Insomnia is a sleep disorder where sufferers find it difficult to fall or stay asleep and are unable to feel rested after waking up, leading to exhaustion and other serious symptoms. Left untreated, it can cause several health problems.
What Is Insomnia?
Insomnia or sleeplessness refers to chronic trouble with sleep initiation, quality, maintenance, duration or consolidation despite having a convenient & favorable environment for sleep. It is a common condition that causes severe sleep difficulties. A person with this sleep disorder may have trouble with sleep onset or falling asleep, sleep maintenance or staying asleep and getting enough or desired sleep. The sufferer may also wake up earlier than usual, find it difficult to get back to a state of sleepiness and experience ineffective, disturbed and poor quality sleep repeatedly.
As the individual is unable to get adequate sleep, they do not feel rested or rejuvenated the next day. This can result in low or depressed mood [mfn] Buysse, D. J., Angst, J., Gamma, A., Ajdacic, V., Eich, D., & Rössler, W. (2008). Prevalence, course, and comorbidity of insomnia and depression in young adults. Sleep, 31(4), 473–480. https://doi.org/10.1093/sleep/31.4.473 [/mfn] , low energy, mood disturbances, poor cognitive abilities, irritability, fatigue, poor attention and daytime sleepiness. Over time, it can cause daytime functional impairment and affect a person’s ability to perform daily tasks, work effectively & quality of life and may even cause motor vehicle accidents [mfn] Garbarino, S., Magnavita, N., Guglielmi, O., Maestri, M., Dini, G., Bersi, F. M., Toletone, A., Chiorri, C., & Durando, P. (2017). Insomnia is associated with road accidents. Further evidence from a study on truck drivers. PloS one, 12(10), e0187256. https://doi.org/10.1371/journal.pone.0187256 [/mfn] .
A 2015 study [mfn] Levenson, J. C., Kay, D. B., & Buysse, D. J. (2015). The pathophysiology of insomnia. Chest, 147(4), 1179–1192. https://doi.org/10.1378/chest.14-1617 [/mfn] explains that this sleep disorder is “characterized by chronic dissatisfaction with sleep quantity or quality that is associated with difficulty falling asleep, frequent nighttime awakenings with difficulty returning to sleep, and/or awakening earlier in the morning than desired.” However, it should be noted that insomnia is different from sleep deprivation “by difficulty sleeping despite having adequate opportunity to sleep,” adds the study. This form of sleeplessness can be acute or short-term, lasting from one or few days to few weeks, and chronic or long-term, lasting from few weeks to several months. Insomnia is primarily characterized by the following:
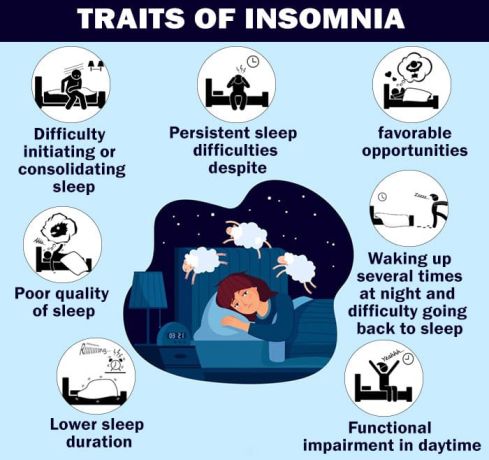
- Difficulty initiating or consolidating sleep
- Persistent sleep difficulties or trouble staying asleep despite favorable opportunities
- Poor quality and quantity of sleep
- Waking up several times at night and difficulty going back to sleep
- Waking earlier than needed, expected or desired or lower sleep duration
- Functional impairment in daytime caused by poor sleep quality
Considered to be a hyperarousal disorder experienced mostly during the day, this condition may be caused by a number of different factors such as stress, poor lifestyle and sleeping habits, diseases, mental health disorders, medications etc. However, with early diagnosis and effective treatment one can overcome this condition.
