Table of Contents
Bipolar disorder is a psychological condition that involves extreme changes in mood, behavior, and energy levels, leading to severe disruptions in daily life. However, with effective treatment, one can cope with its symptoms and live a productive life.
What Is Bipolar Disorder?
Bipolar disorder (BD) is a mood disorder, characterized by repeated episodes of depression and unnaturally elevated mood along with changes in levels of energy and activity. These episodes may last from several days to weeks. Also known as bipolar affective disorder, manic depressive illness or manic depression, BD can lead to drastic changes in thinking, judgment, memory, behavior, and sleep.
Although a lot of us have occasional mood swings, people with bipolar disorder experience them in an overwhelming and severe manner. This can disrupt their daily functioning and affect their education, career and personal relationships [mfn] Grover, S., Nehra, R., & Thakur, A. (2017). Bipolar affective disorder and its impact on various aspects of marital relationship. Industrial psychiatry journal, 26(2), 114–120. https://doi.org/10.4103/ipj.ipj_15_16 [/mfn]. A 2019 study [mfn] Dome, P., Rihmer, Z., & Gonda, X. (2019). Suicide Risk in Bipolar Disorder: A Brief Review. Medicina (Kaunas, Lithuania), 55(8), 403. https://doi.org/10.3390/medicina55080403 [/mfn] found that the risk of suicide was 10-30 times higher in people with bipolar disorder than in normal people.
Bipolar disorder usually begins during a person’s late teen or early adult years. However, children can also suffer from the condition and it may last a lifetime. Moreover, several comorbid conditions, like anxiety disorders and substance use disorders, are related to BD.
Unfortunately, BD tends to get worse without treatment. Thus, early diagnosis and treatment under a mental health professional is crucial for the effective management of bipolar disorder symptoms.
People with this disorder can be treated effectively with psychological counseling and/or medication depending on the symptoms.
Case Example
Let’s consider the example of Shreya, a 25 year old writer.
People who knew Shreya often described her as “moody”.
There were times when she was highly energetic, and there was nothing that could bring her enthusiasm down. She’d be extremely chatty and overflow with ideas, a lot of which proved to be impractical.
Sometimes, she even talked about becoming the greatest author the world has ever known. On such occasions, Shreya would frequently take up more projects than she could handle.
However, these phases approximately lasted a week. They were mostly followed by days where she was barely productive and hardly spoke to anyone. She would also eat significantly lesser than usual.
In stark contrast to her enthusiastic attitude, Shreya could be heard saying things like, “There is no point to anything, why even work?” and was sometimes even found sleeping at her desk.
These mood fluctuations, that had been a part of Shreya’s life for the past 6 years, were typical of Bipolar I mood disorder.
Symptoms Of Bipolar Disorder
BD is characterized by cognitive deficits and affective instability. Symptoms of bipolar disorder can be different for each patient as the disorder varies widely in frequency, severity, and pattern. Some may experience highs and lows in quick succession while others may experience episodes that last for months or even years.
