Table of Contents
Shared Psychotic Disorder is a mental condition where one or more healthy people obtain delusions from someone they are close with. It is also popularly known as Folie à deux, which means madness shared by two.
What Is Shared Psychotic Disorder?
Shared psychotic disorder (SPD) is a rare psychiatric syndrome where a delusion is shared by two or more people with strong emotional connections. It is a delusional disorder where one mentally healthy individual can start believing the delusions, and even hallucinations, of someone with a psychotic disorder. It is also known as shared delusional disorder (SDD) or shared psychosis. According to a 2010 study [mfn] Korkmaz, S., Kuloğlu, M., Bahçeci, B., & Atmaca, M. (2010). Shared psychotic disorder: A case report. Dusunen Adam: The Journal of Psychiatry and Neurological Sciences, 206-209. https://doi.org/10.5350/dajpn2010230308t [/mfn] “Shared psychotic disorder (folie à deux) is a rare disorder characterized by delusions and demonstrates intercultural differences.”
This condition is usually observed in people involved in a close personal relationship where the person without any previous mental health issues (termed as the acceptor, associate or secondary) picks up on the delusions of another individual with a psychotic or delusional disorder, like schizophrenia (known as the inducer, principal or primary). It has been observed that SPD occurs almost exclusively in members of the same family, mostly sisters, parent & child or husband & wife.
The Merck Manuals explain [mfn] Tamminga, C. (2020). Shared psychosis – Psychiatric disorders – MSD manual professional edition. MSD Manual Professional Edition. https://www.msdmanuals.com/professional/psychiatric-disorders/schizophrenia-and-related-disorders/shared-psychosis [/mfn] “The patient with the primary disorder is usually the socially dominant member in the relationship and imposes the delusion on or convinces the patient with the secondary disorder of the unusual beliefs.” For proper diagnosis and effective treatment, it is important that the inducer or the person with the primary psychosis is identified as the secondary person usually lets go of the delusional ideas and beliefs when they are separated from the inducer.
Origins Of Folie à Deux
Shared Psychotic Disorder was first reported in 1860 by Baillarger. However, the disorder was conceptualized in 1877 by Charles Lasègue and Jean-Pierre Falret as Folie à Deux. It was also commonly known as Lasègue-Falret syndrome [mfn] Arnone, D., Patel, A., & Tan, G. M. (2006). The nosological significance of Folie à Deux: a review of the literature. Annals of general psychiatry, 5, 11. https://doi.org/10.1186/1744-859X-5-11 [/mfn] .
It refers to a group of disorders where symptoms like paranoid delusions are transferred from one individual to one or more people who are “intimately associated.” During the 19th century, it was known by various other names, like Folie communique or communicated psychosis in France and Induziertes Irresein in German, termed by Lehman and Sharfetter.
The transference and sharing of delusional ideas is known as Folie à deux, when it occurs between 2 people, Folie à trois when three people are involved, Folie à quatre when four people are affected and so on. When the condition involves an entire family it is known as Folie en famille or ‘family madness’ [mfn] Jolfaei, A. G., Isfahani, M. N., & Bidaki, R. (2011). Folie à deux and delusional disorder by proxy in a family. Journal of research in medical sciences : the official journal of Isfahan University of Medical Sciences, 16 Suppl 1(Suppl1), S453–S455. [/mfn] . However, when a group of people or a community is involved in sharing a delusion, like in a cult, it is called Folie à plusieurs or ‘madness of several’. For instance, if a cult leader has a psychotic disorder and is delusional, then it is highly likely that their followers will also believe their delusions, like the Heaven’s Gate mass suicide incidence.
This rare condition was originally listed as ‘shared paranoid disorder’ in DSM-3. But later the psychiatric classifications in DSM-4 referred to this condition as shared psychotic disorder and as induced delusional disorder in ICD-10. However, the condition is listed as “other specified schizophrenia spectrum and other psychotic disorder” in the latest Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5).
