Major depressive disorder (MDD) is a mood disorder characterized by feelings of sadness, loss of interest, and worthlessness. Also known as clinical depression, it can significantly affect our health and our lives, if left untreated.
What Is Major Depressive Disorder?
Major depressive disorder (MDD) is a psychological condition (( Brigitta, B. (2022). Pathophysiology of depression and mechanisms of treatment. Pathophysiology of Depression, 4(1), 7–20. https://doi.org/10.31887/dcns.2002.4.1/bbondy )) that not only affects our thinking, mood, and behavior, but also our physical wellbeing. Other than a constant feeling of sadness, those affected may experience:
- Low energy
- Low self-esteem
- Aches and pains without any probable reason
- Loss of interest in activities they used to enjoy earlier
MDD can also affect their ability to study, work, eat, sleep, and socialize. In severe cases, it can lead to self-harm and suicide. Unfortunately, due to mental health stigmatization, most people suffering from MDD do not seek professional help or treatment.
Read More About Self-Esteem Here
Major Depressive Disorder In Films
Multiple films (( DAS, S., Doval, N., Mohammed, S., Dua, N., & Chatterjee, S. S. (2017). Psychiatry and Cinema: What Can We Learn from the Magical Screen?. Shanghai archives of psychiatry, 29(5), 310–313. https://doi.org/10.11919/j.issn.1002-0829.217014 )) have portrayed characters with clinical depression, their struggles, and the impact on their lives and relationships. David O. Russell’s Silver Linings Playbook (2012) tells the story of Pat Solitano (Bradley Cooper), who is diagnosed with bipolar disorder and major depressive disorder. Prozac Nation (2001) stars Christina Ricci as Elizabeth, who deals with depression and is prescribed Prozac for treatment.
Most notably, The Hours (2002) interweaves the stories of three women facing major depressive disorder across three generations, based on Michael Cunningham’s novel. It has notable performances by Meryl Streep, Nicole Kidman, and Julianne Moore.
Prevalence Of Major Depressive Disorder
According to the World Health Organization (WHO), more than 264 million people worldwide suffer from major depressive disorder (MDD) (( Reddy, M. (2010). Depression: The disorder and the burden. Indian Journal of Psychological Medicine, 32(1), 1. https://doi.org/10.4103/0253-7176.70510 )) , with a higher prevalence among women. The average lifetime prevalence of clinical depression is about 12% (( Bains, N., & Abdijadid, S. (2022). Major Depressive Disorder. PubMed; StatPearls Publishing. Available from: https://www.ncbi.nlm.nih.gov/books/NBK559078/ )) , with developed countries experiencing higher rates at around 15% (( Wang, J., Wu, X., Lai, W., Long, E., Zhang, X., Li, W., Zhu, Y., Chen, C., Zhong, X., Liu, Z., Wang, D., & Lin, H. (2017). Prevalence of depression and depressive symptoms among outpatients: a systematic review and meta-analysis. BMJ Open, 7(8), e017173. https://doi.org/10.1136/bmjopen-2017-017173 )) , compared to 11% in developing nations.
Short-term prevalence of MDD symptoms is approximately 7%, varying by age. MDD is more common among those lacking close relationships or who are divorced, separated, or widowed, but socioeconomic status and racial/ethnic groups show no significant differences (( Wang, J., Wu, X., Lai, W., Long, E., Zhang, X., Li, W., Zhu, Y., Chen, C., Zhong, X., Liu, Z., Wang, D., & Lin, H. (2017). Prevalence of depression and depressive symptoms among outpatients: a systematic review and meta-analysis. BMJ Open, 7(8), e017173. https://doi.org/10.1136/bmjopen-2017-017173 )) .