Listed below are some of the most common manic and depressive symptoms of bipolar disorder:
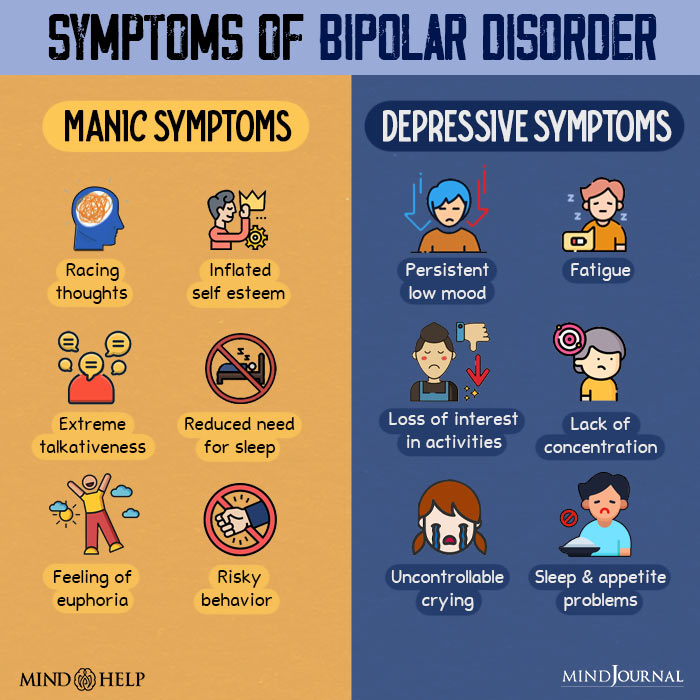
A. Manic symptoms
Mania or hypomania are characterized by elevated moods. Hypomania is milder in intensity than mania. According to the American Psychiatric Association [mfn] American Psychological Association. (2015, February 15). Recognizing the signs of bipolar disorder. https://www.apa.org/topics/bipolar-disorder/recognizing [/mfn], manic episodes in BD usually last at least a week wherein the person is excessively irritable or extremely high spirited. They display at least three of the following symptoms:
- Intrusive, unmanageable racing thoughts and rapidly changing topics or ideas
- Inflated self-esteem or an exaggerated sense of grandiosity
- Reduced need for sleep
- Getting distracted easily
- Increased risky behavior
- Being highly talkative or speaking rapidly and loudly
- Engaging more activities or events at once than can be completed
Mania or hypomania also involves these additional symptoms, including:
- Jumpy or upbeat behavior
- Extremely high levels of energy
- Flawed judgment and poor decision-making
- Psychotic symptoms, including delusions and hallucinations
- Boredom
- Aggression
- Increased libido leading to unprotected sex
- Euphoria
- Incoherent speech
- Exaggerated self-confidence and self-importance
- Spending sprees
- Substance abuse, like alcoholism, drug abuse, etc.
2. Depressive symptoms
According to the American Psychiatric Association [mfn]American Psychological Association. (2015, February 15). Recognizing the signs of bipolar disorder. https://www.apa.org/topics/bipolar-disorder/recognizing [/mfn], an episode of major depression tends to last for two weeks and involves at least five of the following symptoms:
- Extreme despair or sadness
- Feelings of worthlessness
- Sense of hopelessness and helplessness
- Guilt
- Shame
- Loss of interest in pleasurable activities
- Disturbed sleeping patterns, like insomnia or oversleeping
- Agitation
- Restlessness
- Slurred speech
- Restricted body movement
- Changes in appetite
- Chronic fatigue, exhaustion, or loss of energy
- Poor concentration
- Chronic forgetfulness
- Suicidal ideation
- Self harm
Read More About Guilt Here
A patient in a depressive episode of bipolar disorder also experiences the following symptoms:
- Uncontrollable weeping
- Weight gain or weight loss
- Indecisiveness or difficulty in making decisions
- Anxiety about insignificant issues
- Irritability
- Listlessness
- Lack of interest in work or school, leading to underperformance
- High sensitivity to sensory stimuli
Experts believe bipolar disorder should be considered as a spectrum of moods. At one end of the spectrum is severe to mild depression, while mania and hypomania are at the other end. Surprisingly, a balanced and normal mood also lies in the middle of the spectrum as well.
Some individuals may experience symptoms of both mania and depression at the same time – this is known as a mixed bipolar state.
