Sleep disorders are a group of health conditions that disturb normal sleep patterns, and interfere with our everyday functioning. They are quite a common clinical problem.
What Are Sleep Disorders?
Sleep disorders are psychological conditions that interfere with a person’s quality, timing, and amount of sleep resulting in subsequent distress and disturbances in functioning.
The symptoms can last for a few weeks, a certain phase in life, or for several years. If left untreated, sleep disorders can affect our personal and professional lives and social relationships.
Such disorders include problems related to falling asleep and maintaining sleep (such as insomnias), disorders associated with excessive sleeping, and other sleep dysfunctions, related to the sleep stages or parasomnias.
People suffering from acute or chronic sleep disorders experience disrupted sleeping patterns. They experience great difficulty in falling asleep or staying awake and are usually plagued by conditions like –
- Irritability
- Low energy
- Mood swings
- Daytime drowsiness
Sleep conditions [mfn] Karna, B., Sankari, A., & Tatikonda, G. (2022). Sleep Disorder. In StatPearls. StatPearls Publishing. Available Here: https://www.ncbi.nlm.nih.gov/books/NBK560720/ [/mfn] , if left untreated, lead to severe mental and physical health issues, such as:
- Cognitive decline
- Neurodegenerative diseases
- Pain conditions
- Cardiovascular and coronary diseases
- Hormonal imbalances leading to diabetes, etc.
- Hypoxemia and dyspnea
- Gastroesophageal reflux disease
- Brain aging
- Delayed puberty
- Early-onset of menses and menopause
- Memory disorders like dementia, Alzheimer’s disease (AD), etc.
- Psychiatric disorders like depression, anxiety, stress disorders, etc.
Sleep disorders, in some form or the other, affect populations from all age groups across the globe. In some cases, these disorders are short-term and acute—lasting for a few days or weeks.
These disorders can be easily treated with therapy, medication, or self-help strategies. However, if left untreated, they can grow into complex and long-drawn health conditions with fatal comorbid conditions sometimes requiring surgery and hospitalization.
You Can Read More About Nightmare Disorder Here
Symptoms
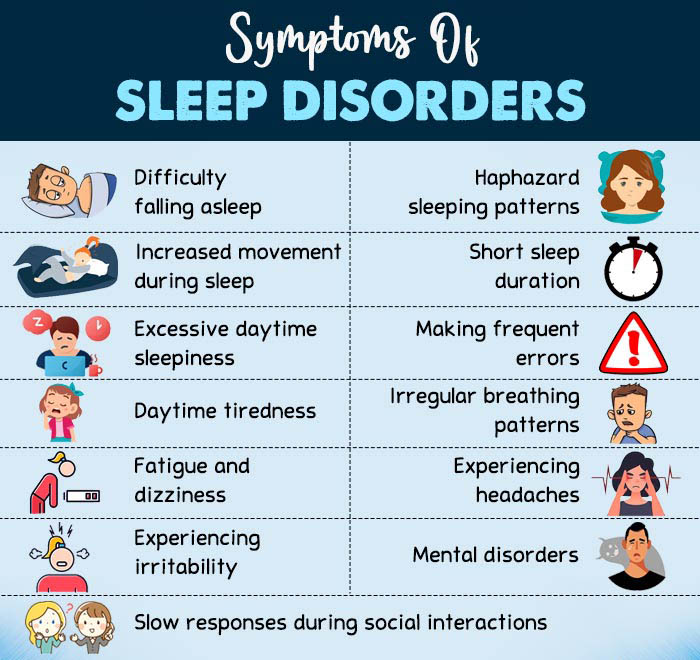
The most common sleep disorders symptoms include:
- Difficulty falling asleep
- Haphazard sleeping patterns
- Increased movement during sleep
- Short sleep duration
- Excessive daytime sleepiness
- Making frequent errors or mistakes
- Daytime tiredness
- Irregular breathing patterns
- Fatigue and dizziness
- Experiencing migraines and headaches
- Experiencing irritability, lack of concentration, attention deficiency, forgetfulness, etc.
- Slow responses during social interactions
- Mental disorders like depression, anxiety, schizoaffective disorders, etc.