Prevalence Of Insomnia
Insomnia has a high prevalence and affects a large volume of the global population “on a situational, recurrent or chronic basis and is among the most common complaints in medical practice,” according to researchers [mfn] Morin, C. M., Drake, C. L., Harvey, A. G., Krystal, A. D., Manber, R., Riemann, D., & Spiegelhalder, K. (2015). Insomnia disorder. Nature reviews. Disease primers, 1, 15026. https://doi.org/10.1038/nrdp.2015.26 [/mfn] . Different studies [mfn] Bhaskar, S., Hemavathy, D., & Prasad, S. (2016). Prevalence of chronic insomnia in adult patients and its correlation with medical comorbidities. Journal of family medicine and primary care, 5(4), 780–784. https://doi.org/10.4103/2249-4863.201153 [/mfn] have found that prevalence is around 10% to 30% of the population worldwide, however some other studies have found that the prevalence can be around 50% to 60% as well. Moreover, chronic insomnia is observed in about 33% of adults. The researchers also found that the sleep disorder is common in women, individuals with mental health issues and those who are medically ill. Moreover, it is also closely associated with increasing age as well as diabetes.
Understanding Insomnia
Insomnia is a person’s self-perception [mfn] Harvey, A. G., & Tang, N. K. (2012). (Mis)perception of sleep in insomnia: a puzzle and a resolution. Psychological bulletin, 138(1), 77–101. https://doi.org/10.1037/a0025730 [/mfn] and report of sleep impairment and chronic difficulty with initiating & maintaining sleep, having repeated non-restorative sleep or waking up before scheduled time despite favorable opportunities. It “is a highly prevalent, often debilitating, and economically burdensome form of sleep disturbance caused by various situational, medical, emotional, environmental and behavioral factors,” states a 2004 research paper [mfn] Edinger, J. D., Bonnet, M. H., Bootzin, R. R., Doghramji, K., Dorsey, C. M., Espie, C. A., Jamieson, A. O., McCall, W. V., Morin, C. M., Stepanski, E. J., & American Academy of Sleep Medicine Work Group (2004). Derivation of research diagnostic criteria for insomnia: report of an American Academy of Sleep Medicine Work Group. Sleep, 27(8), 1567–1596. https://doi.org/10.1093/sleep/27.8.1567 [/mfn].
People suffering from this condition often try hard to sleep and struggle repeatedly to get some much needed sleep, which can make the process of falling asleep even more challenging regardless of their level of tiredness. Other sufferers may wake up a short while after falling asleep and may not be able to get any sleep for the rest of the night. This can directly lead to emotional stress and anxiety [mfn] Choueiry, N., Salamoun, T., Jabbour, H., El Osta, N., Hajj, A., & Rabbaa Khabbaz, L. (2016). Insomnia and Relationship with Anxiety in University Students: A Cross-Sectional Designed Study. PloS one, 11(2), e0149643. https://doi.org/10.1371/journal.pone.0149643 [/mfn] .
Conversely, high levels of stress [mfn] Kim, E. J., & Dimsdale, J. E. (2007). The effect of psychosocial stress on sleep: a review of polysomnographic evidence. Behavioral sleep medicine, 5(4), 256–278. https://doi.org/10.1080/15402000701557383 [/mfn] and an inability to relax may also play a role in the onset of sleeplessness. However, as each of us are unique, we may have different requirements when it comes to sleep, even though 7 to 9 hours of sleep every day is the standard acceptable amount of sleep for healthy functioning. Regardless, insomnia is concerned about the quality of sleep rather than the quantity. It is about how a person feels after waking up and whether they feel restored and energized instead of fatigued and depressed.
According to researchers, to be considered insomnia, a person must experience sleep difficulties for a minimum of three nights a week for over three months. Considered as a sleep disorder, it can often occur with various comorbid or co-occurring conditions, such as different psychiatric disorders [mfn] Benca, R. M., Obermeyer, W. H., Thisted, R. A., & Gillin, J. C. (1992). Sleep and psychiatric disorders. A meta-analysis. Archives of general psychiatry, 49(8), 651–670. https://doi.org/10.1001/archpsyc.1992.01820080059010 [/mfn] and medical disorders [mfn] Smith, M. T., Huang, M. I., & Manber, R. (2005). Cognitive behavior therapy for chronic insomnia occurring within the context of medical and psychiatric disorders. Clinical psychology review, 25(5), 559–592. https://doi.org/10.1016/j.cpr.2005.04.004 [/mfn] . Research [mfn] Taylor, D. J., Mallory, L. J., Lichstein, K. L., Durrence, H. H., Riedel, B. W., & Bush, A. J. (2007). Comorbidity of chronic insomnia with medical problems Sleep, 30(2), 213–218. https://doi.org/10.1093/sleep/30.2.213 [/mfn] shows that this disorder can have significant comorbidity with multiple medical and psychiatric problems [mfn] Ohayon M. M. (2002). Epidemiology of insomnia: what we know and what we still need to learn. Sleep medicine reviews, 6(2), 97–111. https://doi.org/10.1053/smrv.2002.0186 [/mfn] .