Read More About Depression Here
Types Of Bipolar Disorder
Depending on the frequency, severity, and presence of symptoms, a person may be diagnosed with different types of bipolar disorder. Here are the major types of bipolar disorders based on the Diagnostic and Statistical Manual of Mental Disorders (DSM) 5 [mfn] American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.) [/mfn] that may be used by doctors to diagnose a patient:
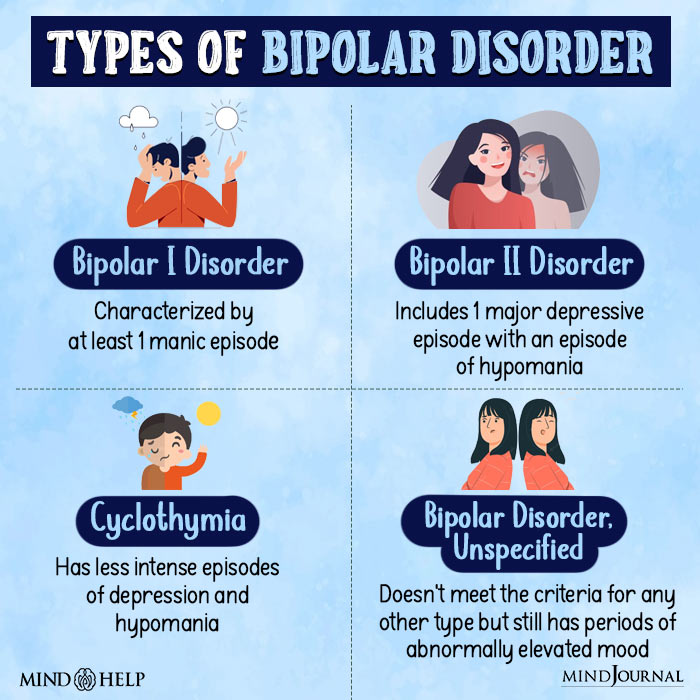
1. Bipolar I disorder (manic or mixed episode)
According to a 2007 study, [mfn] Keener, M. T., & Phillips, M. L. (2007). Neuroimaging in bipolar disorder: a critical review of current findings. Current psychiatry reports, 9(6), 512–520. https://doi.org/10.1007/s11920-007-0070-2 [/mfn] “bipolar I disorder (BPI) is among the top 10 most debilitating illnesses globally.” It is marked by at least one episode of mania. Periods of major depression or hypomania may also occur before or after the manic episode.
This type of BD can often lead to dramatic mood swings and make the person feel as if they are on top of the world. It may also trigger psychosis. However, periods of normal moods are common between such episodes.
Bipolar I disorder requires that the patient must experience a manic episode for at least 7 days or the episode must be severe enough to necessitate hospitalization. However, the symptoms must not be caused by any other mental conditions, like delusional disorder or schizophrenia.
Studies [mfn] Bebbington, P., & Ramana, R. (1995). The epidemiology of bipolar affective disorder. Social psychiatry and psychiatric epidemiology, 30(6), 279–292. https://doi.org/10.1007/BF00805795 [/mfn] reveal that lifetime prevalence of bipolar disorder type 1 is around 1% in the general population.
2. Bipolar II disorder (hypomania and depression)
Individuals with this variant of BD experience an episode of major depression which may sustain for two weeks or more, and a period of hypomania which can last up to four days.
It has been observed that bipolar II disorder is more common in female patients than in males [mfn] Arnold L. M. (2003). Gender differences in bipolar disorder. The Psychiatric clinics of North America, 26(3), 595–620. https://doi.org/10.1016/s0193-953x(03)00036-4 [/mfn]. Contrary to popular belief, this is not a milder version of bipolar I disorder; it is a distinct subtype with its own diagnostic criteria.
Individuals with bipolar II disorder usually do not experience a full-blown manic episode, and depression often dominates their mood [mfn] Bipolar Disorder. (n.d.). National Institute of Mental Health (NIMH); www.nimh.nih.gov. Retrieved August 26, 2022, from https://www.nimh.nih.gov/health/topics/bipolar-disorder [/mfn]. During a hypomanic episode, a person may feel normal and function effectively, but depressive episodes are characterized by unstable and volatile moods.
The mood shifts of bipolar II disorder are very different from mood disorders caused by other mental conditions or medications. Yet, even though the symptoms of bipolar II disorder are milder, these are often accompanied by a plethora of symptoms linked to depression, anxiety, or substance abuse. This condition generally doesn’t require hospitalization.
Read More About Anxiety Here
3. Cyclothymic disorder (hypomania and mild depression)
Cyclothymia is characterized by less intense and shorter episodes of depression and hypomania. Its symptoms are milder than bipolar I and bipolar II disorders.