It states that all individuals suffering from the condition will be diagnosed with a “delusional disorder”. Hence, there is no differentiation made between the primary case and secondary case(s) for diagnostic purposes. But the differentiation could be crucial for the treatment process.
Understanding Shared Psychotic Disorder
“Shared psychotic disorder, also known as folie a’ deux, psychosis by association and induced psychotic disorder, is an uncommon and unique psychiatric disorder,” states a 2011 scientific review [mfn] Christensen, R. C., & Ramos, E. (2011). The social and treatment consequences of a shared delusional disorder in a homeless family. Innovations in clinical neuroscience, 8(4), 42–44. [/mfn] . Individuals suffering from shared psychotic disorder may lose touch with reality. Moreover, they often tend to have difficulty with functioning in daily life. Delusions and hallucinations are the most common symptoms as sufferers see or hear things that are unreal and believe things which are untrue, even when presented with facts pointing to the contrary.
It usually occurs in people sharing a long-term relationship with one person being dominant and the other individual being passive. People sharing the delusion are often related, either by marriage or blood. As the primary individual influences and imposes their delusional beliefs on the secondary person, their delusions may disappear or diminish when they are no longer in contact with the primary case or if their relationship is affected in some way.
It has also been observed that although sufferers may have strong emotional connections with each other, they tend to lack social ties. Although the exact cause of occurrence is unclear, researchers believe that social isolation and stress may be a significant contributing factor. Research [mfn] José, M. S., & Mary, V. S. (1995). Shared psychotic disorder: A critical review of the literature. The Canadian Journal of Psychiatry, 40(7), 389-395. https://doi.org/10.1177/070674379504000705 [/mfn] indicates that this disorder “occurs in premorbidly disposed individuals in the context of social isolation which is shared with a psychotic person.”
In many cases, particularly in family situations, one parent may act as the primary individual, while the children may acquire their parent’s delusional beliefs to varying degrees. This may make the children believe in certain conspiracy theories like alien abductions or authorities spying on them. Unfortunately, most people suffering from this condition rarely seek any treatment. Their disorder is noticed and diagnosed only when the primary individual seeks or gets treatment or when the secondary partner acts out of their delusion.
Prevalence Of Shared Psychotic Disorder
The prevalence of shared psychotic disorder is unclear but it is considered to be a rare condition. However, some studies [mfn] Al Saif F, Al Khalili Y. Shared Psychotic Disorder. [Updated 2021 Aug 30]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK541211/ [/mfn] reveal that around 1.7-2.6% of psychiatric hospital admissions suffer from SPD. But these statistics could be inaccurate as the condition is under-diagnosed.
Moreover, very few people suffering from this disorder actively seek treatment as they are mostly unaware of their mental illness. This is why many experts believe that Shared Psychotic Disorder may not be a rare condition [mfn] Arnone, D., Patel, A., & Tan, G. M. (2006). The nosological significance of Folie à Deux: a review of the literature. Annals of general psychiatry, 5, 11. https://doi.org/10.1186/1744-859X-5-11 [/mfn] . It has also been observed that more women than men with delusional dominant partners tend to develop this disorder.
According to a 2012 research paper, “Folie à deux is also known as communicated insanity, contagious insanity, infectious insanity, psychosis of association and induced psychosis [mfn] Mentjox, R., van Houten, C. A., & Kooiman, C. G. (1993). Induced psychotic disorder: clinical aspects, theoretical considerations, and some guidelines for treatment. Comprehensive psychiatry, 34(2), 120–126. https://doi.org/10.1016/0010-440x(93)90056-a [/mfn] .” It adds that around 90% of relationships affected by this disorder tend to be nuclear families with sister–sister relationships being the most common dyad. Therapy and medication can successfully help someone recover from the disorder.