Further studies [mfn] Morin, C. M., Drake, C. L., Harvey, A. G., Krystal, A. D., Manber, R., Riemann, D., & Spiegelhalder, K. (2015). Insomnia disorder. Nature reviews. Disease primers, 1, 15026. https://doi.org/10.1038/nrdp.2015.26 [/mfn] have found that chronic sleeplessness is significantly associated with long-term, adverse health outcomes, psychological & physical morbidity and decreased quality of life. It can significantly contribute to the development of depression [mfn] Nutt, D., Wilson, S., & Paterson, L. (2008). Sleep disorders as core symptoms of depression. Dialogues in clinical neuroscience, 10(3), 329–336. https://doi.org/10.31887/DCNS.2008.10.3/dnutt [/mfn] , substance abuse [mfn] Rosenblum M. (2017). Substance abuse and insomnia. Minnesota medicine, 100(3), 38–39. [/mfn] , cardiovascular disease [mfn] Javaheri, S., & Redline, S. (2017). Insomnia and Risk of Cardiovascular Disease. Chest, 152(2), 435–444. https://doi.org/10.1016/j.chest.2017.01.026 [/mfn] , diabetes [mfn] Khandelwal, D., Dutta, D., Chittawar, S., & Kalra, S. (2017). Sleep Disorders in Type 2 Diabetes. Indian journal of endocrinology and metabolism, 21(5), 758–761. https://doi.org/10.4103/ijem.IJEM_156_17 [/mfn] and even obesity [mfn] Ding, C., Lim, L. L., Xu, L., & Kong, A. (2018). Sleep and Obesity. Journal of obesity & metabolic syndrome, 27(1), 4–24. https://doi.org/10.7570/jomes.2018.27.1.4 [/mfn] or weight gain [mfn] Cai, G. H., Theorell-Haglöw, J., Janson, C., Svartengren, M., Elmståhl, S., Lind, L., & Lindberg, E. (2018). Insomnia symptoms and sleep duration and their combined effects in relation to associations with obesity and central obesity. Sleep medicine, 46, 81–87. https://doi.org/10.1016/j.sleep.2018.03.009 [/mfn] . By seeking medical help and treating any underlying conditions one can recover from this sleeplessness disorder.
Symptoms Of Insomnia
A person suffering from insomnia may experience the following common symptoms –
- Trouble falling asleep at night
- Waking up too early
- Waking up frequently during sleep
- Impaired daytime functioning
- Inability to feel rested after sleep
- Daytime sleepiness
- Fatigue & exhaustion
- Lack of concentration & poor attention
- Low motivation and lack of energy
- Mood swings
- Constantly worried about sleep
- Poor cognitive functioning
- Impulsiveness, hyperactivity & other behavioral issues
- Malaise
- Grumpiness, irritability & aggression
- Lack of coordination & increased likelihood of accidents or mistakes
- Chronic pain, headache or stomach problems
- Memory problems
- Stress, anxiety & depression
- Social withdrawal
- Repeated use of alcohol or sleeping aids
Moreover, chronic insomnia can also affect executive functions, decision making abilities, social interactions [mfn] Roth T. (2007). Insomnia: definition, prevalence, etiology, and consequences. Journal of clinical sleep medicine : JCSM : official publication of the American Academy of Sleep Medicine, 3(5 Suppl), S7–S10. [/mfn] , personal relationships etc. In fact, it can even cause suicidal thoughts [mfn] Chu, C., Hom, M. A., Rogers, M. L., Stanley, I. H., Ringer-Moberg, F. B., Podlogar, M. C., Hirsch, J. K., & Joiner, T. E. (2017). Insomnia and suicide-related behaviors: A multi-study investigation of thwarted belongingness as a distinct explanatory factor. Journal of affective disorders, 208, 153–162. https://doi.org/10.1016/j.jad.2016.08.065 [/mfn] and ideations. “Insomnia has been established as a risk factor for depression and mental illness for decades, but a growing body of evidence has recently exposed insomnia to be an independent risk factor for suicide that encompasses all age ranges,” states a 2013 study [mfn] McCall, W. V., & Black, C. G. (2013). The link between suicide and insomnia: theoretical mechanisms. Current psychiatry reports, 15(9), 389. https://doi.org/10.1007/s11920-013-0389-9 [/mfn] .