Major Depressive Disorder Symptoms
A person suffering from major depressive disorder will experience multiple depressive episodes consisting mainly of the following signs and symptoms based on the DSM-5 :
1. Psychological Symptoms
The common psychological major depressive disorder symptoms include:
- Persistent sadness
- Low mood
- Excessive overthinking
- Stress, anxiety, and frustration
- Feelings of hopelessness and worthlessness
- Irritability and agitation
- Feelings of guilt
- Pessimism and helplessness
- Loss of interest in pleasurable activities
- Difficulty in concentrating and making decisions
- Memory problems or difficulty in remembering details
- Angry outbursts over small issues
- Poor performance at work or school
- Drug and alcohol abuse
- Suicidal thoughts and tendencies
Read More About Stress Here
2. Physical Symptoms
The common physical major depressive disorder symptoms include:
- Reduced energy, constant exhaustion, or fatigue
- Lethargy
- Feelings of restlessness
- Slowed thinking, talking, or body movements
- Difficulty in sleeping, or excessive sleeping
- Changes in appetite
- Weight loss or gain
- Digestive problems
- Headache disorders
- Body aches or pains due to unknown reasons
- Injuries due to self-harm
Causes Of Major Depressive Disorder
The common (( Chand, S. P., & Arif, H. (2023). Depression. PubMed; StatPearls Publishing. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430847/#:~:text=Clinical%20and%20preclinical%20trials%20suggest )) causes of major depressive disorder in children and adults include:
- Genetic predisposition and family history
- Brain chemistry imbalances (involving serotonin and other neurotransmitters)
- Life stressors (such as trauma, loss, or significant life changes)
- Chronic medical conditions or chronic pain
- Substance abuse or alcoholism
- Hormonal changes (like those occurring during pregnancy, menopause, or thyroid problems)
- Certain medications with depressive side effects
- Co-occurring mental health disorders (like anxiety or bipolar disorder)
- Personal and environmental factors (such as social isolation and low socioeconomic status)
Read More About Chronic Pain Here
Mental Health Effects Of MDD
People suffering from the symptoms of MDD are affected in a variety of ways (( Christensen, M. C., Wong, C. M. J., & Baune, B. T. (2020). Symptoms of Major Depressive Disorder and Their Impact on Psychosocial Functioning in the Different Phases of the Disease: Do the Perspectives of Patients and Healthcare Providers Differ?. Frontiers in psychiatry, 11, 280. https://doi.org/10.3389/fpsyt.2020.00280 )) , including:
- Having low mood
- Experiencing anxiety
- Suffering from insomnia
- Experiencing psychotic symptoms (such as hallucinations and delusions)
- Worrying excessively about their physical health.
- Having difficulty functioning effectively at school or work
- Having difficulty forming/maintaining healthy relationships
- Having frequent conflicts in interpersonal relationships
- Being vulnerable to substance abuse and addiction
- Having low sexual drive among other things
Read More About Insomnia Here
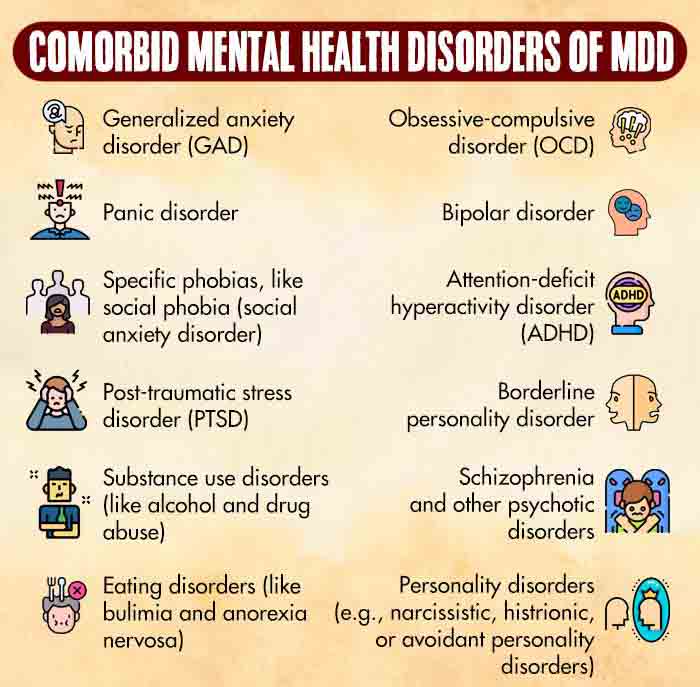
Major depressive disorder symptoms are also believed to affect and alter (( Zhang, F.-F., Peng, W., Sweeney, J. A., Jia, Z.-Y., & Gong, Q.-Y. (2018). Brain structure alterations in depression: Psychoradiological evidence. CNS Neuroscience & Therapeutics, 24(11), 994–1003. https://doi.org/10.1111/cns.12835 )) regions of the human brain which help regulate moods. In people with clinical depression, nerve cells in specific areas of the brain function ineffectively, which affects communication between nerve circuits. Therefore, sufferers are prone to developing a bevy of co-morbid mental health disorders.