Types Of Shared Psychotic Disorder
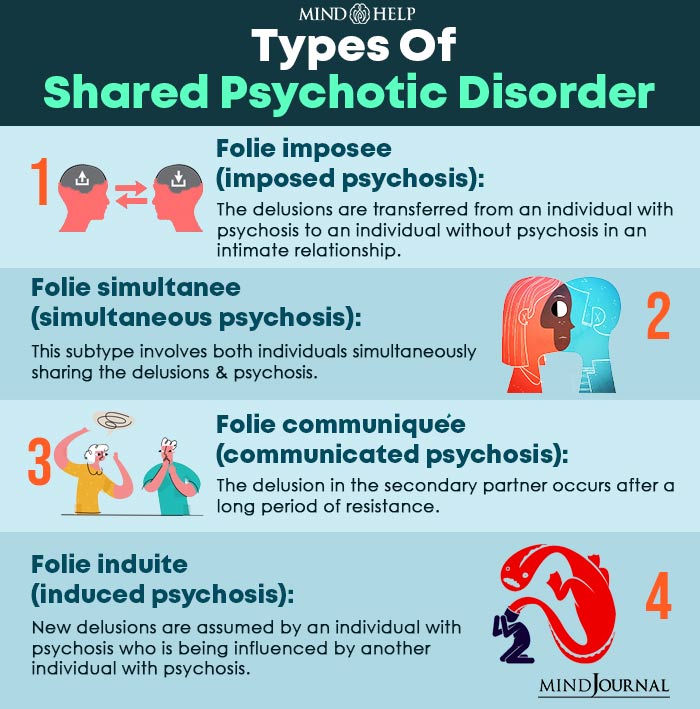
Various subtypes of Shared Psychotic Disorder have been described which include the following:
1. Folie imposee (imposed psychosis)
Conceptualized in 1877 by Lasègue and Falret, this subtype involves the transference of delusions from one person to another in an intimate relationship. The primary individual is dominant while the secondary individual is suggestible and submissive. These are mostly persecutory delusions which reduce or disappear when the two people are separated.
2. Folie simultanee (simultaneous psychosis)
Conceptualized in 1880 by Regis, this subtype involves both individuals simultaneously sharing the delusions and psychosis. Research indicates that there may be a genetic risk factor among family members, especially siblings. Moreover, prolonged social isolation may also be a risk factor as well.
3. Folie communiquée (communicated psychosis)
Originally described in 1881 by Marandon de Montyel, this subtype is almost similar to Folie imposee or imposed psychosis. However, the second individual is usually more resistant to the delusions of the primary individual. But eventually, the second partner tends to give in and acquires the delusional beliefs. Moreover, they may keep believing in their delusions even when separated from the primary case.
4. Folie induite (induced psychosis)
This subtype was described in 1885 by Lehmann. It involves the second individual being induced with new and additional delusions by the primary partner. Research reveals that in this type of Shared Psychotic Disorder, the delusions are often expanded. This is usually observed between two individuals who are both suffering from mental illnesses.
Shared Psychotic Disorder And Delusions
The severity of the condition and the symptoms largely depend on the type of delusion which is shared by two or more people. Delusions [mfn] Kiran, C., & Chaudhury, S. (2009). Understanding delusions. Industrial psychiatry journal, 18(1), 3–18. https://doi.org/10.4103/0972-6748.57851 [/mfn] may be categorized under the following 4 major types:
1. Bizarre delusions
These are mostly implausible beliefs that are physically impossible and are not accepted or understood by most people from the same cultural background. A bizarre delusion may be being abducted by aliens and being operated or experimented on .
2. Non-bizarre delusions
These include delusional ideas which may be possible and are understood by people from the culture, but are highly improbable. For instance, believing that the FBI is tracking your smartphone and watching you all the time. Although this may be possible, it is highly unlikely.
3. Mood-congruent delusions
These delusions correspond to your mood and emotions (manic or depressed) within a given period of time. For instance, if the sufferer is experiencing a manic episode, they believe that they will win the lottery or hit the jackpot in a casino without any reason to believe so. However, in a depressive state the person may believe that they or a family member may die in an accident, again without any probable reason.