Types Of Insomnia
This sleep disorder can be categorized by duration into acute and chronic insomnia. Acute or transient insomnia is primarily short-term [mfn] Momin RR, Ketvertis K. Short Term Insomnia. [Updated 2020 Sep 22]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK554516/ [/mfn] and the problem can come and go. The symptoms are experienced for a brief period and tend to last for a few days or weeks. It is typically caused by stress [mfn] Kalmbach, D. A., Anderson, J. R., & Drake, C. L. (2018). The impact of stress on sleep: Pathogenic sleep reactivity as a vulnerability to insomnia and circadian disorders. Journal of sleep research, 27(6), e12710. https://doi.org/10.1111/jsr.12710 [/mfn] . Chronic insomnia can cause long standing problems [mfn] Kaur H, Spurling BC, Bollu PC. Chronic Insomnia. [Updated 2020 Nov 19]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK526136/ [/mfn] and can last for months or even years. In this form of sleeplessness, sleep difficulties are experienced at least three times a week for about three months or more.
However, the condition can also be classified based on severity, namely –
1. Mild
The symptoms experienced are typically mild and include lack of sleep causing fatigue and tiredness after waking up.
2. Moderate
The symptoms can be more impactful and may lead to impairment of daily functioning.
3. Severe
The sufferer experiences serious symptoms on a daily basis which adversely affects different aspects of their life.
However, most medical professionals categorize the disorder [mfn] Lichstein, K. L., Durrence, H. H., Bayen, U. J., & Riedel, B. W. (2001). Primary versus secondary insomnia in older adults: subjective sleep and daytime functioning. Psychology and aging, 16(2), 264–271. https://doi.org/10.1037//0882-7974.16.2.264 [/mfn] based on the causes. These types are as follow:
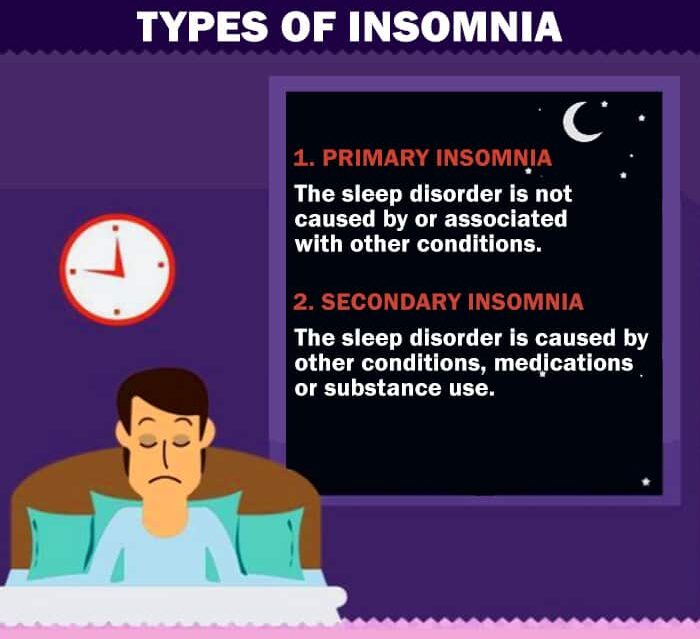
A. Primary insomnia
In this classification, the sleep disorder is a problem in itself. The symptoms or sleep difficulties are not caused by or associated with other underlying medical or psychological health issues or conditions.
B. Secondary insomnia
This variant of this disorder is caused by other underlying health problems or disorders. Hence, the symptoms and sleeping problems are linked with certain physical or psychiatric conditions, health problems, medications or even substance use.