People with this condition experience several episodes of hypomania and depression, lasting for at least two years, with brief episodes of normal mood in between lasting less than 8 weeks [mfn] Bipolar Disorder. (n.d.). National Institute of Mental Health (NIMH); www.nimh.nih.gov. Retrieved August 26, 2022, from https://www.nimh.nih.gov/health/topics/bipolar-disorder [/mfn].
Nonetheless, most of the time, the symptoms of cyclothymia fail to meet the criteria established for hypomanic or depressive episodes. During this 2–year period, the mood swings sustain for at least 50% of the time, without ceasing for over 2 months.
Although many people with this condition avoid seeking help under the impression that the symptoms are not serious enough, cyclothymia can have severe effects in a person’s relationships, career and quality of life.
Read More About Hypomania Here
4. Bipolar Disorder, “other specified” and “unspecified”
Research shows that there are multiple types of “unspecified” bipolar disorders in which a person does not meet the criteria for either bipolar I, II, or cyclothymia.
But they still experience periods of clinical mood elevation and suffer from health disorders triggered by substance abuse, a psychiatric illness, or a medical condition (such as a stroke, multiple sclerosis, or Cushing’s disease) [mfn] Duckworth, K. (2017). Bipolar disorder . National Alliance on Mental Illness; www.nami.org. https://www.nami.org/About-Mental-Illness/Mental-Health-Conditions/Bipolar-Disorder#:~:text=Bipolar%20Disorder%2C%20%E2%80%9Cother%20specified%E2%80%9D,clinically%20significant%20abnormal%20mood%20elevation. [/mfn]
Bipolar Disorder Diagnosis
As of now, there is no medical test to diagnose bipolar disorder [mfn] Gomez-Casati, D., Grisolía, M., & Busi, M. (2016). The significance of Metabolomics in human health. Medical and Health Genomics, 89-100. https://doi.org/10.1016/b978-0-12-420196-5.00007-1 [/mfn]. A mental health professional, such as a psychologist or a psychiatrist, usually takes a detailed history of the person, along with a mental status examination (MSE), and conducts certain psychometric assessments [mfn] Miller, C. J., Johnson, S. L., & Eisner, L. (2009). Assessment Tools for Adult Bipolar Disorder. Clinical psychology : a publication of the Division of Clinical Psychology of the American Psychological Association, 16(2), 188–201. https://doi.org/10.1111/j.1468-2850.2009.01158.x [/mfn] in order to arrive at a diagnosis. Some of these include :
- Structured Clinical Interview for DSM IV (SCID)
- Schedule for Affective Disorders and Schizophrenia (SADS)
- Mood Disorder Questionnaire, etc.
Read More About Schizophrenia Here
Certain other tests may also be recommended such as a blood test, thyroid level test, protein levels test, substance, and alcohol screening, etc. in order to rule out other causes for the symptoms.
To be diagnosed with BD:
- You must have experienced at least one episode of mania or hypomania.
- For mania, the elevated or irritable mood must persist for at least 7 consecutive days and be experienced almost every day.
- For hypomania, the elevated mood must persist for at least 4 consecutive days and be experienced almost every day.
Diagnosing bipolar disorder accurately and timely can significantly help to manage the condition and improve the prognosis for the patient [mfn] Culpepper L. (2014). The diagnosis and treatment of bipolar disorder: decision-making in primary care. The primary care companion for CNS disorders, 16(3), PCC.13r01609. https://doi.org/10.4088/PCC.13r01609 [/mfn] However, due to the diversity of symptoms, proper bipolar disorder diagnosis can often be a challenge.