4. Mood-neutral delusions
These delusions are not influenced by your mood and can be either bizarre or non-bizarre. These are not directly related to the emotional state of the sufferer. For instance, a person may believe that an imposter or doppelgänger has switched bodies with a friend or a family member. The delusional belief may continue even with adequate changes in their emotional status.
Symptoms Of Shared Psychotic Disorder
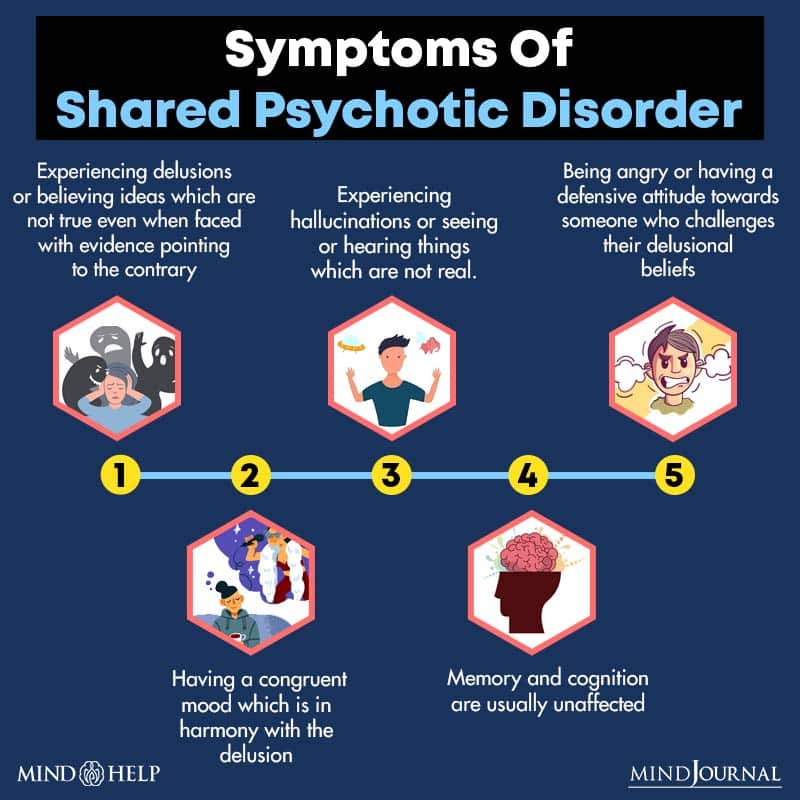
A shared delusion occurs in a person when they are in a close relationship with someone who already has an established delusion. Here are some of the common specific symptoms of SPD:
- Experiencing delusions or believing ideas which are not true even when faced with evidence pointing to the contrary
- Experiencing hallucinations or seeing or hearing things which are not real. Secondary partner may experience hallucinations
- Being angry or having a defensive attitude towards someone who challenges their delusional beliefs
- Relevant and coherent speech
- Having a congruent mood which is in harmony with the delusion
- Having systematically structured thoughts that are goal oriented while sharing delusional ideas
- Less likely to express distorted or abnormal perceptions
- Memory and cognition are usually unaffected
- Mostly unaware of their mental illness
- Homicidal or suicidal thoughts and behavior may be present
Moreover, both the primary individual and the secondary partner may appear normal, groomed and well-dressed. However, if they have a history or aggression or outbursts, then hospitalization may be recommended for safety issues.
Read More About Anger Here
Causes Of Shared Psychotic Disorder

Although the exact causes for the occurrence of shared psychotic disorder are still unclear, there are some risk factors which are associated with this condition. Some of them include:
1. Untreated mental illness in primary partner
Chronic mental disorder can be a serious issue when left untreated. It could lead to some serious social problems like influencing and affecting the lives of other family members. In the case of SPD, it has been observed that the primary case is usually suffering from delusional disorder, schizophrenia or affective disorder.