Causes Of Insomnia
Sleeplessness may be caused by a wide range of factors that may influence the onset of varying levels of sleep problems. Some of the most common contributing factors may include the following:
1. Genetics
Twin and family studies [mfn] Lind, M. J., & Gehrman, P. R. (2016). Genetic Pathways to Insomnia. Brain sciences, 6(4), 64. https://doi.org/10.3390/brainsci6040064 [/mfn] have shown this sleep disorder “is moderately heritable.” It means the condition can run in families [mfn] Gehrman, P. R., Pfeiffenberger, C., & Byrne, E. (2013). The Role of Genes in the Insomnia Phenotype. Sleep medicine clinics, 8(3), 323–331. https://doi.org/10.1016/j.jsmc.2013.04.005 [/mfn] . So if someone has a first-degree relative with a sleep disorder or insomnia, then that person can also develop the condition due to genetic predisposition [mfn] Lane, J. M., Jones, S. E., Dashti, H. S., Wood, A. R., Aragam, K. G., van Hees, V. T., Strand, L. B., Winsvold, B. S., Wang, H., Bowden, J., Song, Y., Patel, K., Anderson, S. G., Beaumont, R. N., Bechtold, D. A., Cade, B. E., Haas, M., Kathiresan, S., Little, M. A., Luik, A. I., … Saxena, R. (2019). Biological and clinical insights from genetics of insomnia symptoms. Nature genetics, 51(3), 387–393. https://doi.org/10.1038/s41588-019-0361-7 [/mfn] .
2. Stress, anxiety and depression
It has been observed that being overly stressed [mfn] Basta, M., Chrousos, G. P., Vela-Bueno, A., & Vgontzas, A. N. (2007). CHRONIC INSOMNIA AND STRESS SYSTEM. Sleep medicine clinics, 2(2), 279–291. https://doi.org/10.1016/j.jsmc.2007.04.002 [/mfn] or worrying excessively can cause sleep disorders by keeping the mind active. In fact, this condition is closely associated with certain psychological and emotional factors like anxiety, depressed mood [mfn] Drake, C. L., Pillai, V., & Roth, T. (2014). Stress and sleep reactivity: a prospective investigation of the stress-diathesis model of insomnia. Sleep, 37(8), 1295–1304. https://doi.org/10.5665/sleep.3916 [/mfn] , grief, trauma [mfn] Han, K. S., Kim, L., & Shim, I. (2012). Stress and sleep disorder. Experimental neurobiology, 21(4), 141–150. https://doi.org/10.5607/en.2012.21.4.141 [/mfn] and anger. It can often have a bi-directional relationship as sleep difficulties can also lead to high levels of stress, anxiety and depression. “Greater sleep difficulty following a challenging event, or a vulnerability to stress-related sleep disturbance (i.e., sleep reactivity), is characteristic of insomnia,” explains a study [mfn] Vargas, I., Friedman, N. P., & Drake, C. L. (2015). Vulnerability to Stress-Related Sleep Disturbance and Insomnia: Investigating the Link with Comorbid Depressive Symptoms. Translational issues in psychological science, 1(1), 57–66. https://doi.org/10.1037/tps0000015 [/mfn] .
Read More About Depression Here.
3. Health conditions or illness
Sleeplessness can be caused by various medical problems & diseases [mfn] Saddichha S. (2010). Diagnosis and treatment of chronic insomnia. Annals of Indian Academy of Neurology, 13(2), 94–102. https://doi.org/10.4103/0972-2327.64628 [/mfn] , such as Parkinson’s disease, degenerative neurological disorders, chronic pain [mfn] Keilani, M., Crevenna, R., & Dorner, T. E. (2018). Sleep quality in subjects suffering from chronic pain. Wiener klinische Wochenschrift, 130(1-2), 31–36. https://doi.org/10.1007/s00508-017-1256-1 [/mfn] , prostate hypertrophy, cancer, heart failure, kidney disease, hyperthyroidism, asthma, renal disorders, acid reflux, rhinitis and allergies.
4. Medications
Different types of prescription medications can often cause certain side effects associated with sleep impairments. Medications such as cold and flu medications, high blood pressure drugs, antidepressants [mfn] Wichniak, A., Wierzbicka, A., Walęcka, M., & Jernajczyk, W. (2017). Effects of Antidepressants on Sleep. Current psychiatry reports, 19(9), 63. https://doi.org/10.1007/s11920-017-0816-4 [/mfn] , thyroid hormone, ADHD stimulants and even contraceptives can cause sleeplessness.
