Paranoid schizophrenia is a debilitating psychiatric disorder that significantly impacts a person’s daily functioning, overall health, and well-being. However, with appropriate and timely treatment, individuals with this mental health condition can manage the signs of paranoid schizophrenia and improve their quality of life.
What Is Paranoid Schizophrenia?
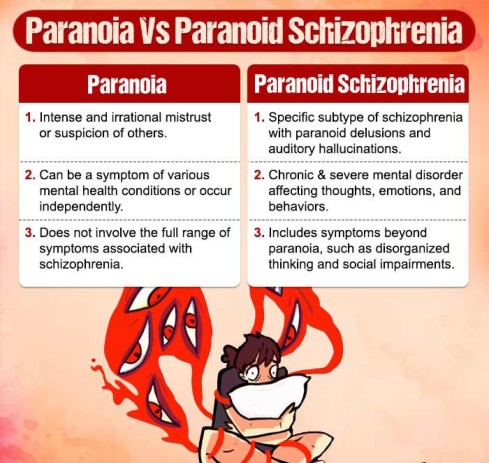
Paranoid schizophrenia is a subtype of schizophrenia, which is a chronic mental disorder characterized by a combination of symptoms that may include hallucinations, delusions, disorganized thinking or speech, emotional disturbances, and impaired social functioning.
This type of schizophrenia, along with other subtypes of schizophrenia, is recognized and classified in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) 1 Hany, M., Rehman, B., Azhar, Y., & Chapman, J. (2023). Schizophrenia. In StatPearls. StatPearls Publishing. Available from: https://www.ncbi.nlm.nih.gov/books/NBK539864/ .
What sets paranoid schizophrenia apart from other types of schizophrenia is the prominence of paranoid delusions and auditory hallucinations. Individuals with paranoid schizophrenia often have a strong belief that they are being persecuted, spied on, or conspired against by others, leading to significant mistrust and suspicion.
This form of schizophrenia is a severe one that, if left untreated, can have a negative impact on a person’s daily functioning, social relationships, as well as academic and occupational opportunities.
Prevalence Of Paranoid Schizophrenia
Globally, schizophrenia affects about 1% of the population 2 Rotshteĭn V. G. (1982). O zabolevaemosti paranoidnoĭ shizofrenieĭ [Incidence of paranoid schizophrenia]. Zhurnal nevropatologii i psikhiatrii imeni S.S. Korsakova (Moscow, Russia : 1952), 82(4), 91–98. , with paranoid schizophrenia being one of the more common subtypes.
The age of onset for paranoid schizophrenia tends to be slightly later than other subtypes, typically in late adolescence or early adulthood. However, it can also develop later in life. Gender differences exist, as paranoid schizophrenia appears to be more prevalent in males compared to females.
Case Example:
Emily Johnson, a 26-year-old student, has been experiencing suspiciousness, restlessness, negative thoughts, and anxiety for the past two years. She constantly feels observed and believes her classmates are conspiring against her, spreading rumors, and trying to harm her academically.
She holds the belief that the way others communicate with Emily is part of a plot to launch personal attacks against her. Also, when she walks alone or takes a rest at home, she hears voices that comment negatively about her appearance, abilities, and worth, leading her to isolate herself from the social world to stay safe from perceived threats.
Case Analysis:
From the present case, it can be observed that Emily has fixed, firm, false paranoid beliefs about her experiences.
She goes through anxious apprehension, experiences auditory hallucinations, and signs of persecutory delusion that led her to extreme distress and detachment from the external environment. All of her behavior indicates that Emily has significant symptoms of paranoid schizophrenia.
Read More About Schizophrenia Here
Symptoms Of Paranoid Schizophrenia
Common 3 Picchioni, M. M., & Murray, R. M. (2007). Schizophrenia. BMJ (Clinical research ed.), 335(7610), 91–95. https://doi.org/10.1136/bmj.39227.616447.BE signs of paranoid schizophrenia include:
- Delusions
- Hallucinations
- Disorganized thinking and speech
- Paranoia (or an intensely irrational feeling of distrust or suspicion of others)
- Impaired social functioning
- Emotional disturbances
- Cognitive impairments
- Lack of insight
- Catatonia
- Impaired self-care
What Causes Paranoid Schizophrenia?
The exact cause of paranoid schizophrenia is unknown, but it is believed to result from a combination of genetic, environmental, and neurochemical factors 4 Wong, V., Chin, K., & Leontieva, L. (2022). Multifactorial Causes of Paranoid Schizophrenia With Auditory-Visual Hallucinations in a 31-Year-Old Male With History of Traumatic Brain Injury and Substance Abuse. Cureus, 14(5), e25488. https://doi.org/10.7759/cureus.25488 :
- Genetic factors play a role, as individuals with a family history of schizophrenia have a higher risk of developing the condition.
- Imbalances in certain brain chemicals, including dopamine and glutamate, are thought to contribute to the development of paranoid schizophrenia.
- Environmental factors such as prenatal exposure to viruses, maternal stress during pregnancy, and complications during birth may increase the risk.
- Negative social interactions and relationships reinforce and validate paranoid thoughts and hostile behavior.