2. Age
Age of the partners can be a significant risk factor as well. Studies [mfn] Shimizu, M., Kubota, Y., Toichi, M., & Baba, H. (2007). Folie à deux and shared psychotic disorder. Current psychiatry reports, 9(3), 200–205. https://doi.org/10.1007/s11920-007-0019-5 [/mfn] have shown that age differences between primary and secondary partners can make the older person more dominant and the younger person more submissive.
Read More About Aging Here
3. Gender
It has been observed that gender also plays an important part. Shared Psychotic Disorder is more commonly seen in women, not only as the secondary partner but also as the primary case as well.
Read More About Gender Here
4. Type of the relationship
Most of the cases studied by researchers revealed that the disorder usually occurs among family members The most common relationship between primary and secondary partners are “married or common-law couples”, while the second most common dyad are sisters.
5. Duration of a relationship
Research reveals that the length of relationship plays a major role in the development of this disorder. The attachment which the secondary individual shares with the primary case greatly influences their adoption of the delusional beliefs.
6. Social Isolation
Social withdrawal and isolation have been reported in most studied cases of SPD. Poor social interaction can often confuse a person and make them more submissive and suggestible to their primary partner. Due to lack of social comparison, they can become easily influenced under threatening or frightening conditions. To maintain a mutual relationship, the secondary individual may harmoniously receive information from the primary individual and will eventually believe the information to be true.
7. Cognitive impairment
Experts have observed that the secondary partner usually lacks adequate intelligence and good judgment.
8. Personality issues
Personality defects can also be a prominent factor leading to shared psychotic disorder. Usually, the secondary individual tends to be emotionally immature, introverted and neurotic. Case studies have revealed that premorbid personality disorders characteristics, like dependent, schizotypal or schizoid, could also play a major role.
9. Communication problems
Communication issues can lead to problems in sharing ideas and emotions and this may result in social withdrawal and isolation. Experts [mfn] Bankier R. G. (1988). Role reversal in folie à deux. Canadian journal of psychiatry. Revue canadienne de psychiatrie, 33(3), 231–232. https://doi.org/10.1177/070674378803300313 [/mfn] believe that by strengthening communication between dyad relationships can help both individuals accept different perspectives which may subside “in the presence of rigid mindless thinking.” This can be done with multiple-conjoint psychotherapy.
10. Comorbidity of secondary partner
Research [mfn] Silveira, J. M., & Seeman, M. V. (1995). Shared psychotic disorder: a critical review of the literature. Canadian journal of psychiatry. Revue canadienne de psychiatrie, 40(7), 389–395. [/mfn] reveals that if someone has been diagnosed with a serious mental condition, like dementia, bipolar affective disorder, depression, mental retardation or schizophrenia, then they are more likely to be influenced and affected by someone who is also suffering from some form of mental illness.
11. Stressful life events
Adverse and negative life experiences may affect the mindset and behavior of someone and make them accept specific delusions. As the stressful event may influence the relationship between the primary and the secondary person, it can reduce the ability of the secondary partner to resist certain emotions and delusional ideas of the primary case.
Diagnosis Of Shared Psychotic Disorder
This mental condition is not identified in the recent DSM-5 as a separate diagnosis and is listed as “Other specific schizophrenia spectrum and other psychotic disorders.” It is difficult to diagnose shared delusional disorder as the secondary partner usually does not seek professional help.
The individual is mostly unaware that they have distorted beliefs and delusions that are acquired from a dominant person they are emotionally connected with. Moreover, as the delusional beliefs are obtained over time and built gradually, their resistance and doubts is reduced slowly.
A person must meet the following criteria to be diagnosed with shared delusional disorder:
- It must involve a delusion which has been acquired through a close personal relationship between the primary partner and the secondary partner(s). The primary case must have an already established delusion.