5. Sleep disorders
Even though insomnia itself is considered as a sleep disorder [mfn] Karna B, Gupta V. Sleep Disorder. [Updated 2021 Feb 6]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK560720/ [/mfn] , it can often be influenced by the presence of other sleep disorders. Hence, it can be a symptom of sleep conditions such as restless leg syndrome, circadian rhythm disturbances, jet lag or sleep apnea. It can also be associated with night shift work.
Apart from these, there may be some other risk factors that can lead to this sleep condition, such as:
- Poor sleeping habits & sedentary, unhealthy lifestyle
- Lack of physical exercise
- Sleeping during the day
- Life stressors such as work pressure, family responsibilities, financial problems etc
- Environmental factors like loud sound, strong lights or uncomfortable temperature
- Use of technology or gadgets in the bedroom or before bedtime
- Specific nighttime responsibilities, such as caregiving
- Travel or shift work causing jet lag
- Substance abuse or smoking & drinking close to bedtime
- Consuming too much food late in the evening
- Nightmares, bad dreams or night terrors
- Aging or older age
- Gender (40% increased risk [mfn] Mallampalli, M. P., & Carter, C. L. (2014). Exploring sex and gender differences in sleep health: a Society for Women’s Health Research Report. Journal of women’s health (2002), 23(7), 553–562. https://doi.org/10.1089/jwh.2014.4816 [/mfn] of onset for women)
- Mental health and psychiatric conditions
- Pregnancy
- Vitamin deficiency [mfn] Gao, Q., Kou, T., Zhuang, B., Ren, Y., Dong, X., & Wang, Q. (2018). The Association between Vitamin D Deficiency and Sleep Disorders: A Systematic Review and Meta-Analysis. Nutrients, 10(10), 1395. https://doi.org/10.3390/nu10101395 [/mfn]
- Hormone fluctuations caused by menopause, menstruation etc
Diagnosis Of Insomnia
There is no particular test for diagnosing this sleep disorder. A doctor or a healthcare professional like a psychiatrist or psychologist may ask certain questions about the patient’s medical history and family history. The patient may also be asked to maintain a sleep log to better understand the symptoms. However, the doctor may conduct a few physical exams like a blood test to rule out other underlying causes. The doctor may review the patient’s sleep history by performing some other tests such as –
- Sleep diary
- Sleep-wake actigraphy
- Multiple Sleep Latency Test (MSLT [mfn] Arand, D. L., & Bonnet, M. H. (2019). The multiple sleep latency test. Handbook of clinical neurology, 160, 393–403. https://doi.org/10.1016/B978-0-444-64032-1.00026-6 [/mfn] )
- Sleep study or Polysomnography [mfn] Rundo, J. V., & Downey, R., 3rd (2019). Polysomnography. Handbook of clinical neurology, 160, 381–392. https://doi.org/10.1016/B978-0-444-64032-1.00025-4 [/mfn]
The doctor may also ask if the patient has any existing medical conditions and if they take any medications which may adversely affect their sleep.
Treatment Of Insomnia

Treatment typically depends on the cause and intensity of the condition. In case of acute insomnia, medical treatment may not be necessary as the symptoms may improve naturally over time. In case the sleep disorder is caused by a specific environmental factor, then changing the environment and practicing better sleep habits and sleep hygiene can have a significant positive impact. However, for chronic insomnia seeking medical support may be necessary.
A doctor may suggest medications or behavioral therapy approaches or a combination of both for recovery depending on the patient and other factors like causes and risk factors. According to researchers, pharmacologic and nonpharmacologic or behavioral interventions and therapies can help to treat insomnia effectively. “Nonpharmacologic therapies include sleep hygiene, cognitive behavior therapy, relaxation therapy, multicomponent therapy, and paradoxical intention,” add the researchers.