- Traumatic experiences, such as childhood abuse, neglect, or significant life stressors, can contribute to the development of paranoid schizophrenia.
- Social isolation and lack of social support can exacerbate symptoms and increase the risk of paranoid schizophrenia relapse.
- Substance abuse, particularly marijuana and stimulant drugs, can also contribute to the onset or worsening of symptoms in individuals predisposed to paranoid schizophrenia.
How Paranoid Schizophrenia Affects Mental Health
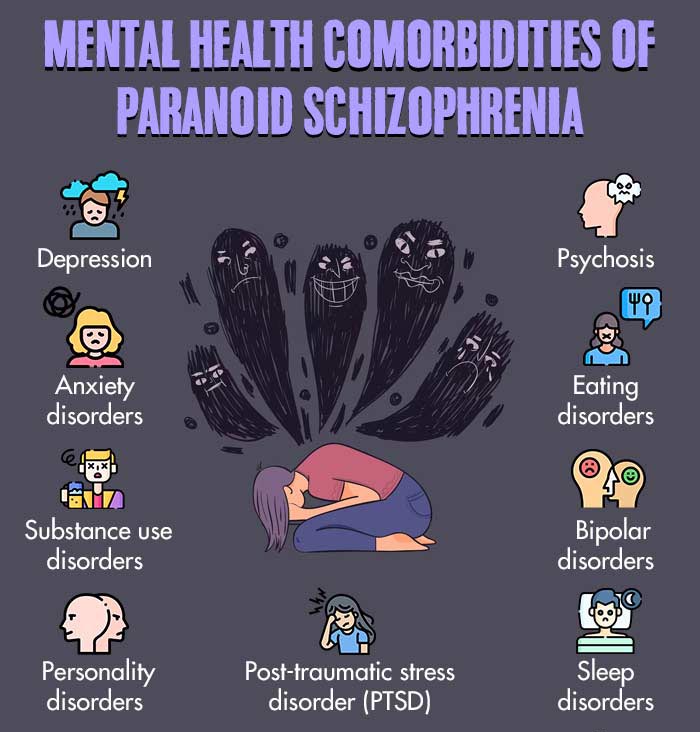
Paranoid schizophrenia has profound effects on mental health, impacting multiple aspects of an individual’s well-being.
Cognitive and perceptual disturbances disrupt thinking processes and can cause hallucinations, while emotional challenges lead to mood fluctuations and difficulties in emotional regulation. Social and occupational impairments arise from withdrawal, suspicion, and communication difficulties.
Self-care and functional limitations can pose challenges in managing daily activities and personal hygiene. The cumulative impact of these symptoms significantly affects overall well-being, leading to decreased quality of life, increased distress, and limitations in various areas of life.
Schizophrenia also enhances the risk factors for mental health disorders 5 Tcheremissine, O. V., & Englert, D. (2013). A case of paranoid schizophrenia and severe antipsychotic-induced Parkinson’s disorder treated with a combination of olanzapine and lurasidone. Innovations in clinical neuroscience, 10(9-10), 10–11. like depression, psychosis, bipolar disorders, self-harm, and suicidality.
Read More About Psychosis Here
How To Diagnose Paranoid Schizophrenia
Paranoid schizophrenia diagnosis involves a comprehensive evaluation 6 Jablensky A. (2010). The diagnostic concept of schizophrenia: its history, evolution, and future prospects. Dialogues in clinical neuroscience, 12(3), 271–287. https://doi.org/10.31887/DCNS.2010.12.3/ajablensky by a mental health professional. This includes a clinical assessment through interviews and standardized questionnaires to gather information about symptoms, medical history, and family history.
These clinical tools 7 Mortimer, A. (2007). Symptom rating scales and outcome in schizophrenia. The British Journal of Psychiatry, 191(S50), S7-S14. doi:10.1192/bjp.191.50.s7 may include Structured Clinical Interview for DSM (SCID), Positive and Negative Syndrome Scale (PANSS), Brief Psychiatric Rating Scale (BPRS), Scale for the Assessment of Positive Symptoms (SAPS), Scale for the Assessment of Negative Symptoms (SANS), etc.
The diagnostic criteria outlined in the DSM-5 are used to determine if the individual meets the specific symptoms and impaired functioning required for a diagnosis of paranoid schizophrenia.
Differential diagnosis is conducted to differentiate it from other similar conditions, and collaboration with specialists may occur to rule out any underlying medical or neurological causes. It is important to seek the expertise of a trained professional for an accurate diagnosis, as it may involve multiple assessments over time.
Treatment For Paranoid Schizophrenia
Paranoid schizophrenia treatment typically involves a combination of medication, therapy, and support 8 Patel, K. R., Cherian, J., Gohil, K., & Atkinson, D. (2014). Schizophrenia: overview and treatment options. P & T : a peer-reviewed journal for formulary management, 39(9), 638–645. . Antipsychotic medications help manage psychotic symptoms, while therapy, such as cognitive-behavioral therapy (CBT), can assist individuals in developing coping strategies and improving functioning.