Major Depressive Disorder In Children
Major depressive disorder in children can severely impact their mental health (( Pataki, C., & Carlson, G. A. (2016). Major Depressive Disorder Among Children and Adolescents. Focus (American Psychiatric Publishing), 14(1), 10–14. https://doi.org/10.1176/appi.focus.20150037 )) , leading to persistent feelings of sadness, hopelessness, and low self-esteem. It can hinder their ability to engage in daily activities, concentrate at school and in academics, and form healthy social relationships. Left untreated, clinical depression may contribute to a negative self-image and, in severe cases, even suicidal thoughts or self-harming behaviors in children.
Diagnosis For Major Depressive Disorder
Diagnosing major depressive disorder in children and adults typically involves a mental health professional examining the patient’s symptom history, emotional state, and considering personal, social, and family backgrounds.
There are no specific major depressive disorder screening test, but psychologists often use psychometric tests (( Smith, K. M., Renshaw, P. F., & Bilello, J. (2013). The diagnosis of depression: current and emerging methods. Comprehensive psychiatry, 54(1), 1–6. https://doi.org/10.1016/j.comppsych.2012.06.006 )) like the Hamilton Rating Scale for Depression (HAM-D) and Beck’s Depression Inventory (BDI) to evaluate depression. The patient’s physical health is also examined to rule out other medical conditions that might contribute to the symptoms, such as thyroid problems.
Treatment For Major Depressive Disorder
The treatment for major depressive disorder in children and adults involves a combination of psychotherapies and medication (( Karrouri, R., Hammani, Z., Benjelloun, R., & Otheman, Y. (2021). Major depressive disorder: Validated treatments and future challenges. World journal of clinical cases, 9(31), 9350–9367. https://doi.org/10.12998/wjcc.v9.i31.9350 )) :
1. Psychotherapies
Several psychotherapies are prescribed in the treatment for major depressive disorder, including:
- Cognitive-behavioral therapy (CBT)
- Interpersonal psychotherapy (IPT)
- Problem-solving therapy
- Psycho-dynamic therapy
- Group therapy
Through psychotherapy, patients can learn to identify and challenge negative thought patterns, develop healthier coping strategies for major depressive disorder symptoms, and improve their interpersonal relationships. It can be used as a standalone treatment for milder symptoms of MDD or in combination with medication for more severe major depressive disorder.
Read More About Cognitive Behavioral Therapy (CBT) Here
2. Medication
A mental health professional may recommend various types of antidepressants tailored to the individual and the severity in the symptoms of MDD, including:
- Atypical antidepressants
- Monoamine oxidase inhibitors (MAOIs)
- Selective serotonin reuptake inhibitors (SSRIs)
- Selective serotonin and norepinephrine reuptake inhibitors (SNRIs)
- Tricyclic antidepressants
These medications (( Seifert, J., Maier, H. B., Führmann, F., Bleich, S., Stübner, S., Sieberer, M., Bernegger, X., Greil, W., Schüle, C., Toto, S., Grohmann, R., & Reinhard, M. A. (2022). Pharmacological treatment of major depressive disorder according to severity in psychiatric inpatients: results from the AMSP pharmacovigilance program from 2001-2017. Journal of neural transmission (Vienna, Austria : 1996), 129(7), 925–944. https://doi.org/10.1007/s00702-022-02504-6 )) can be highly effective in treating moderate to severe major depressive disorder by targeting specific neurotransmitters that influence the brain’s regulation of stress and mood.
Coping With Major Depressive Disorder
Mild or severe major depressive disorder can be a debilitating mental health disorder and, therefore, medical help is central to its recovery. However, you can avail the following self-help tips (( van Grieken, R. A., Kirkenier, A. C., Koeter, M. W., & Schene, A. H. (2014). Helpful self-management strategies to cope with enduring depression from the patients’ point of view: a concept map study. BMC psychiatry, 14, 331. https://doi.org/10.1186/s12888-014-0331-7 )) to manage mild symptoms of MDD in-between therapy sessions:
- Establish a routine: Create a structured daily schedule to provide a sense of stability and purpose.
- Set realistic goals: Break tasks into smaller, manageable steps, and celebrate achievements.