In case the sleep disorder is caused by an underlying medical or psychiatric disorder, then it is crucial that treatment is targeted at the comorbid condition(s) along with specific treatment for sleep problems. Treatment of insomnia may require some patience, determination, trial and error and co-ordination between the doctor and the patient. By cooperating with the doctor, the sufferer can help them to devise the most effective treatment plan for their specific condition and symptoms. “Regardless of the type of therapy used, the treatment of chronic insomnia has two primary objectives: improving sleep quality and quantity, and improving daytime impairments,” states a 2015 study [mfn] Lie, J. D., Tu, K. N., Shen, D. D., & Wong, B. M. (2015). Pharmacological Treatment of Insomnia. P & T : a peer-reviewed journal for formulary management, 40(11), 759–771. [/mfn] .
Some of the most common and recommended treatment approaches for chronic insomnia include –
1. Pharmaceutical treatment
“Medications, in general, can be safely utilized on a short-term basis for the treatment of transient insomnia,” explains a 2001 study [mfn] Pagel, J. F., & Parnes, B. L. (2001). Medications for the Treatment of Sleep Disorders: An Overview. Primary care companion to the Journal of clinical psychiatry, 3(3), 118–125. https://doi.org/10.4088/pcc.v03n0303 [/mfn] . A doctor may prescribe certain sleeping aids and pills to help the patient sleep better. However, medications, such as sleeping pills, benzodiazepine [mfn] Solomon, F., White, C. C., Parron, D. L., & Mendelson, W. B. (1979). Sleeping pills, insomnia and medical practice. The New England journal of medicine, 300(14), 803–808. https://doi.org/10.1056/NEJM197904053001423 [/mfn] and non-benzodiazepine drugs, are mostly prescribed for short-term use as these can have severe adverse effects in the long run. These are not the preferred or recommended treatment for this condition.
2. Non-pharmaceutical treatment
Behavioral interventions and non-pharmacologic or non-pharmaceutical treatment approaches typically involve the following:
- Psychotherapy or counseling
- Cognitive behavioral therapy (CBT)
- Hypnosis
- Melatonin
Psychotherapies such as insomnia-specific cognitive behavioral therapy (CBTi [mfn] Jansson-Fröjmark, M., & Norell-Clarke, A. (2016). Cognitive Behavioural Therapy for Insomnia in Psychiatric Disorders. Current sleep medicine reports, 2(4), 233–240. https://doi.org/10.1007/s40675-016-0055-y [/mfn] ) have been identified as the first-line of treatment [mfn] Anderson K. N. (2018). Insomnia and cognitive behavioural therapy-how to assess your patient and why it should be a standard part of care. Journal of thoracic disease, 10(Suppl 1), S94–S102. https://doi.org/10.21037/jtd.2018.01.35 [/mfn] for this sleep disorder. CBTi helps the sufferer to identify negative thought and behavior patterns and replace them with positive ones to promote sound sleep. Studies have found that cognitive behavioral treatment of insomnia (CBTi) focuses on improving cognitions, behaviors and other associated factors that cause the disorder.
CBTi is effective for different types of people, even individuals with psychiatric and medical comorbidities. This therapy [mfn] Haynes, J., Talbert, M., Fox, S., & Close, E. (2018). Cognitive Behavioral Therapy in the Treatment of Insomnia. Southern medical journal, 111(2), 75–80. https://doi.org/10.14423/SMJ.0000000000000769 [/mfn] involves stimulus control, sleep hygiene, relaxation training, cognitive therapy and sleep restriction that helps to manage the symptoms. “CBT-I is effective for treating insomnia when compared with medications, and its effects may be more durable than medications.” explains a 2012 study [mfn] Mitchell, M. D., Gehrman, P., Perlis, M., & Umscheid, C. A. (2012). Comparative effectiveness of cognitive behavioral therapy for insomnia: a systematic review. BMC family practice, 13, 40. https://doi.org/10.1186/1471-2296-13-40 [/mfn] . Cognitive behavioral therapy can also be effective in overcoming underlying causes and comorbidities.