- The delusional beliefs of the secondary individual(s) should be identical or at least similar to the already established delusion of the primary case.
- The delusion must not be due to some other mental illness, like a psychological disorder or a mood disorder involving psychological characteristics, or a general medical condition, medications or due to substance abuse.
Like most psychiatric disorders, no particular lab tests are required for diagnosing SPD. However, some brain imaging or laboratory tests, like blood tests, or physical exams may be required to rule out other medical conditions and causes. The doctor, psychiatrist, psychologist or any other mental health professional may ask certain questions to assess the medical and psychiatric history of both the primary and secondary case.
Once it has been established that the symptoms are not caused by other factors, the doctor may conduct a clinical interview and talk to the patient to understand their behavior and attitude. The doctor may also conduct a mental state examination and talk to a third party to gain better understanding.
Complications Of Shared Psychotic Disorder
If left untreated, shared psychotic disorder may become a chronic condition. It can lead to aggressive behavior, depression, anxiety and complete social withdrawal. Moreover, patients can even become suicidal and homicidal as well when they start acting on their delusional thoughts and beliefs. One 2013 study [mfn] Guivarch, J., Piercecchi-Marti, M. D., & Poinso, F. (2018). Folie à deux and homicide: Literature review and study of a complex clinical case. International journal of law and psychiatry, 61, 30–39. https://doi.org/10.1016/j.ijlp.2018.10.001 [/mfn] of SPD cases revealed that “homicides were committed with great violence, usually against a victim in the family circle, and were sometimes followed by suicide.”
It is believed that a combination of persecutory and mystical delusions comprised the major risk factor for homicide. The study added “The homicides occurred in response to destabilization of the delusional dyads.” By acting on their paranoid delusions, patients may unintentionally commit certain assaults and put their own and others’ lives in danger.
Treatment Of Shared Psychotic Disorder
Standard treatment methods are not that well acknowledged as the condition is rare. Moreover, it is often undiagnosed and hence, untreated. Although the primary case may receive treatment, the doctor may be unable to identify or diagnose the secondary partner. However, once the secondary sufferer is identified, various treatment options may be utilized to help the sufferer overcome the symptoms of SPD and reduce the delusions.
According to Unusual psychiatric syndromes [mfn] Bhandari, S. (2012). Unusual psychiatric syndromes. Core Psychiatry, 349-357. https://doi.org/10.1016/b978-0-7020-3397-1.00023-9 [/mfn] published in Core Psychiatry (Third Edition), 2012, “The first step in treatment is separation of the two persons suffering from the delusions because about 40% The majority of those who are impacted secondary react to this treatment. Primary cases require therapy for the underlying disorder, which in most cases is schizophrenia, while secondary cases that do not improve with separation may require antipsychotic medication.” Furthermore, there is the issue of social isolation also needs to be resolved as family therapy and social support can significantly help in overcoming delusions.
The following treatment options are available for overcoming the symptoms of shared psychotic disorder:
1. Therapy
The most beneficial and common types of therapy for the treatment of SPD include
- Psychotherapy
- Family therapy
Let’s take a look at how these therapeutic practices can help someone recover from this condition:
A. Psychotherapy
“Psychotherapy is a successful psychological intervention for a wide range of psychological, behavioural, and somatic issues, symptoms, and disorders, and is thus appropriately regarded as a primary treatment option in mental and somatic disorders” health care management,” explains a recent 2019 study [mfn] Locher, C., Meier, S., & Gaab, J. (2019). Psychotherapy: A World of Meanings. Frontiers in psychology, 10, 460. https://doi.org/10.3389/fpsyg.2019.00460 [/mfn] . Individual psychotherapy involves one-on-one counseling that aims to reduce stress and anxiety and helps the sufferer understand their distorted thinking and behavior patterns. As the therapist encourages the patient to talk more openly by gaining their trust, they can learn about the patient’s mindset and help them better.