Family support and psychoeducation are crucial in understanding the condition and promoting a supportive environment. Paranoid schizophrenia treatment plans are tailored to individual needs, and regular monitoring and adjustment are necessary to ensure the most effective outcomes for managing paranoid schizophrenia.
Read More About Treatment For Paranoid Schizophrenia Here
How To Cope With Paranoid Schizophrenia
Holistic approaches 9 Ganguly, P., Soliman, A., & Moustafa, A. A. (2018). Holistic Management of Schizophrenia Symptoms Using Pharmacological and Non-pharmacological Treatment. Frontiers in public health, 6, 166. https://doi.org/10.3389/fpubh.2018.00166 can be valuable in supporting individuals with paranoid schizophrenia alongside medical treatment. Psychoeducation, while maintaining a healthy lifestyle through exercise, balanced nutrition, and sufficient sleep can positively impact overall well-being.
Stress reduction techniques (such as meditation and mindfulness) help manage anxiety, and support networks provide understanding and encouragement. Engaging in creative outlets fosters self-expression and emotional well-being, while mind-body practices like acupuncture and massage therapy can offer additional support.
Read More About Coping With Paranoid Schizophrenia Here
How To Help Someone With Paranoid Schizophrenia
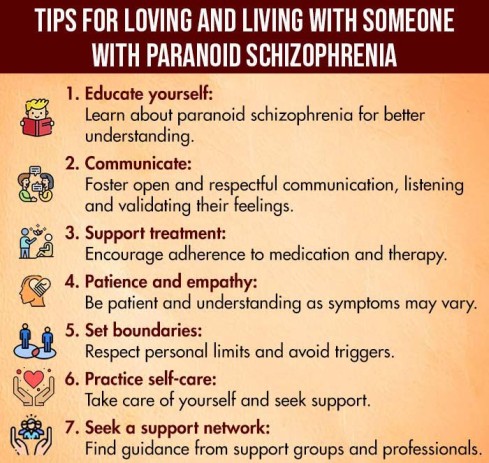
Supporting someone with paranoid schizophrenia requires understanding, empathy, and appropriate strategies 10 Mucci, A., Kawohl, W., Maria, C., & Wooller, A. (2020). Treating Schizophrenia: Open Conversations and Stronger Relationships Through Psychoeducation and Shared Decision-Making. Frontiers in psychiatry, 11, 761. https://doi.org/10.3389/fpsyt.2020.00761 . These include:
- Educate yourself to understand the condition and its symptoms.
- Communicate openly by creating a non-judgmental and safe environment.
- Encourage treatment adherence.
- Offer practical assistance with daily tasks and reduce stressors.
- Foster a supportive network.
- Respect personal boundaries and sensitivities.
Read More About Helping Someone With Paranoid Schizophrenia Here
Takeaway
The prognosis of paranoid schizophrenia can vary from person to person and is influenced by various factors. Generally, paranoid schizophrenia is a chronic condition 11 Kanahara, N., Yoshida, T., Oda, Y., Yamanaka, H., Moriyama, T., Hayashi, H., Shibuya, T., Nagaushi, Y., Sawa, T., Sekine, Y., Shimizu, E., Asano, M., & Iyo, M. (2013). Onset Pattern and Long-Term Prognosis in Schizophrenia: 10-Year Longitudinal Follow-Up Study. PloS one, 8(6), e67273. https://doi.org/10.1371/journal.pone.0067273 with a relapsing rate next to alcoholism and drug addiction. Some individuals may continue to experience residual symptoms or face occasional relapses.
Long-term prognosis can be improved with early intervention, adherence to treatment plans, a strong support system, and a comprehensive approach to managing the condition. Regular monitoring and collaboration with mental health professionals are crucial for optimizing the prognosis and providing the best possible outcomes for individuals with paranoid schizophrenia.
At A Glance
- Paranoid schizophrenia is characterized by delusions and hallucinations, primarily of control, grandeur, persecution, or reference.
- The symptoms of paranoid schizophrenia can cause severe distress and impair an individual’s ability to think clearly or communicate effectively.
- The criteria for paranoid schizophrenia diagnosis have been included in DSM-5.
- Paranoid schizophrenia affects thoughts, emotions, behaviors, actions, and relationships, significantly impacting the patient’s overall life.
- Patients may experience self-harm and suicidal ideation or behaviors, particularly when left untreated.
- Paranoid schizophrenia is a chronic psychiatric disorder with no specific cure.
- Long-term paranoid schizophrenia treatment can help patients effectively manage symptoms and enhance their quality of life.
Frequently Asked Questions (FAQs)
1. Is paranoid schizophrenia genetic?
Yes, there is evidence to suggest that genetic factors play a role in the development of paranoid schizophrenia, but it is not solely determined by genetics.
2. Can paranoid schizophrenia be cured?
There is currently no known cure for paranoid schizophrenia, but with appropriate treatment and support, individuals can manage their symptoms and lead fulfilling lives.
3. Is paranoid schizophrenia considered a disability?
Paranoid schizophrenia is generally recognized as a disabling condition that can significantly impact a person’s ability to function in various areas of life, including work, relationships, and daily activities.