- Physical health: Prioritize regular exercise, a balanced diet, and adequate sleep.
- Avoid substance abuse: Stay away from alcohol and drugs, as they can worsen depressive symptoms.
- Reach out to loved ones: Share your feelings with trusted friends and family members, and lean on their support.
- Challenge negative thoughts: Work with a therapist to identify and change negative thought patterns.
- Relaxation techniques: Practice stress-reduction techniques like deep breathing, meditation, or yoga.
- Engage in enjoyable activities: Participate in hobbies and interests that bring joy and satisfaction.
- Self-compassion: Be kind to yourself, and recognize that recovery takes time and effort.
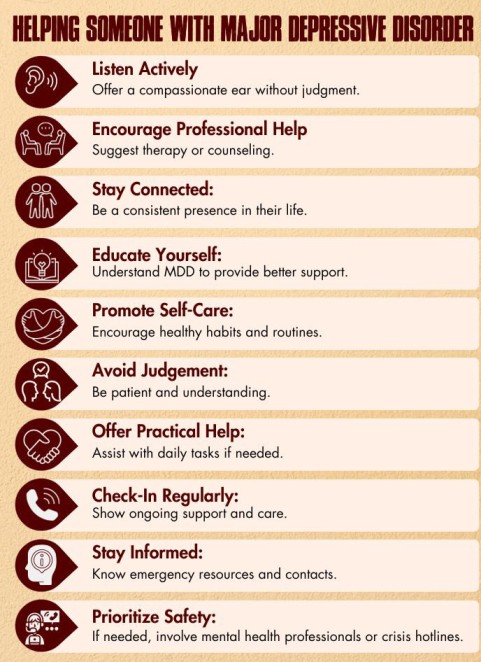
Helping Someone With Major Depressive Disorder
Supporting someone with symptoms of MDD requires patience, empathy, and understanding. Offer a listening ear without judgment, encourage them to seek professional help, and engage in activities together that they enjoy. Ensure they stick to their treatment plan, and be there for them even on tough days. Your unwavering support (( Li, Z., Ruan, M., Chen, J., & Fang, Y. (2021). Major Depressive Disorder: Advances in Neuroscience Research and Translational Applications. Neuroscience bulletin, 37(6), 863–880. https://doi.org/10.1007/s12264-021-00638-3 )) can make a significant difference in their journey towards recovery.
Takeaway
Mild or severe major depressive disorder is a significant mental illness that responds well to early diagnosis and treatment. If you or someone you know is struggling with the symptoms of MDD, it’s crucial to consult a primary care physician or mental health specialist and adhere to the treatment plan to enhance the patient’s outlook on life and facilitate their full recovery for a happier, healthier life.
At A Glance
- Major depressive disorder (MDD) is a serious mood disorder characterized by persistent sadness and low energy.
- Films like “Silver Linings Playbook,” “Prozac Nation,” and “The Hours” have depicted characters with MDD and its impact.
- Worldwide, more than 264 million people have MDD.
- The symptoms of MDD encompass psychological and physiological aspects.
- The causes of major depressive disorder include genetic factors, brain chemistry imbalances, life stressors, etc.
- MDD can have various mental health effects and affect brain function, potentially leading to co-morbid mental disorders.
- Treatment for major depressive disorder involves a combination of therapies, medication, and self-help techniques.
Frequently Asked Questions (FAQs)
1. Is Major Depressive Disorder A Disability?
Major depressive disorder can be considered a disability if it significantly impairs an individual’s ability to carry out daily activities.
2. What Goals Should I Set For My Major Depressive Disorder?
Goals for major depressive disorder may include improving daily functioning, managing symptoms, and enhancing overall well-being.
3. What Could Be Some Biological Reasons For Developing Depression After Traumatic Events?
Biological causes of major depressive disorder after traumatic events involve changes in brain chemistry, genetics, and the body’s stress response system.
4. What Is The Difference Between Major Depressive Disorder And Persistent Depressive Disorder?
The key difference between major depressive disorder and persistent depressive disorder is the duration of symptoms; MDD involves discrete episodes, while PDD features a chronic, long-lasting pattern.
5. Can Schizoaffective Disorder And Major Depressive Disorder Coexist At The Same Time In The Same Person?
Yes, schizoaffective disorder and major depressive disorder can coexist in the same person, as they are distinct but sometimes comorbid conditions.