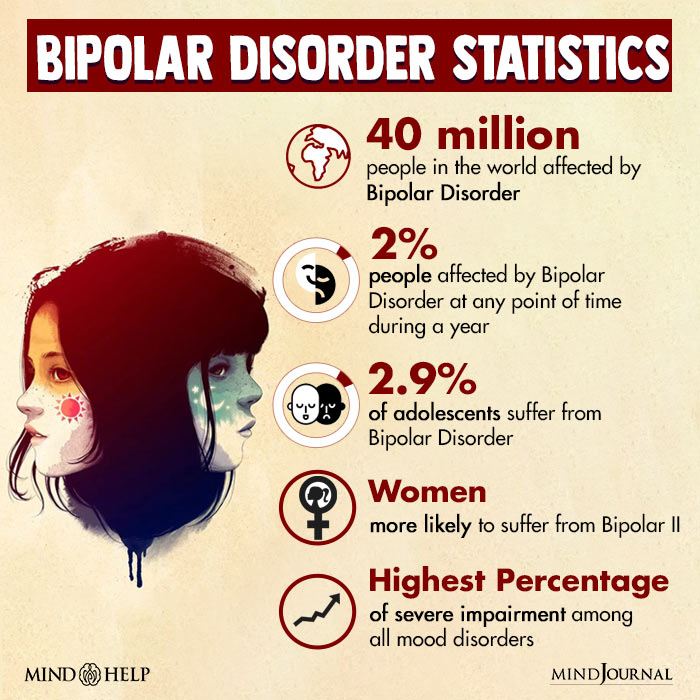
How Common Is Bipolar Disorder?
Bipolar disorder statistics [mfn] Bipolar disorder | NEJM. (2020, July 1). New England Journal of Medicine. https://www.nejm.org/doi/full/10.1056/NEJMra1906193 [/mfn] indicate that it has a yearly prevalence of 2%. It has the highest percentage [mfn] Kessler, R. C., Chiu, W. T., Demler, O., Merikangas, K. R., & Walters, E. E. (2005). Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Archives of general psychiatry, 62(6), 617–627. https://doi.org/10.1001/archpsyc.62.6.617 [/mfn] of severe impairment amongst all mood disorders.
Around 2.9% of adolescents are living with bipolar disorder. According to a 2011 survey, [mfn] Merikangas, K. R., Jin, R., He, J. P., Kessler, R. C., Lee, S., Sampson, N. A., Viana, M. C., Andrade, L. H., Hu, C., Karam, E. G., Ladea, M., Medina-Mora, M. E., Ono, Y., Posada-Villa, J., Sagar, R., Wells, J. E., & Zarkov, Z. (2011). Prevalence and correlates of bipolar spectrum disorder in the world mental health survey initiative. Archives of general psychiatry, 68(3), 241–251. https://doi.org/10.1001/archgenpsychiatry.2011.12 [/mfn] the prevalence for bipolar type 1 was around 0.6% and for bipolar type 2, it was about 0.4%. Men and women tend to be affected at the same rate. [mfn] Diflorio, A., & Jones, I. (2010). Is sex important? Gender differences in bipolar disorder. International review of psychiatry (Abingdon, England), 22(5), 437–452. https://doi.org/10.3109/09540261.2010.514601 [/mfn]
Co-existing Disorders
Bipolar disorder is associated with an increased risk of medical illnesses. [mfn] Forty, L., Ulanova, A., Jones, L., Jones, I., Gordon-Smith, K., Fraser, C., Farmer, A., McGuffin, P., Lewis, C. M., Hosang, G. M., Rivera, M., & Craddock, N. (2014). Comorbid medical illness in bipolar disorder. The British journal of psychiatry : the journal of mental science, 205(6), 465–472. https://doi.org/10.1192/bjp.bp.114.152249 [/mfn] and multiple lifelong psychiatric disorders [mfn] McElroy, S. L., Altshuler, L. L., Suppes, T., Keck, P. E., Jr, Frye, M. A., Denicoff, K. D., Nolen, W. A., Kupka, R. W., Leverich, G. S., Rochussen, J. R., Rush, A. J., & Post, R. M. (2001). Axis I psychiatric comorbidity and its relationship to historical illness variables in 288 patients with bipolar disorder. The American journal of psychiatry, 158(3), 420–426. https://doi.org/10.1176/appi.ajp.158.3.420 [/mfn].
