Schizophrenia is a severe psychiatric disorder that affects a person’s thoughts, perceptions, behaviour, and how they perceive reality.
What Is Schizophrenia?
Schizophrenia is a mental disorder involving hallucinations (perceiving things that aren’t actually present) and delusions (false beliefs about oneself and the world).
It is also characterized by thought disorders and dysfunctions in speech, movement, and behavior. Schizophrenia can have a disabling effect on the people suffering from it. However, the severity of the condition mostly depends on individual factors.
The term “schizophrenia” was originally coined in 1908 by Swiss psychiatrist Eugen Bleuler 1 Kahn R. S. (2020). On the Origins of Schizophrenia. The American journal of psychiatry, 177(4), 291–297. https://doi.org/10.1176/appi.ajp.2020.20020147 . It is derived from the Greek words schizo meaning “splitting” and phren meaning “mind”.
Case Example
Mr. Mehra had retired from his job as a Manager about 5 years ago and had been living alone since then. His children were working in different cities and would come to visit him about once a year.
For the past 6 months, a generally extroverted Mr. Mehra had been showing increasing signs of social withdrawal. On more than one occasion, his househelp found him talking to the walls as though someone was actually there. He often complained that he could hear the neighbor’s son taunting him every time he got up to do anything – such as open his cupboard, or take a book from the shelf. This constantly hindered his daily activities. It was clear that the taunts that Mr. Mehra was hearing was not real; however, he would get extremely agitated if his claims were ever challenged and would accuse everybody of plotting against him. He was quite convinced that the entire world was coming to get him.
Soon, he was beginning to appear quite disheveled and was gradually losing a sense of what was real and what wasn’t. After a failed attempt at taking his own life, Mr. Mehra was admitted to the hospital.
Case Analysis
From the case study, it is evident that Mr. Mehra has been experiencing hallucinations (seeing/ hearing things that others can’t) and paranoid delusions about the neighbor’s son being after him and the entire world being against him. These are classic symptoms of schizophrenia of the paranoid type.
Early Warning Signs Of Schizophrenia
Schizophrenia can occur at any age and can last from months to years. The initial signs differ depending on age and gender. The period in which early warning signs are experienced is called the prodromal stage 2 George, M., Maheshwari, S., Chandran, S., Manohar, J. S., & Sathyanarayana Rao, T. S. (2017). Understanding the schizophrenia prodrome. Indian journal of psychiatry, 59(4), 505–509. https://doi.org/10.4103/psychiatry.IndianJPsychiatry_464_17 .
For instance, in children, the early signs include severe developmental delay (like slow motor development, delay in speech, etc.) and impaired social development. In adolescents, young adults, and elderly people, the initial signs and symptoms of schizophrenia are more or less similar. Some of these include:
- Agitation
- Mood disorders
- Social withdrawal
- Severe anxiety
- Sluggishness
- Disorganized thinking
- Bizarre behavior
- Suicidal ideations
Signs And Symptoms Of Schizophrenia
The symptoms of schizophrenia tend to vary in duration, intensity, and frequency—depending on the individual.
Experts 3 Hany, M., Rehman, B., Azhar, Y., & Chapman, J. (2022). Schizophrenia. In StatPearls. StatPearls Publishing. Available from: https://www.ncbi.nlm.nih.gov/books/NBK539864/ categorize the symptoms of schizophrenia into the following 3 groups:
1. Positive symptoms of schizophrenia
The positive symptoms of schizophrenia are those which are abnormally present. These mostly include
- Hallucinations
- Delusions
- Disorganized speech
- Disorganized behavior
2. Negative symptoms of schizophrenia
Negative symptoms associated with schizophrenia generally include
- Flattened affect
- Lack of interest in previously pleasurable activities
- Reduced speech
- Lack of initiative
- Reduced energy
3. Cognitive symptoms of schizophrenia
The common cognitive symptoms of schizophrenia include
- Irritability and a lack of concentration
- Memory problems (like amnesia)
- Difficulty in planning and structuring activities
- Difficulty in processing information & making decisions
- Lack of insight
- Volatile behavior (related to anger and violence)
Types Of Schizophrenia
The common types 4 Wy , T., & Saadabadi, A. (2022). Schizoaffective Disorder. In StatPearls. StatPearls Publishing. Available from: https://www.ncbi.nlm.nih.gov/books/NBK541012/ of schizophrenia include:
1. Paranoid schizophrenia
This type is characterized by positive symptoms of schizophrenia—involving repeated frequent visual or auditory hallucinations and one or more delusions.