Causes
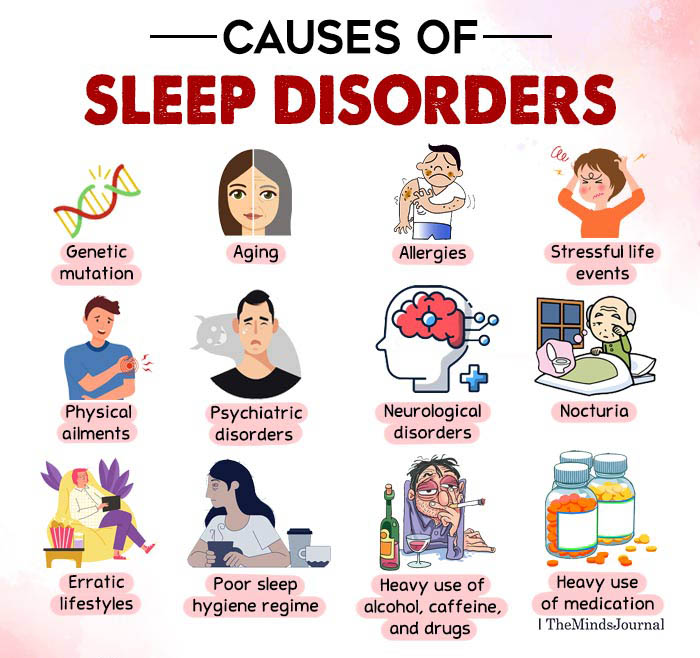
According to research, the causes of sleep disorders in children and adults are as follows:
- Genetic mutation [mfn] Sehgal, A., & Mignot, E. (2011). Genetics of sleep and sleep disorders. Cell, 146(2), 194–207. https://doi.org/10.1016/j.cell.2011.07.004 [/mfn]
- Aging [mfn] Suzuki, K., Miyamoto, M., & Hirata, K. (2017). Sleep disorders in the elderly: Diagnosis and management. Journal of general and family medicine, 18(2), 61–71. https://doi.org/10.1002/jgf2.27 [/mfn]
- Allergies [mfn] Xi, Y., Deng, Y. Q., Chen, S. M., Kong, Y. G., Xu, Y., Li, F., Jiao, W. E., Lu, G., & Tao, Z. Z. (2022). Allergy-related outcomes and sleep-related disorders in adults: a cross-sectional study based on NHANES 2005-2006. Allergy, asthma, and clinical immunology : official journal of the Canadian Society of Allergy and Clinical Immunology, 18(1), 27. https://doi.org/10.1186/s13223-022-00669-z [/mfn] and respiratory problems
- Stressful life events [mfn] Li, Y., Gu, S., Wang, Z., Li, H., Xu, X., Zhu, H., Deng, S., Ma, X., Feng, G., Wang, F., & Huang, J. H. (2019). Relationship Between Stressful Life Events and Sleep Quality: Rumination as a Mediator and Resilience as a Moderator. Frontiers in psychiatry, 10, 348. https://doi.org/10.3389/fpsyt.2019.00348 [/mfn]
- Physical ailments [mfn] Colten, H. R., Altevogt, B. M., & Institute of Medicine (US) Committee on Sleep Medicine and Research (Eds.). (2006). Sleep Disorders and Sleep Deprivation: An Unmet Public Health Problem. National Academies Press (US). Available here: https://pubmed.ncbi.nlm.nih.gov/20669438/ [/mfn] (such as ulcers, asthma, hypothyroidism, hyperthyroidism, etc.)
- Psychiatric disorders [mfn] Anderson, K. N., & Bradley, A. J. (2013). Sleep disturbance in mental health problems and neurodegenerative disease. Nature and science of sleep, 5, 61–75. https://doi.org/10.2147/NSS.S34842 [/mfn] (such as depression, anxiety, schizoaffective disorders, headache disorders, etc.)
- Neurological disorders [mfn] Bishir, M., Bhat, A., Essa, M. M., Ekpo, O., Ihunwo, A. O., Veeraraghavan, V. P., Mohan, S. K., Mahalakshmi, A. M., Ray, B., Tuladhar, S., Chang, S., Chidambaram, S. B., Sakharkar, M. K., Guillemin, G. J., Qoronfleh, M. W., & Ojcius, D. M. (2020). Sleep Deprivation and Neurological Disorders. BioMed research international, 2020, 5764017. https://doi.org/10.1155/2020/5764017 [/mfn] (such as stroke, epilepsy, dementia, etc.)
