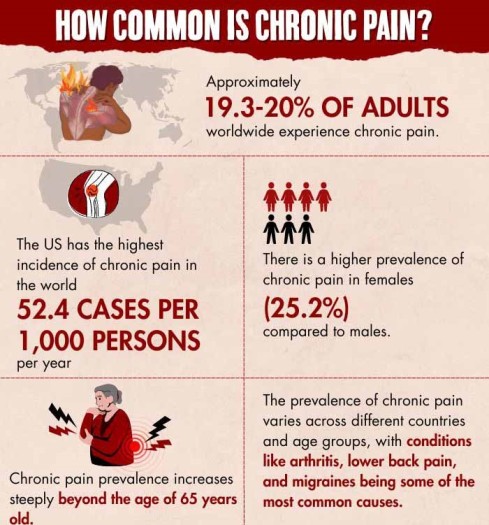
Chronic pain is a persistent and often debilitating condition that affects millions of individuals worldwide. It transcends physical discomfort to turn into mental pain that impacts various aspects of their lives.
What Is Chronic Pain?
Chronic pain refers to persistent discomfort 1 Dydyk, A. M., & Conermann, T. (2020). Chronic pain. PubMed; StatPearls Publishing. Available from: https://www.ncbi.nlm.nih.gov/books/NBK553030/ that lasts for an extended period, typically beyond the expected timeframe for healing or recovery. Unlike acute pain, which is a natural response to injury and generally subsides as the body heals, chronic pain persists for weeks, months, or even years.
Chronic pain symptoms encompasses a diverse range of conditions, including arthritis, fibromyalgia, migraines, and lower back pain, to name a few. This enduring discomfort often manifests as a persistent or recurring sensation characterized by aching, burning, stabbing, or throbbing.
Unlike the fleeting nature of acute pain, chronic pain weaves its way into emotional and mental well-being, leading to stress, anxiety, depression, and an overall diminished quality of life. Chronic pain can also be extremely debilitating for our ability to form and maintain social relationships. What makes chronic pain especially challenging is its potential to create a self-perpetuating cycle, where physical suffering exacerbates emotional distress, and heightened stress and anxiety can intensify the perception of pain.
Chronic Pain In Films
Chronic pain in films is often utilized to elicit empathy and illuminate the struggles faced by individuals enduring this condition. Commercially and critically acclaimed films like The Elephant Man (1980), The Fault In Our Stars (2014), Cake (2014), and The Theory Of Everything (2014) all feature protagonists who experience chronic pain. Similarly, short films like Fibro And The New Me (2018) and End-O (2019) provide insights into the complex psychological effects of chronic pain to raise awareness for the same.
Chronic Pain And Mental Health
Chronic pain and mental health are closely connected. The different types of chronic pain affect the sufferer biologically and psychologically. The relentless chronic pain symptoms can lead to anxiety and depression, affecting daily life and creating a challenging cycle where pain and mental distress reinforce each other.
Furthermore, the psychological effects of chronic pain can extend beyond mood disorders. It can disrupt sleep patterns, impair cognitive function, and even strain relationships, leading to feelings of isolation and decreased social support. Conversely, individuals with pre-existing mental health conditions may be more susceptible to developing or exacerbating 2 Rama Yasaei, & Abdolreza Saadabadi. (2019, May 11). Chronic Pain Syndrome. Nih.gov; StatPearls Publishing. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470523/ chronic pain, highlighting the complex bidirectional relationship between the two.

Mental Health Conditions Associated With Chronic Pain

The psychological effects of chronic pain can be enhanced by mental health conditions 3 Mills, S. E. E., Nicolson, K. P., & Smith, B. H. (2019). Chronic pain: a review of its epidemiology and associated factors in population-based studies. British journal of anaesthesia, 123(2), e273–e283. https://doi.org/10.1016/j.bja.2019.03.023 like:
1. Anxiety disorders:
Conditions like generalized anxiety disorder can increase muscle tension and amplify pain perception, worsening chronic pain.