Some of these comorbid conditions include:
- Attention-deficit hyperactivity disorder (ADHD)
- Post-traumatic stress disorder (PTSD)
- Obsessive-compulsive disorder (OCD)
- Psychosis
- Anxiety disorders
- Personality disorders
- Impulse control disorders, etc.
Read More About Attention Deficit Hyperactivity Disorder (ADHD) Here
Bipolar disorder treatment is often plagued by misdiagnosis, particularly when it comes to ‘comorbid’ symptoms [mfn] Keller M. B. (2006). Prevalence and impact of comorbid anxiety and bipolar disorder. The Journal of clinical psychiatry, 67 Suppl 1, 5–7. [/mfn] of other disorders. This may worsen the symptoms, make the treatment process difficult, and lead to a poor prognosis of the condition.
- Read More About Causes Of Bipolar Disorder Here
- Read More About Treatment of Bipolar Disorder Here
Takeaway
Bipolar disorder is a serious yet common psychiatric illness that can affect a person’s mood, behavior, and energy levels. Although it can severely disrupt the daily functioning of the patient when left untreated, ongoing and appropriate treatment can be significantly helpful in managing symptoms, stabilizing their moods, and improving the quality of their life.
At A Glance
- Bipolar disorder (BD) is a condition that leads to extreme changes in mood, behavior, and energy levels.
- Around 1% of the global population is affected by it.
- People with BD have extreme and intense emotional states that occur at distinct times, called mood episodes.
- The mood episodes are categorized as manic, hypomanic, or depressive.
- A person with BD may experience periods of depression more frequently than periods of mania or vice versa.
- Bipolar disorder is associated with a high risk of suicide.
- BD is a recurrent chronic disorder that requires long-term treatment and ongoing care.
Frequently Asked Questions (FAQs)
1. Can children have bipolar disorder?
Yes, children can be diagnosed with bipolar disorder [mfn] Renk, K., White, R., Lauer, B. A., McSwiggan, M., Puff, J., & Lowell, A. (2014). Bipolar disorder in children. Psychiatry journal, 2014, 928685. https://doi.org/10.1155/2014/928685 [/mfn]. However, as they don’t typically show the same symptoms as adults, identifying or diagnosing the condition in them can be challenging. In children, bipolar disorder symptoms can often be confused with that of ADHD and other disorders.
2. Who are some of the famous people with bipolar disorder?
Catherine Zeta-Jones, Kurt Cobain, Graham Greene, Nina Simone, Winston Churchill, and Demi Lovato are some of the famous people who are believed to have suffered from bipolar disorders.
3. Is bipolar disorder curable?
Bipolar disorder, like any other complex mood disorder, may not be completely cured. However, it can be easily managed with therapies, medication, etc.
4. How common is bipolar disorder in men?
As per recent data, the prevalence of bipolar disorder in adult males is 2.9%. [mfn] Harvard Medical School, 2007. National Comorbidity Survey (NSC). (2017, August 21). Retrieved from https://www.hcp.med.harvard.edu/ncs/index.php [/mfn]
5. What percentage of the world suffers from bipolar disorder?
As per research, [mfn] Bipolar disorder. (n.d.). ScienceDirect.com | Science, health and medical journals, full text articles and books. https://www.sciencedirect.com/science/article/abs/pii/S014067361500241X [/mfn] around 1% of the global population is affected by bipolar disorder.
6. What population is most at risk for bipolar disorder?
People around the age of 15-24 and 45-54 are most at risk for bipolar disorder, although it can develop at any age. Moreover, people who have family members suffering from mood disorders, have other comorbid conditions or were maltreated as children are also at risk of developing BD. [mfn] Rowland, T. A., & Marwaha, S. (2018). Epidemiology and risk factors for bipolar disorder. Therapeutic advances in psychopharmacology, 8(9), 251–269. https://doi.org/10.1177/2045125318769235 [/mfn]
7. Can people with bipolar disorder completely control their mood swings?
People with bipolar disorder are not in complete control of their mood swings. However, various pharmacological and psychological treatments are available that can help them manage their symptoms better.