Over time, the therapist can help the patient identify the delusions and enable them to think in a healthier manner. Although this can be a challenging process as the sufferer is unaware of their own condition, psychotherapy can help a person with SPD by relieving emotional distress and separating the secondary person from the primary case with mental illness, who has the original delusions.
B. Family therapy
Family therapy [mfn] Varghese, M., Kirpekar, V., & Loganathan, S. (2020). Family Interventions: Basic Principles and Techniques. Indian journal of psychiatry, 62(Suppl 2), S192–S200. https://doi.org/10.4103/psychiatry.IndianJPsychiatry_770_19 [/mfn] or group therapy encourages the secondary person to build healthy social connections and relationships and seek various interests outside the dyad. It involves therapy for the entire family so that each member can work on improving their relationships with each other. Moreover, it can also help to reduce delusional thoughts in the family dynamic. With healthy family support, the patient can get out of the influence of the inducer and recover from SPD. It can also help the patient develop healthy social ties, build new life goals, pursue interests, adhere to medications and live a healthier life.
2. Medications
If separation from the mentally ill primary case, who had the original delusion, proves ineffective, then medication may be prescribed for a brief period of time. Medications may also be recommended to ease extreme symptoms, like anxiety, insomnia and excessive restlessness, depending on the individual. Some common medications prescribed for shared psychotic disorder may include:
- Antipsychotics
- Antidepressants
- Mood stabilizers
- Tranquilizers
- Sedatives
Antipsychotics can help with delusions and hallucinations, which are common symptoms of psychosis. However, they may not cure psychosis. Research [mfn] Arnone, D., Patel, A., & Tan, G. M. (2006). The nosological significance of Folie à Deux: a review of the literature. Annals of general psychiatry, 5, 11. https://doi.org/10.1186/1744-859X-5-11 [/mfn] reveals that treatment using medication for both primary and secondary partners with antipsychotics, antidepressants and mood stabilizers “could improve the condition.”
Read More About Antidepressants Here
Coping With Shared Psychotic Disorder
Although SPD cannot be prevented, effective diagnosis and treatment can help someone recover from this condition. However, apart from professional help, the sufferer can do certain things to overcome the disorder. Here a few things to remember, if you are recovering from SPD:
- Strictly follow your doctor’s instructions and stick to the prescribed treatment process.
- Keep seeing your doctor or therapist until you can form a trusting professional relationship with them. This is crucial for successful treatment even though it may seem difficult initially.
- If you or someone you know is suffering from this condition, then make sure to reach out and seek professional help.
This condition can become chronic and damaging if left untreated. Although it may be initially difficult to distinguish the delusions from the truth, with proper treatment a sufferer can fully recover. In fact, if you are the secondary person, you can overcome the feeling of being dependent on the mentally ill primary partner and encourage them to seek help as well.
Recovery Is Possible
Shared psychotic disorder can be an intense, unsettling and terrifying experience. But it is possible to reduce and even eliminate the symptoms. If you are the primary partner receiving treatment, then you need to inform your doctor about the impact of your condition and help them identify the secondary person(s) so that they can also be treated for the shared delusion. In case, the secondary person is a child or unable to seek help, then family, friends or a third party must intervene and reach out.
Effective and proper treatment can not only help to reduce the symptoms, but it can even help the patient to fully recover from SPD in most cases.
Shared Psychotic Disorder At A Glance
- Shared psychotic disorder (SPD) is a rare psychiatric syndrome where a delusion is shared by two or more people with strong emotional connections.
- Shared psychotic disorder, also known as folie a’ deux, psychosis by association and induced psychotic disorder, is an uncommon and unique psychiatric disorder.
- The severity of the condition and the symptoms largely depend on the type of delusion which is shared by two or more people.
- SPD cannot be prevented, effective diagnosis and treatment can help someone recover from this condition.
- Shared psychotic disorder can be an intense, unsettling and terrifying experience.






Leave a Reply