- Nocturia [mfn] Leslie, S. W., Sajjad, H., & Singh, S. (2022). Nocturia. In StatPearls. StatPearls Publishing. Available here: https://pubmed.ncbi.nlm.nih.gov/30085529/ [/mfn] , or frequent urination
- Erratic lifestyles [mfn] Shochat T. (2012). Impact of lifestyle and technology developments on sleep. Nature and science of sleep, 4, 19–31. https://doi.org/10.2147/NSS.S18891 [/mfn]
- Poor sleep hygiene regime [mfn] Yazdi, Z., Loukzadeh, Z., Moghaddam, P., & Jalilolghadr, S. (2016). Sleep Hygiene Practices and Their Relation to Sleep Quality in Medical Students of Qazvin University of Medical Sciences. Journal of caring sciences, 5(2), 153–160. https://doi.org/10.15171/jcs.2016.016 [/mfn]
- Working schedules [mfn] Jeong, I., Park, J. B., Lee, K. J., Won, J. U., Roh, J., & Yoon, J. H. (2018). Irregular work schedule and sleep disturbance in occupational drivers-A nationwide cross-sectional study. PloS one, 13(11), e0207154. https://doi.org/10.1371/journal.pone.0207154 [/mfn] that mess up the circadian rhythm (like night shifts, break shifts, etc.)
- Heavy use [mfn] Mahfoud, Y., Talih, F., Streem, D., & Budur, K. (2009). Sleep disorders in substance abusers: how common are they?. Psychiatry Edgmont (Pa. : Township), 6(9), 38–42. [/mfn] of alcohol, caffeine, and drugs (like narcotics, etc.)
- Heavy use of medication [mfn] Foral, P., Knezevich, J., Dewan, N., & Malesker, M. (2011). Medication-induced sleep disturbances. The Consultant pharmacist : the journal of the American Society of Consultant Pharmacists, 26(6), 414–425. https://doi.org/10.4140/TCP.n.2011.414 [/mfn]
Types
Sleep disorders list is an integral component of psychiatric manuals which categorize different sleep disorders in a myriad of ways. However, the most commonly used classification of sleep disorders used by researchers and medical practitioners is provided in the International Classification of Sleep Disorders (ICSD [mfn] Thorpy, M.J. Classification of Sleep Disorders. Neurotherapeutics 9, 687–701 (2012). https://doi.org/10.1007/s13311-012-0145-6 [/mfn] ).
As per ICSD classification, types of sleep disorders are as follows:
1. Insomnia
Insomnia disorder is characterized by dissatisfaction with sleep quantity or quality, associated with
- difficulty falling asleep
- frequent nighttime awakenings with difficulty returning to sleep, and/or
- awakening earlier in the morning than desired
There are different types of insomnia such as chronic insomnia disorder, short term insomnia disorder etc.
You Can Read More About Insomnia Here
2. Sleep-related breathing disorders
Sleep-related breathing disorders include various types of apnea and are characterized by a lack of breathing effort and obstruction of the breathing canals. The different types of sleep-related breathing disorders include:
I. Obstructive sleep apnea (OSA)
Obstructive sleep apnea (OSA) is characterized by “episodes of a complete collapse of the airway or partial collapse along with an associated decrease in oxygen saturation or arousal from sleep”. (2022 study [mfn] Slowik, J. M., & Collen, J. F. (2022). Obstructive Sleep Apnea. In StatPearls. StatPearls Publishing. Available here: https://www.ncbi.nlm.nih.gov/books/NBK459252/ [/mfn] ) This causes fragmented and nonrestorative sleep.
II. Cheyne-Stokes respiration
Cheyne-Stokes respiration is “a type of breathing disorder characterized by cyclical episodes of apnea and hyperventilation” (2021 study [mfn] Rudrappa, M., Modi, P., & Bollu, P. C. (2022). Cheyne Stokes Respirations. In StatPearls. StatPearls Publishing. Available here: https://www.ncbi.nlm.nih.gov/books/NBK448165/ [/mfn] ). It is associated with:
- Heart failure
- Stroke
- Other coronary morbidities, etc.
III. Sleep-related hypoventilation disorders
Chronic hypoventilation affects [mfn] Böing, S., & Randerath, W. J. (2015). Chronic hypoventilation syndromes and sleep-related hypoventilation. Journal of thoracic disease, 7(8), 1273–1285. https://doi.org/10.3978/j.issn.2072-1439.2015.06.10 [/mfn] patients with disorders on any level of the respiratory system. It includes health conditions like obesity hypoventilation syndrome, etc., and is associated with poor sleep quality, excessive daytime sleepiness, and morning headaches.