2. Depression:
Depressive disorders can lower pain tolerance and make it more difficult to cope with the emotional and physical aspects of chronic pain.
Read More About Depression Here
3. Post-traumatic stress disorder (PTSD):
Trauma-related stress can exacerbate chronic pain symptoms and lead to a more complex and challenging pain management process.
Read More About Post-Traumatic Stress Disorder (PTSD) Here
4. Obsessive-compulsive disorder (OCD):
Obsessive thoughts and compulsive behaviors may distract individuals from managing their pain effectively.
Read More About Obsessive-Compulsive Disorder (OCD) Here
5. Bipolar disorder:
Mood swings and fluctuations in energy levels can impact an individual’s ability to manage chronic pain consistently.
Read More About Bipolar Disorder Here
6. Somatization disorder (conversion disorder):
Individuals with this condition may experience physical symptoms that are worsened by psychological distress, complicating the management of chronic pain.
7. Substance use disorders:
Substance abuse can co-occur with chronic pain and exacerbate both the pain and the mental health challenges associated with it.
8. Eating disorders:
The physical toll of eating disorders can amplify the experience of chronic pain and complicate its treatment.
9. Personality disorders:
Conditions like borderline personality disorder may lead to impulsive behaviors that can worsen the management of chronic pain and mental health.
Read More About Personality Disorders Here
10. Somatic symptom disorder:
This disorder involves excessive focus on physical symptoms, which can intensify the perception of chronic pain and make it more challenging to address.
What Causes Chronic Pain?
The common 4 Raffaeli, W., Tenti, M., Corraro, A., Malafoglia, V., Ilari, S., Balzani, E., & Bonci, A. (2021). Chronic Pain: What Does It Mean? A Review on the Use of the Term Chronic Pain in Clinical Practice. Journal of pain research, 14, 827–835. https://doi.org/10.2147/JPR.S303186 causes of chronic pain symptoms:
- Physical injuries or trauma, such as fractures or surgeries
- Underlying medical conditions like arthritis, diabetes, or cancer
- Nerve damage (neuropathic pain)
- Inflammation and tissue damage
- Persistent muscle tension and spasms
- Psychological factors, including stress, anxiety, depression, psychogenic pain syndrome, etc.
How Is Chronic Pain In Mental Health Diagnosed?
Diagnosing chronic pain symptoms within the context of mental health involves a thorough assessment 5 Cohen, S. P., Vase, L., & Hooten, W. M. (2021). Chronic pain: an update on burden, best practices, and new advances. Lancet (London, England), 397(10289), 2082–2097. https://doi.org/10.1016/S0140-6736(21)00393-7 . The mental health treatment for chronic pain includes a medical history, physical examination, and psychological evaluation to gauge its impact on mental well-being. Collaboration between medical and mental health professionals is essential for a comprehensive diagnosis and proper psychological treatment for patients with chronic pain that addresses all aspects of chronic pain in mental health.
Mental Health Treatment For Chronic Pain
An integrated, personalized plan 6 Crofford L. J. (2015). Chronic Pain: Where the Body Meets the Brain. Transactions of the American Clinical and Climatological Association, 126, 167–183. is mandatory in the psychological treatment for patients with chronic pain to improve mental well-being. The commonly available methods in the mental health treatment for chronic pain include:
- Psychotherapy, including cognitive-behavioral therapy (CBT), to address pain-related thoughts and emotions.
- Medications (like antidepressants, anti-convulsants, opioids, etc.) to manage mood disorders, depression or anxiety.
- Relaxation techniques, stress management, and mindfulness practices.
- Support groups and peer counseling for a sense of community and shared understanding.