Continue Reading About Paranoid Schizophrenia
2. Disorganized schizophrenia
Also known as Hebephrenia, this subtype is marked by disorganized speech and behavior. It may also involve impairment in the emotional expression or reactions of the patient. Although hallucinations and delusions may occur, they are not very prominent.
Continue Reading About Disorganized Schizophrenia

3. Catatonic schizophrenia
Catatonic schizophrenia is characterized by noticeable abnormal motor behavior. This may involve a substantial decrease in voluntary movement or agitation and hyperactivity. Motor behavior in this type of schizophrenia can range from stupor (extreme immobility) to waxy flexibility.
4. Undifferentiated schizophrenia
This type of schizophrenia is characterized by vague symptoms. The patient may behave in ways that can be seen in two or more of the other subtypes of schizophrenia. This can involve symptoms like hallucinations, delusions, paranoia, catatonic behavior, and disorganized speech or behavior.
5. Residual schizophrenia
This subtype is often considered the ‘recovery phase’ in which severe symptoms usually begin to fade. Residual schizophrenia occurs when a person, previously affected by at least one schizoid episode, has reduced or no symptoms; however, the person may still feel paranoid or have strange beliefs, or may be socially withdrawn.
What Causes Schizophrenia?
Schizophrenia causes are multiple, covering a wide range of genetic and environmental factors. These include:
1. Genetic factors
Genetics plays a vital role in the onset of schizoaffective disorders. People with a history of schizophrenia or other mental disorders (like depression, psychosis, bipolar disorders, etc.) are at a greater risk of schizophrenia.
However, no single gene has yet been identified and this makes genetic information unreliable when anticipating if someone may develop the disorder.
2. Factors related to brain structure and function
Research 5 Syvälahti E. K. (1994). Biological factors in schizophrenia. Structural and functional aspects. The British journal of psychiatry. Supplement, (23), 9–14. shows that structural and functional changes in the brain can make a person vulnerable to schizophrenia. These include:
- Changes in certain brain regions (like the hippocampus, parahippocampal gyrus, amygdala, etc.)
- Dysfunctional neurotransmitters (like dopamine and serotonin abnormalities)
- Viral and bacterial infections
- Traumatic brain injury
3. Environmental factors
Common psychosocial factors associated with schizophrenia include:
- Poverty
- Stressful surroundings
- Exposure to toxins
- Unhealthy lifestyle
- Experiences of trauma
- Negative developmental experiences (like grief, war, invasion, terrorism, etc.)
- A family history of mental disorders (like substance use disorders, psychosis, etc.)
Schizophrenia Diagnosis
According to the Diagnostic and Statistical Manual for Mental Disorders (DSM- 5 6 Substance Abuse and Mental Health Services Administration. (2016). Impact of the DSM-IV to DSM-5 Changes on the National Survey on Drug Use and Health. Substance Abuse and Mental Health Services Administration (US). Available from: https://www.ncbi.nlm.nih.gov/books/NBK519704/table/ch3.t22/ ), schizophrenia can be diagnosed if a person has been suffering from at least two of the following for a period of one month or more:
- Delusions
- Hallucinations
- Disorganization in speech
- Disorganization in behavior (catatonic stupor/ waxy flexibility)
- Decreased activity and emotional expression
The symptoms must result in significant distress and impairment in functioning. Moreover, they should not be a result of other mental illnesses or substance use.
A mental health professional arrives at a diagnosis after a careful examination of the symptoms and past history of the individual. Certain assessments such as the Positive and Negative Symptoms Scale (PANSS) and Clinical Global Impression Schizophrenia (CGI-SCH) may also be used to confirm the diagnosis 7 Kumari, S., Malik, M., Florival, C., Manalai, P., & Sonje, S. (2017). An Assessment of Five (PANSS, SAPS, SANS, NSA-16, CGI-SCH) commonly used Symptoms Rating Scales in Schizophrenia and Comparison to Newer Scales (CAINS, BNSS). Journal of addiction research & therapy, 8(3), 324. https://doi.org/10.4172/2155-6105.1000324 .