IV. Sleep-related hypoxemia
Hypoxia is “a state in which oxygen is not available in sufficient amounts at the tissue level to maintain adequate homeostasis ”. (2017 study [mfn] Bhutta, B. S., Alghoula, F., & Berim, I. (2022). Hypoxia. In StatPearls. StatPearls Publishing. Available here: https://www.ncbi.nlm.nih.gov/books/NBK482316/ [/mfn] ) In the context of sleep, it causes apnea-like conditions.
V. Isolated symptoms
Isolated symptoms of breathing-related sleep disorders include:
- Snoring
- Catathrenia, etc.
3. Central disorders of hypersomnolence
Hypersomnolence is the inability to stay awake and alert during normal waking hours, resulting in periods of irrepressible need for sleep or becoming drowsy or sleepy without intending to.
Its predominant symptom is excessive daytime sleepiness (EDS) and it is often linked to mild maladaptive behaviors, systemic disorders, and substance abuse. It is of the following types:
I. Narcolepsy
Narcolepsy (2021 study [mfn] Slowik, J. M., Collen, J. F., & Yow, A. G. (2022). Narcolepsy. In StatPearls. StatPearls Publishing. Available here: https://www.ncbi.nlm.nih.gov/books/NBK459236/ [/mfn] ) is a sleep disorder of Rapid Eye Movement (REM) sleep, which involves Excessive Daytime Sleepiness (EDS), frequent uncontrollable attacks of sleep, along with fragmentation or breaks in sleep.
It is also frequently associated with cataplexy, sleep paralysis, and hypnagogic hallucinations. It is of two types, distinguished by the presence or absence of cataplexy.
II. Idiopathic hypersomnia (IH)
Idiopathic hypersomnia (IH) is a chronic neurological disorder that results in daytime sleepiness ( 2018 study [mfn] Trotti L. M. (2017). Idiopathic Hypersomnia. Sleep medicine clinics, 12(3), 331–344. https://doi.org/10.1016/j.jsmc.2017.03.009 [/mfn] ). People with this condition experience long nocturnal or daytime sleep, unrefreshing sleep, difficulty in awakening, cognitive dysfunction, and other autonomic symptoms.
III. Kleine-Levin syndrome (KLS)
Kleine–Levin syndrome (KLS) is also known as the “sleeping beauty syndrome. One 2021 study [mfn] Shah, F., & Gupta, V. (2021). Kleine–Levin syndrome (KLS). In StatPearls. StatPearls Publishing. Available here: https://www.ncbi.nlm.nih.gov/books/NBK568756/ [/mfn] defines it as “a rare yet devastating parasomnia” which includes:
- Recurrent episodes of hypersomnia
- Behavioral or cognitive abnormalities
- Compulsive eating
- Hypersexuality
IV. Insufficient sleep syndrome
Insufficient sleep syndrome [mfn] Chattu, V. K., Sakhamuri, S. M., Kumar, R., Spence, D. W., BaHammam, A. S., & Pandi-Perumal, S. R. (2018). Insufficient Sleep Syndrome: Is it time to classify it as a major noncommunicable disease?. Sleep science (Sao Paulo, Brazil), 11(2), 56–64. https://doi.org/10.5935/1984-0063.20180013 [/mfn] is when you voluntarily restrict your daily sleep time to such an extent that it is less than what is biologically required. It is the foremost cause of excessive daytime sleepiness.
V. Isolated symptoms
Hypersomnolence-like isolated symptoms can also be caused by several factors like medication use, mental and physical illness, etc.
4. Circadian rhythm sleep-wake disorders
Circadian rhythm sleep-wake disorders are caused by disturbances [mfn] Basit, H., Damhoff, T. C., & Huecker, M. R. (2022). Sleeplessness And Circadian Disorder. In StatPearls. StatPearls Publishing. Available here: https://www.ncbi.nlm.nih.gov/books/NBK534238/ [/mfn] to or disruptions in the normal circadian rhythm. It manifests in:
- Delayed sleep-wake phase disorder (DSWPD)
- Advanced sleep-wake phase disorder (ASPD)
- Irregular sleep-wake rhythm
- Non-24-hour sleep-wake rhythm disorder (N24)
- Shift work disorder
- Jet lag disorder
You Can Read More About Body Clock Here
5. Parasomnias
Parasomnias are characterized by abnormal events (verbal or physical) that occur during sleep or while transitioning into sleep. These sleep disorders occur during non-rapid eye movement (NREM) and rapid eye movement (REM) stages of sleep. These are more commonly seen in children than adults. It can be of different types, including:
- Disorders of arousal from NREM sleep
- Recurrent isolated sleep paralysis
- Nightmare disorder
- Nocturnal enuresis, etc.