Hypnotherapy [mfn] Lam, T. H., Chung, K. F., Yeung, W. F., Yu, B. Y., Yung, K. P., & Ng, T. H. (2015). Hypnotherapy for insomnia: a systematic review and meta-analysis of randomized controlled trials. Complementary therapies in medicine, 23(5), 719–732. https://doi.org/10.1016/j.ctim.2015.07.011 [/mfn] can also be helpful in treating this condition. Research [mfn] Chamine, I., Atchley, R., & Oken, B. S. (2018). Hypnosis Intervention Effects on Sleep Outcomes: A Systematic Review. Journal of clinical sleep medicine : JCSM : official publication of the American Academy of Sleep Medicine, 14(2), 271–283. https://doi.org/10.5664/jcsm.6952 [/mfn] shows that hypnosis [mfn] Paterson D. C. (1982). Hypnosis: an alternate approach to insomnia. Canadian family physician Medecin de famille canadien, 28, 768–770. [/mfn] can help to reduce the adverse effects of sleep disorders and help to manage symptoms in both primary or secondary insomnia. Although melatonin can be suggested to help the recovery process, there is no clear evidence for its effectiveness.
In general, melatonin [mfn] Ferracioli-Oda, E., Qawasmi, A., & Bloch, M. H. (2013). Meta-analysis: melatonin for the treatment of primary sleep disorders. PloS one, 8(5), e63773. https://doi.org/10.1371/journal.pone.0063773 [/mfn] can help to improve sleep in people with sleep disorders compared to placebo. However, “No evidence-based guidelines or evidence regarding the cost-effectiveness of melatonin for the treatment of insomnia were identified,” explains a study [mfn] Gray C, Ryce A. Melatonin for the Treatment of Insomnia: A Review of Clinical Effectiveness, Cost-Effectiveness, and Guidelines [Internet]. Ottawa (ON): Canadian Agency for Drugs and Technologies in Health; 2019 Feb 22. Available from: https://www.ncbi.nlm.nih.gov/books/NBK544670/ [/mfn] . Regardless, following the treatment plan and attending therapy sessions regularly can ensure that the patient recovers successfully.
Read More About Cognitive Behavioral Therapy Here.
Self-help And Coping Strategies
Apart from medications and therapies, certain lifestyle changes and self-help techniques can also prove to be beneficial. Some effective coping strategies can include the following:
- Develop good sleeping habits
- Practice better sleep hygiene
- Create a calm and comfortable environment in the bedroom
- Go to sleep at the same time daily and have a consistent sleep-wake time
- Follow relaxing rituals before bedtime, like reading books, taking a warm bath, listening to soothing music
- Use essential oils and aromatherapy to promote better sleep
- Stay active during the day and exercise regularly
- Practice relaxation techniques like deep breathing, meditation [mfn] Black, D. S., O’Reilly, G. A., Olmstead, R., Breen, E. C., & Irwin, M. R. (2015). Mindfulness meditation and improvement in sleep quality and daytime impairment among older adults with sleep disturbances. JAMA Internal Medicine, 175(4), 494. https://doi.org/10.1001/jamainternmed.2014.8081 [/mfn] , yoga etc
- Use your bed only for resting, sleeping and sexual activities
- Practice progressive muscle relaxation
- Don’t force yourself to sleep. Get up, relax and calm your mind if you’re not sleepy.
- Avoid eating heavy meals & beverages late in the evening or before bedtime
- Restrict or avoid daytime naps
- Avoid or restrict the use of nicotine, caffeine and alcohol
- Avoid physical exercise close to bedtime
- Avoid using technology, such as a smartphone, laptop, e-book reader or tablet before bedtime
- Consult your doctor to know if any of your existing medications may cause insomnia
It should be noted that these self-help tips can only help in the recovery process when you are seeking proper medical care for your sleep disorder and other comorbid conditions. Coping strategies should never be considered as substitutes for medical treatment.
Recovery From Insomnia
Insomnia is a widely prevalent sleep disorder that affects millions of people worldwide. When left untreated, it can not only affect your mental and physical health but also significantly impair your daily functioning and quality of life. This is why it is important to consult a doctor and follow the prescribed and recommended treatment for complete recovery.
Insomnia At A Glance
- Insomnia is a sleep disorder where sufferers find it difficult to fall or stay asleep and are unable to feel rested after waking up.
- Chronic insomnia is observed in about 33% of adults.
- People suffering from this condition often try hard to sleep and struggle repeatedly to get some much needed sleep.
- Insomnia is common in women, individuals with mental health issues and those who are medically ill.
- Pharmacologic and nonpharmacologic or behavioral interventions and therapies can help to treat insomnia effectively.






Leave a Reply