Treatment For Schizophrenia
Schizophrenia may have a life-long prevalence and, if left untreated, can negatively impact your personal, professional, and social life. But, the lack of a definitive schizophrenia treatment regime, the ambiguity 8 Jablensky A. (2010). The diagnostic concept of schizophrenia: its history, evolution, and future prospects. Dialogues in clinical neuroscience, 12(3), 271–287. https://doi.org/10.31887/DCNS.2010.12.3/ajablensky surrounding schizophrenia diagnosis, and the stigmatization of schizoid patients act as impediments to timely and proper treatment.
The best and most effective treatment for this condition includes a long-term combination 9 Patel, K. R., Cherian, J., Gohil, K., & Atkinson, D. (2014). Schizophrenia: overview and treatment options. P & T : a peer-reviewed journal for formulary management, 39(9), 638–645. of psychological interventions, medications, self-help strategies, and social support.
However, severe cases of schizophrenia heavily involve constant medical supervision and, even, hospitalization. If you or a loved one appear to suffer from the signs and symptoms of schizophrenia, it is important that you seek medical help immediately.
Read More About How Schizophrenia Can Be Treated Here
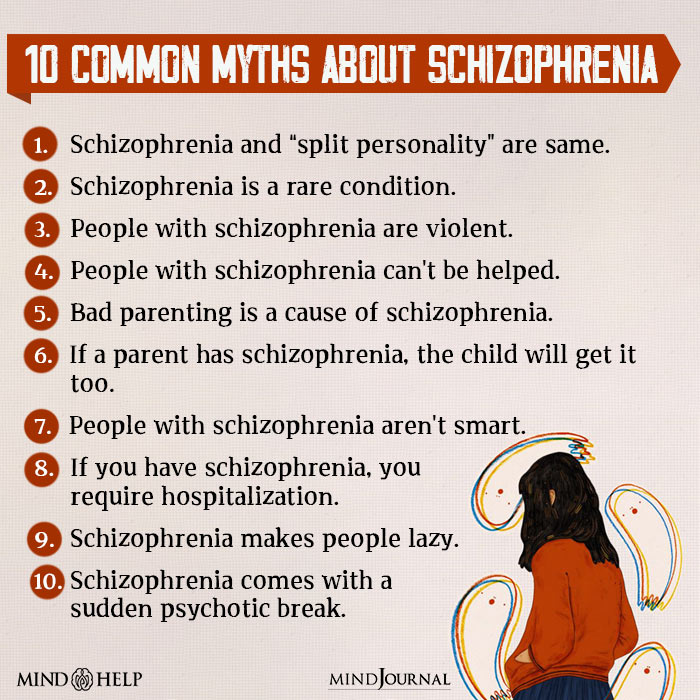
Myths About Schizophrenia
Schizophrenia is the subject of never-ending fascination, works of pop culture, and urban legends. Most schizophrenia cases have witnessed extreme media frenzy and stereotypical representations and, over the years, have accumulated a substantial body of myths and false, exaggerated notions.
Some of the most common myths 10 Fischer B. A. (2012). The unofficial myths of schizophrenia. The Journal of nervous and mental disease, 200(7), 567–568. https://doi.org/10.1097/NMD.0b013e31825bf9f7 about schizophrenia include:
1. Schizophrenia is synonymous with a “split personality” or multiple personalities.
Schizophrenia is a separate psychiatric disorder from dissociative identity disorder or multiple personality disorder.
2. Schizophrenia is a rare condition.
Schizophrenia is not a rare condition. It affects 0.32% 11 McGrath J. J. (2005). Myths and plain truths about schizophrenia epidemiology–the NAPE lecture 2004. Acta psychiatrica Scandinavica, 111(1), 4–11. https://doi.org/10.1111/j.1600-0447.2004.00467.x of the global population worldwide.