You Can Read More About Parasomnia Here
6. Sleep-related movement disorders
Sleep-related movement disorders are characterized by simple and repetitive movements during sleep or wake phases that cause sleeplessness. Its types include:
I. Restless leg syndrome (RLS)
Restless legs syndrome or Willis-Ekbom disease [mfn] Mansur, A., Castillo, P. R., Rocha Cabrero, F., & Bokhari, S. (2022). Restless Legs Syndrome. In StatPearls. StatPearls Publishing. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430878/ [/mfn] is a common and chronic “multifactorial movement disorder of the limbs in which patients have an irresistible urge to move the legs.”
II. Periodic limb movement disorder (PLMD)
Periodic limb movements (PLM), according to one 1998 study [mfn] Nozawa T. (1998). Nihon rinsho. Japanese journal of clinical medicine, 56(2), 389–395. [/mfn] , are defined as “stereotyped, periodic movements of the legs and/or upper limbs during sleep”. It is usually associated with –
- Sleep apnea
- Delayed sleep phase syndrome
- Narcolepsy
- Spinal cord tumor
- Diabetes mellitus
- Uremia
III. Sleep-related leg cramps
A person with sleep-related leg cramps experiences leg cramps during sleeping.
IV. Sleep-related bruxism
This is a condition [mfn] Shetty, S., Pitti, V., Satish Babu, C.L. et al. Bruxism: A Literature Review. J Indian Prosthodont Soc 10, 141–148 (2010). https://doi.org/10.1007/s13191-011-0041-5 [/mfn] in which a person grinds, gnashes, or clenches his/her teeth in sleep.
V. Sleep-related rhythmic movement disorder (SRRMD)
Sleep-related rhythmic movements disorder (SRRMD) comprises a group of movement disorders [mfn] DelRosso, L. M., Cano-Pumarega, I., & E, S. (2021). Sleep-Related Rhythmic Movement Disorder. Sleep medicine clinics, 16(2), 315–321. https://doi.org/10.1016/j.jsmc.2021.02.007 [/mfn] like body rocking, head rolling, or headbanging. These occur predominantly early in childhood, though the more chronic cases persist into adulthood.
VI. Sleep myoclonus (BNSM)
According to a 2011 study [mfn] John, B. M., & Patnaik, S. K. (2006). Benign Neonatal Sleep Myoclonus: Is it so Uncommon?. Medical journal, Armed Forces India, 62(2), 186–187. https://doi.org/10.1016/S0377-1237(06)80069-9 [/mfn] , benign neonatal sleep myoclonus (BNSM) is “a self-limiting disorder characterized by neonatal onset myoclonic jerks during non-rapid eye movement (NREM) sleep”.
Diagnosis
The criteria for diagnosing sleep disorders have been laid out in psychiatric manuals like the Diagnostic and Statistical Manual of Mental Disorders (DSM), the International Classification of Sleep Disorders (ICSD), etc. The first step involves a general medical professional examining the patient’s medical history and outlining a working diagnosis.
An accurate and detailed history from the patient, bed partner, or family member combined with a sleep questionnaire can elicit critical information. At this stage, the patient is asked to maintain a 2-week sleep log or a sleep diary and answer a questionnaire that assesses:
- A family history of sleep disorders (such as snoring, narcolepsy, etc.)