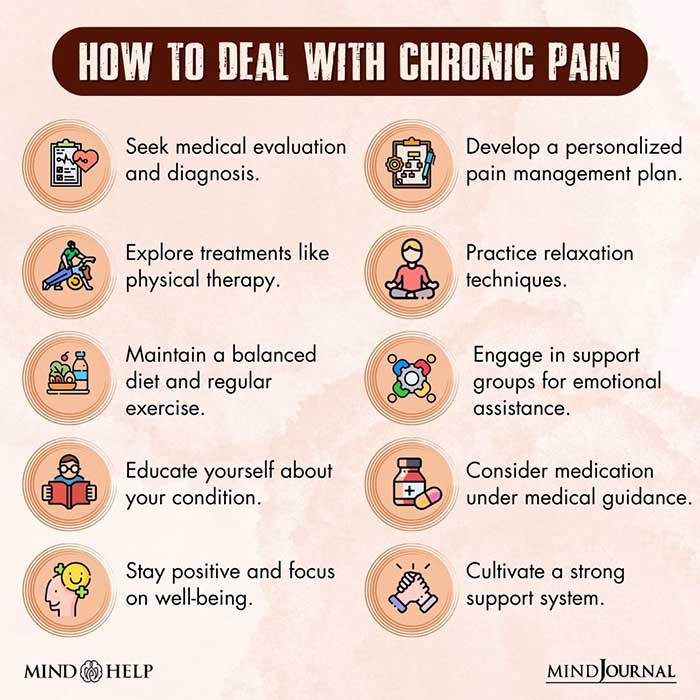
Coping With The Psychological Effects Of Chronic Pain
Consider the following measures 7 Dueñas, M., Ojeda, B., Salazar, A., Mico, J. A., & Failde, I. (2016). A review of chronic pain impact on patients, their social environment and the health care system. Journal of pain research, 9, 457–467. https://doi.org/10.2147/JPR.S105892 for coping with the psychological effects of chronic pain:
- Therapy: Participate in tailored therapy sessions (like nature, art, and music therapies, etc.) to enhance mobility and reduce pain.
- Mind-Body Techniques: Practice relaxation methods like mindfulness and deep breathing.
- Support: Connect with support groups or seek peer counseling for emotional assistance.
- Pain Management: Learn techniques like pacing and goal-setting.
- Education: Stay aware and educated about your condition for informed decision-making.
Read More About Therapy Here
Takeaway
Chronic pain’s connection to mental health is a complex relationship that necessitates a holistic approach for effective management. By recognizing this interplay, healthcare providers can develop more personalized plans for psychological treatment for patients with chronic pain. Increased awareness and understanding of this dynamic relationship can also help reduce stigma and improve the quality of mental health treatment for chronic pain.
At A Glance
- Chronic pain is an enduring and often debilitating condition that goes beyond just physical discomfort.
- The relationship between chronic pain and mental health is complex.
- This prolonged pain can lead to emotional distress, anxiety, and depression.
- The mental health treatment for chronic pain requires collaboration between medical and mental health professionals.
- Plans for the psychological treatment for patients with chronic pain include psychotherapy, medication, relaxation techniques, and support groups.
- Understanding this intricate relationship can lead to more effective management and reduce the stigma around chronic pain and mental health.
Frequently Asked Questions (FAQs)
1. Is psychogenic pain a form of chronic pain?
Yes, psychogenic pain is a form of chronic pain that is primarily attributed to psychological factors.
2. How do you deal with chronic pain mentally?
Dealing with chronic pain mentally often involves techniques like cognitive-behavioral therapy (CBT), mindfulness, and relaxation exercises to manage pain-related stress and emotions.
3. Is mental pain chronic pain?
Mental pain and chronic pain are related but distinct; mental pain typically refers to emotional suffering, while chronic pain pertains to persistent physical discomfort.
4. What are the emotional causes of chronic pain?
Emotional causes of chronic pain can include stress, anxiety, depression, unresolved trauma, and negative emotional states that contribute to the experience and perception of physical pain.