3. People with schizophrenia are dangerous.
It is a huge misconception that people with schizophrenia are violent or dangerous. They are similar to healthy people and not every schizophrenic person requires restraint or hospitalization.
4. People with schizophrenia can’t be helped.
People with schizophrenia can lead happier, healthier lives if they avail of timely treatment 12 Lin, C. H., & Lane, H. Y. (2019). Early Identification and Intervention of Schizophrenia: Insight From Hypotheses of Glutamate Dysfunction and Oxidative Stress. Frontiers in psychiatry, 10, 93. https://doi.org/10.3389/fpsyt.2019.00093 . Schizophrenia can be effectively managed by therapy, medication, and social support.
5. Bad parenting is a cause of schizophrenia.
It is a misconception that bad parenting, especially that of female guardians, is a contributing factor to schizophrenia. Children without positive parenting are at risk of their own personal troubles and behavioral problems (like depression and aggression). This results in ongoing patterns of negative behavior and mental disorders like schizophrenia.
6. If a parent has schizophrenia, the child will get it too.
Schizophrenia is heritable, via genetics and psychosocial environment. Having a parent increases the risk of developing the disorder, but it does not necessarily mean that it is a sure causal factor.
7. People with schizophrenia aren’t smart.
People use stereotypes when talking about schizophrenia. Even though this mental health condition severely impacts cognitive and behavioral functioning, it does not restrict intellect or reasoning.
8. If you have schizophrenia, you require hospitalization.
Only severe cases of schizophrenia entail hospitalization or in-patient medical treatment.
9. Schizophrenia makes people lazy.
People with schizophrenia are widely stigmatized and their professional capacities are frequently questioned. Like any other debilitating mental illness, schizophrenia has its challenges but it doesn’t make people lazy. In fact, several famous and accomplished people are living with the disorder and thriving—with proper treatment.
10. Schizophrenia comes with a sudden psychotic break.
Schizophrenia is characterized by psychotic episodes, but it is very different from brief psychotic disorder or drug-induced acute and transient psychotic states.
Takeaway
Schizophrenia is a severe lifelong condition that frequently requires long-term treatment. Although it can substantially influence the patient’s ability to function, treatment can be highly rewarding and productive. Moreover, support from friends, family members, and the community can also greatly help in recovery as well.
If you or a loved one is suffering from schizophrenia, educating yourself about the disorder, understanding available treatment options, and seeking professional help can make a lot of difference. Sustained medication and psychotherapy can enable people with schizophrenia to live a relatively normal life.
AT A Glance
- Schizophrenia is a chronic mental disorder that often causes hallucinations and delusions, leading the sufferer to experience distorted realities.
- People with schizophrenia often appear to have a disconnection from reality.
- Hallucinations and delusions are common aspects of this mental disorder.
- Patients often struggle with performing well, personally and professionally.
- Schizophrenia is a lifelong condition that may require long-term treatment.
- The most effective schizophrenia treatment includes a combination of psychological interventions, medications, and social support.
Frequently Asked Questions (FAQs)
1. Is schizophrenia genetic?
Schizophrenia tends to run in families. People with a family history of schizophrenia or mental health disorders are more vulnerable to the condition, as multiple genes are thought to be responsible for its genetic development.
2. How common is schizophrenia?
According to the World Health Organization (WHO 13 World Health Organisation. (2022). Schizophrenia. Who.int; World Health Organization: WHO. Available from: https://www.who.int/news-room/fact-sheets/detail/schizophrenia ), schizophrenia affects approximately 24 million people (i.e., 1 in 300 people or 0.32%) worldwide.
3. Is schizophrenia curable?
People with minimal or mild symptoms of schizophrenia can effectively manage their condition with psychiatric medication, therapy, and self-help strategies. However, severe cases of schizophrenia heavily involve constant medical supervision and, even, hospitalization.
4. Who are some famous people with schizophrenia?
Sportsman Lionel Aldridge, Jazz Age socialite Zelda Fitzgerald, musician Peter Green, comic artist Darrell Hammond, mathematician John Nash, artist Vincent van Gogh, and musician Skip Spence are some famous people with schizophrenia.