- The patient’s pertinent medical/surgical/psychiatric history and past treatments
- The reported symptoms of sleeplessness
- The possible causes for such acute or chronic sleeplessness
- The impact of the sleep complaint on the patient’s life
- The patient’s lifestyle, meal, and sleep schedules—especially his/her sleep hygiene regime
- The patient’s occupational and environmental factors
- The patient’s intake of caffeine, drugs, alcohol, and medication
Based on the questionnaire’s answers, the patient is advised to undergo a series of laboratory tests, such as :
- Polysomnogram (PSG [mfn] Kansagra, S., Ghusayni, R., Kherallah, B., Gunduz, T., McLean, M., Prange, L., Kravitz, R. M., & Mikati, M. A. (2019). Polysomnography Findings and Sleep Disorders in Children With Alternating Hemiplegia of Childhood. Journal of clinical sleep medicine : JCSM : official publication of the American Academy of Sleep Medicine, 15(1), 65–70. https://doi.org/10.5664/jcsm.7572 [/mfn] )
- Multiple sleep latency test (MSLT [mfn] Arand, D. L., & Bonnet, M. H. (2019). The multiple sleep latency test. Handbook of clinical neurology, 160, 393–403. https://doi.org/10.1016/B978-0-444-64032-1.00026-6 [/mfn] )
- Maintenance of wakefulness test (MWT [mfn] Doghramji, K., Mitler, M. M., Sangal, R. B., Shapiro, C., Taylor, S., Walsleben, J., Belisle, C., Erman, M. K., Hayduk, R., Hosn, R., O’Malley, E. B., Sangal, J. M., Schutte, S. L., & Youakim, J. M. (1997). A normative study of the maintenance of wakefulness test (MWT). Electroencephalography and clinical neurophysiology, 103(5), 554–562. https://doi.org/10.1016/s0013-4694(97)00010-2 [/mfn] ), etc.
The patient’s performance in these physical tests, coupled with their sleep diary and questionnaire answers, is used to determine the nature of their sleep disorders. Accordingly, the patient is prescribed treatment for their respective disorder.
Treatment

Studies [mfn] Gupta, R., Das, S., Gujar, K., Mishra, K. K., Gaur, N., & Majid, A. (2017). Clinical Practice Guidelines for Sleep Disorders. Indian journal of psychiatry, 59(Suppl 1), S116–S138. https://doi.org/10.4103/0019-5545.196978 [/mfn] claim that acute sleep disorders can be easily managed with short-term therapy or medication and self-help strategies. However, acute sleep disorders may require serious medical attention—even hospitalization and surgery.
To address chronic sleep disorders, several medical sleeplessness treatment options are available, including:
1. Therapy
Several psychotherapies are available that address sleep disorder symptoms like sleep restrictiveness, sleep disturbances, low sleep quality and quantity, somatic arousal, and stimulus control. These include:
• Relaxation therapies
Relaxation therapies used to correct sleep disorders involve strategies like progressive muscle relaxation, biofeedback techniques, autogenic training (AT), imagery training, thought stopping, etc.
• Cognitive-behavioral therapy for insomnia (CBTi)
CBT techniques include sleep education, sleep hygiene, stimulus control, sleep restriction, relaxation training, and cognitive therapy.
You Can Read More About Cognitive Behavioral Therapy (CBT) Here
• Multicomponent therapy
Multicomponent group intervention programs are often used to treat sleep disorders. These include sub-therapies like light therapy, stimulus control therapy, sleep restriction therapy, etc.
According to a 2011 study [mfn] Schlarb, A. A., Velten-Schurian, K., Poets, C. F., & Hautzinger, M. (2010). First effects of a multicomponent treatment for sleep disorders in children. Nature and science of sleep, 3, 1–11. https://doi.org/10.2147/NSS.S15254 [/mfn] , multicomponent therapies serve to increase the frequency of quickly falling asleep, maintain sleep throughout the night by enhancing the cues for sleep, and decrease the cues for sleep-incompatible behavior.
2. Medication
The onset and course of acute sleep disorders can be successfully checked by short-term medication [mfn] Pagel, J. F., & Parnes, B. L. (2001). Medications for the Treatment of Sleep Disorders: An Overview. Primary care companion to the Journal of clinical psychiatry, 3(3), 118–125. https://doi.org/10.4088/pcc.v03n0303 [/mfn] . Such pharmacological interventions are primarily used to regulate levels [mfn] Lie, J. D., Tu, K. N., Shen, D. D., & Wong, B. M. (2015). Pharmacological Treatment of Insomnia. P & T : a peer-reviewed journal for formulary management, 40(11), 759–771. [/mfn] of cortisol and adrenocorticotropic hormone (ACTH) in poor sleepers and reduce the symptoms of sleep disorders. Only consider medical drugs prescribed by a licensed medical practitioner, such as:
- Benzodiazepine receptor agonists (BzRAs)
- Nonbenzodiazepine hypnotics
- Melatonin receptor agonists, etc.
