidal thoughts and tendencies
PPD can only be diagnosed by a healthcare professional, such as a psychiatrist or a psychologist.
- The psychologist may conduct a depression-screening questionnaire such as Beck’s Depression Inventory (BDI) or Hamilton Depression Rating Scale (HAM-D) to rule out other medical illnesses as a cause for the condition.
- They may also recommend some examinations or diagnostic tests, like blood tests to find out if hormonal issues are causing the symptoms.
Prevalence Of PPD
Globally, hundreds of millions of women are affected by PPD annually. According to the American Psychological Association (APA 11 American Psychological Association. (2008). Postpartum depression. Available from: https://www.apa.org/pi/women/resources/reports/postpartum-depression ), about 1 in 7 women are affected by PPD. A recent 2020 scientific review 12 Mughal, S., Azhar, Y., & Siddiqui, W. (2022). Postpartum Depression. In StatPearls. StatPearls Publishing. Available from: https://www.ncbi.nlm.nih.gov/books/NBK519070/ states “PPD occurs in about 6.5% to 20% of women”, mostly in adolescents, mothers who deliver premature infants, and urban women.
For almost 50% of women diagnosed with this disorder, PPD is their first experience with depression. In Asian countries, at least 65% of new mothers experience depression, according to a 2011 study 13 Abdollahi, F., Lye, M. S., Md Zain, A., Shariff Ghazali, S., & Zarghami, M. (2011). Postnatal depression and its associated factors in women from different cultures. Iranian journal of psychiatry and behavioral sciences, 5(2), 5–11. .
Moreover, about 10% of new fathers 14 Paulson, J. F., & Bazemore, S. D. (2010). Prenatal and postpartum depression in fathers and its association with maternal depression: a meta-analysis. JAMA, 303(19), 1961–1969. https://doi.org/10.1001/jama.2010.605 are also affected by postpartum or prenatal depression, according to a 2010 study. It can not only affect first-time mothers and fathers, it can also affect parents who have not experienced PPD when their other children were born.
Treatment Of Postpartum Depression
If you have been diagnosed with PPD, then you must immediately seek treatment from a doctor or mental health professional. The treatment and recovery largely depend on the severity of the condition and the personal needs of the patient.
Therapy and medication are the primary modes of treatment available for postpartum depression. Although the doctor may recommend either, utilizing both together can be more effective.
Read In Details About Treatment Of Postpartum Depression Here
Coping Tips
Apart from seeking medical treatment, it is also important that you make some healthy changes in your lifestyle and daily routine. Here are a few tips that can help you to cope with PPD, when used together with medical treatment and guidance from your doctor:
- Build a strong and secure emotional bond with your child as it will affect your relationship and communication with your baby throughout life.
- Maintain physical contact with your baby as skin-to-skin contact will help to make you both relaxed and strengthen your bond.
- Massage your baby frequently as studies 15 O’Higgins, M., St James Roberts, I., & Glover, V. (2008). Postnatal depression and mother and infant outcomes after infant massage. Journal of affective disorders, 109(1-2), 189–192. https://doi.org/10.1016/j.jad.2007.10.027 have found that infant massage improves the bonding process and reduces the intensity of postpartum depression symptoms in mothers.
- Eat omega-3 fatty acids found in oily fish like salmon and herring, especially during pregnancy, as it may reduce the risk of PPD.
- Get enough sleep as women with this condition tend to sleep less and take longer to fall asleep.
- Spend some time outdoors as exposure to sunlight and even fresh air helps to improve mood.
- Practice self-care and focus on your own needs and wants by asking a loved one to look after the baby for a while.
- Introduce exercise into your schedule as studies 16 Poyatos-León, R., García-Hermoso, A., Sanabria-Martínez, G., Álvarez-Bueno, C., Cavero-Redondo, I., & Martínez-Vizcaíno, V. (2017). Effects of exercise-based interventions on postpartum depression: A meta-analysis of randomized controlled trials. Birth (Berkeley, Calif.), 44(3), 200–208. https://doi.org/10.1111/birt.12294 have found that physical activity helps to overcome PPD.
- Build a support network and try to have positive interactions with your friends and family as emotional support can help to reduce stress.
- It is also important to avoid social isolation.
If your partner or a loved one is suffering from postpartum depression then you must encourage them to seek professional help and follow the medical treatment plan as instructed by the doctor.
Takeaway
Postpartum depression is a treatable condition. Anyone can be affected by depression. However, as new mothers experience a lot of mental, emotional, and physical changes during childbirth, they are more prone to getting depressed during and after pregnancy.
However, it can be effectively treated with timely identification, proper diagnosis, and effective treatment under the supervision of a healthcare professional.
So if PPD is affecting your ability to care for your child and yourself, consult a doctor immediately. With treatment, self-care and support from your partner, family, and friends, you can love and care for your baby the best way.
At A Glance
- Postpartum depression (PPD) is a form of depression that affects women after childbirth.
- Women affected by this condition experience intense sadness, anxiety, low energy, sleeping problems, despair, and irritability which may affect their ability to take care of the infant and perform daily tasks.
- It is a type of major depression that may occur within 4 to 6 weeks after childbirth.
- PPD occurs in about 6.5% to 20% of women.
- Although most new mothers struggle with PPD or postnatal depression, new fathers may also be affected by it.
- This condition can adversely affect the mother-child bond and affect the mother’s ability to care for the infant.
- Therapy and medication are the primary modes of treatment available for postpartum depression.
Frequently Asked Questions (FAQs)
1. Do fathers have postpartum depression?
Yes. Men can also experience sadness, fatigue, anxiety, changes in appetite and sleeping patterns, and feel overwhelmed after childbirth. According to a 2010 study 17 Davé, S., Petersen, I., Sherr, L., & Nazareth, I. (2010). Incidence of maternal and paternal depression in primary care: a cohort study using a primary care database. Archives of pediatrics & adolescent medicine, 164(11), 1038–1044. https://doi.org/10.1001/archpediatrics.2010.184 , around 4% of new fathers suffer from PPD in the first year after their baby’s birth.
2. Does postpartum depression happen after miscarriage?
Almost 20% women who experience a miscarriage show symptoms of anxiety and depression, that can last for 1 or 2 years. 18 Nynas, J., Narang, P., Kolikonda, M. K., & Lippmann, S. (2015). Depression and Anxiety Following Early Pregnancy Loss: Recommendations for Primary Care Providers. The primary care companion for CNS disorders, 17(1), 10.4088/PCC.14r01721. https://doi.org/10.4088/PCC.14r01721 However, ‘postpartum depression’ only occurs during pregnancy and the postnatal period.
3. Can postpartum depression last for years?
Yes. About 5% of women continue to experience symptoms of postpartum depression for 3 years after the birth of the child. 19 Postpartum depression may last for years | National Institutes of Health (NIH). (2020). National Institutes of Health (NIH); www.nih.gov. Retrieved from https://www.nih.gov/news-events/nih-research-matters/postpartum-depression-may-last-years
4. Is peripartum depression the same as postpartum depression?
Yes, the terms are often used interchangeably.