3. Non-medical interventions
Several non-medical interventions are used to treat sleep disorders. Such techniques reduce stress, induce calm and mindfulness, and promote relaxation and sleep [mfn] Poerio, G. L., Blakey, E., Hostler, T. J., & Veltri, T. (2018). More than a feeling: Autonomous sensory meridian response (ASMR) is characterized by reliable changes in affect and physiology. PloS one, 13(6), e0196645. https://doi.org/10.1371/journal.pone.0196645 [/mfn] . These include:
- Autonomous Sensory Meridian Response (ASMR) techniques [mfn] Fredborg, B. K., Clark, J. M., & Smith, S. D. (2018). Mindfulness and autonomous sensory meridian response (ASMR). PeerJ, 6, e5414. https://doi.org/10.7717/peerj.5414 [/mfn] in videos, podcasts, hand gestures, etc.
- Stress management strategies (like yoga [mfn] Bankar, M. A., Chaudhari, S. K., & Chaudhari, K. D. (2013). Impact of long term Yoga practice on sleep quality and quality of life in the elderly. Journal of Ayurveda and integrative medicine, 4(1), 28–32. https://doi.org/10.4103/0975-9476.109548 [/mfn] , meditation [mfn] Rusch, H. L., Rosario, M., Levison, L. M., Olivera, A., Livingston, W. S., Wu, T., & Gill, J. M. (2019). The effect of mindfulness meditation on sleep quality: a systematic review and meta-analysis of randomized controlled trials. Annals of the New York Academy of Sciences, 1445(1), 5–16. https://doi.org/10.1111/nyas.13996 [/mfn] , massages [mfn] Hachul, H., Oliveira, D. S., Bittencourt, L. R., Andersen, M. L., & Tufik, S. (2014). The beneficial effects of massage therapy for insomnia in postmenopausal women. Sleep science (Sao Paulo, Brazil), 7(2), 114–116. https://doi.org/10.1016/j.slsci.2014.09.005 [/mfn], etc.)
Self-Help Tips
The following coping strategies can help you overcome or reduce the risk of sleep disorders:
1. A healthy sleep-hygiene regime
- Educate yourself about good sleep hygiene practices
- Establish a realistic sleep schedule and maintain this sleep timing with regularity every night
- Abstain from daytime napping and resort to “power naps”, if necessary
- Maintain low light levels and comfortable temperature settings in the bedroom
- Create a comfortable sleeping environment with mattresses, pillows, curtains, rugs, etc.
- Maintain a data sheet for body type, sleep preferences, and the best sleep positions
- Limit “screen time” before bedtime
- Consider activities like sex, cold shower, massages, etc. that enhance sleep
2. Other self-help strategies
- Get adequate physical exercise throughout the day
- Try a dental guard (to prevent teeth grinding during sleep)
- Consider mindfulness activities like meditation, yoga, massage, etc.
- Maintain a healthy weight
- Abstain from large meals and consumption of alcohol or caffeine in the hours leading to bedtime
- Avoid consumption of tobacco, nicotine, etc.
- Try home remedies for sleeplessness like food items that enhance sleep, such as nuts, white rice, milk products, fatty fish, lavender oil, chamomile tea, etc.
Prevalence
According to recent research [mfn] Karna, B., Sankari, A., & Tatikonda, G. (2022). Sleep Disorder. In StatPearls. StatPearls Publishing. Available here: https://www.ncbi.nlm.nih.gov/books/NBK560720/ [/mfn], 50–60% [mfn] Bhaskar, S., Hemavathy, D., & Prasad, S. (2016). Prevalence of chronic insomnia in adult patients and its correlation with medical comorbidities. Journal of family medicine and primary care, 5(4), 780–784. https://doi.org/10.4103/2249-4863.201153 [/mfn] of people worldwide are affected by sleeplessness. It is a particularly common concern in people with other physical and mental health conditions and the elderly populace.
Nonetheless, some sleep disorders are more common than others. For instance, women have a lifetime prevalence of insomnia 40% [mfn] Yazdi, Z., Sadeghniiat-Haghighi, K., Loukzadeh, Z., Elmizadeh, K., & Abbasi, M. (2014). Prevalence of Sleep Disorders and Their Impacts on Occupational Performance: A Comparison between Shift Workers and Nonshift Workers. Sleep disorders, 2014, 870320. https://doi.org/10.1155/2014/870320 [/mfn] higher than men. About 30-48% [mfn] Bhaskar, S., Hemavathy, D., & Prasad, S. (2016). Prevalence of chronic insomnia in adult patients and its correlation with medical comorbidities. Journal of family medicine and primary care, 5(4), 780–784. https://doi.org/10.4103/2249-4863.201153 [/mfn] of older groups also suffer from insomnia.
Moreover, men experience greater instances of sleep apnea [mfn] Slowik, J. M., Sankari, A., & Collen, J. F. (2022). Obstructive Sleep Apnea. In StatPearls. StatPearls Publishing. Available here: https://www.ncbi.nlm.nih.gov/books/NBK459252/ [/mfn] than women. Additionally, some sleep disorders are specifically associated with children, such as sleep enuresis [mfn] Gomez Rincon, M., Leslie, S. W., & Lotfollahzadeh, S. (2022). Nocturnal Enuresis. In StatPearls. StatPearls Publishing. Available Here: https://www.ncbi.nlm.nih.gov/books/NBK545181/ [/mfn] , nightmare disorder [mfn] Gieselmann, A., Ait Aoudia, M., Carr, M., Germain, A., Gorzka, R., Holzinger, B., Kleim, B., Krakow, B., Kunze, A. E., Lancee, J., Nadorff, M. R., Nielsen, T., Riemann, D., Sandahl, H., Schlarb, A. A., Schmid, C., Schredl, M., Spoormaker, V. I., Steil, R., van Schagen, A. M., … Pietrowsky, R. (2019). Aetiology and treatment of nightmare disorder: State of the art and future perspectives. Journal of sleep research, 28(4), e12820. https://doi.org/10.1111/jsr.12820 [/mfn], etc.
Takeaway
Sleep disorders are a growing public health concern, affecting millions of children and adults worldwide. If left untreated, these can negatively impact our quality of life and social relationships. Therefore, timely diagnosis and the right treatment options should be availed to address the negative effects of sleep disorders.
At A Glance
- Sleep disorders are a group of health conditions that disturb normal sleep patterns.
- These constitute a common clinical problem that impacts our everyday functioning.
- The common symptoms of sleep disorders include the inability to stay awake or asleep.
- Some common sleep disorders include insomnia, sleep apnea, narcolepsy, sleep-related movement disorders, etc.
- Sleep disorders are caused by factors like genetics, erratic lifestyle, health conditions, etc.
- These disorders can be easily treated with therapy, medication, and self-help methods.
Frequently Asked Questions (FAQs)
1. Is narcolepsy a sleep disorder?
Narcolepsy is a chronic sleep disorder in which the sufferers experience overwhelming daytime drowsiness and sudden attacks of sleep. They often find it difficult to stay awake for long periods of time too.
2. What is the best trick to sleep quickly at night?
Try breathing exercises, follow a good sleep hygiene regime, and take melatonin supplements to sleep quickly at night.
3. What is an extremely rare sleep disorder?
Kleine-Levin syndrome is one of the most rapid and rare sleep disorders, in which the sufferer experiences the need for excessive amounts of sleep, excessive eating, and behavioral abnormalities.
4. Can dreams cause sleep disorders?
Dreams cannot cause sleep disorders. However, in certain REM sleep behavior disorders, a person may vividly act out their dreams with vocal sounds and sudden limb movements.
5. Which sleep disorders are more common among men than women?
Some of the disorders that occur more in men are sleep apnea, narcolepsy and delayed sleep-wake disorders.
6. Which sleep disorder occurs more in children than adults?
Sleep terrors and nightmares occur more in children, and may stop as the person grows into adulthood.
7. Are sleep disorders multifactorial?
Yes. Sleep disorders have multiple causes and influences associated with them.
8. Are sleep disorders permanent?
Acute sleep disorders are not permanent. But, when these disorders follow a more chronic course (like long-term insomnia, sleepwalking, narcolepsy, etc.) due to lack of treatment, then these are considered incurable and permanent.
9. Why more people with sleep disorders are seeking sleep therapy?
Growing awareness about the long-term consequences of sleep disorders and how it impacts our personal and professional lives is making many people with sleep disorders seek therapy.








Leave a Reply