Ever notice how your mood seems to crash at night? Depression at night is more common than you might think. Why do those heavy feelings show up just when you’re trying to rest? And how does it mess with your sleep, creating a cycle that’s hard to break? Read on to find out!
What is Depression at Night?
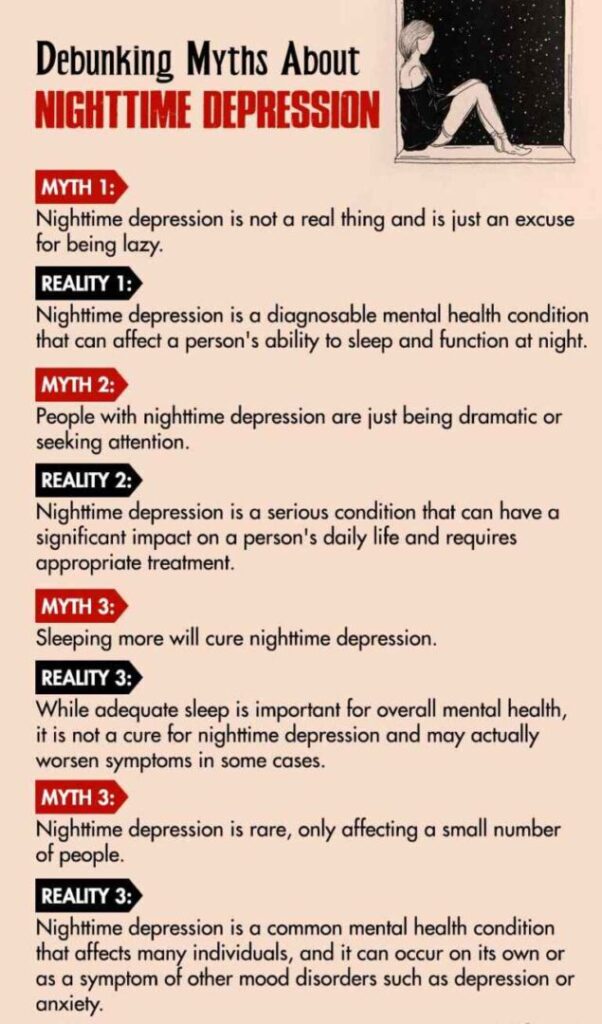
Nighttime depression is a type of depression that feels worse in the evening or at night. You might feel deep sadness, hopelessness, or emotional heaviness when the day ends, making it harder to cope or wind down.
This can make it difficult for some individuals to fall or stay asleep, intensifying their depression and leading to feelings of fatigue, irritability, and difficulty concentrating during the day.
Several factors may contribute to nighttime depression, including changes in circadian rhythms, hormonal imbalances, and an increase in negative thoughts and emotions that tend to arise at night. As a result, nighttime depression can significantly impact daily functioning and quality of life.
Read More About Depression Here
Case Example
Richard, a software engineer from a small town, had dreams of moving to the big city for better career opportunities. But after his father passed away suddenly, he stayed back to support his family and keep his current job.
He took on more projects and worked harder; but, at the end of the day, particularly near bedtime, he felt sleepless and irritable—provoked by ruminating thoughts of his unfulfilled dreams.
Throughout the day, no negative thought haunted him. However, as soon as night came and he tried to sleep, the same worries plagued him. He spent many sleepless nights and this began impacting his well-being in daily life.
Case Analysis
It is evident from the present case that Richard displays signs of insomnia, low mood, poor appetite, negative and distorted thoughts, and feelings of hopelessness at night, particularly before bedtime. This is a clear indication that he suffers from nighttime depression.
Nighttime Depression Symptoms
Depression at night is characterized by persistent feelings of sadness or a loss of interest. According to DSM-5 1 Substance Abuse and Mental Health Services Administration. (2016). Table 9, DSM-IV to DSM-5 Major Depressive Episode/Disorder Comparison. Nih.gov; Substance Abuse and Mental Health Services Administration (US). Available from: https://www.ncbi.nlm.nih.gov/books/NBK519712/table/ch3.t5/ , these depressive symptoms must last for at least two weeks to qualify for a medical diagnosis.
However, other symptoms 2 McCarter T. (2008). Depression overview. American health & drug benefits, 1(3), 44–51. can also be present during nighttime depression, which may include:
- Insomnia 3 Roth T. (2007). Insomnia: definition, prevalence, etiology, and consequences. Journal of clinical sleep medicine : JCSM : official publication of the American Academy of Sleep Medicine, 3(5 Suppl), S7–S10. or hypersomnia
- Significant weight loss or gain
- Changes in appetite
- Irritability
- Fatigue
- Worthlessness 4 Harrison, P., Lawrence, A. J., Wang, S., Liu, S., Xie, G., Yang, X., & Zahn, R. (2022). The Psychopathology of Worthlessness in Depression. Frontiers in psychiatry, 13, 818542. https://doi.org/10.3389/fpsyt.2022.818542
- Excessive guilt
- Hopelessness 5 Liu, R. T., Kleiman, E. M., Nestor, B. A., & Cheek, S. M. (2015). The Hopelessness Theory of Depression: A Quarter Century in Review. Clinical psychology : a publication of the Division of Clinical Psychology of the American Psychological Association, 22(4), 345–365. https://doi.org/10.1111/cpsp.12125
- Helplessness 6 Nuvvula S. (2016). Learned helplessness. Contemporary clinical dentistry, 7(4), 426–427. https://doi.org/10.4103/0976-237X.194124
- Indecisiveness
- Suicidal ideation 7 Harmer, B., Lee, S., Duong, T. vi H., & Saadabadi, A. (2021). Suicidal Ideation. PubMed; StatPearls Publishing. Available from: https://www.ncbi.nlm.nih.gov/books/NBK565877/
- Persistent body aches, such as back pain and headache
Read More About Insomnia Here
What Causes Depression at Night?
Here are several potential factors 8 Council, R., Mary Jane England, & Sim, L. J. (2019). The Etiology of Depression. Nih.gov; National Academies Press (US). Available from: https://www.ncbi.nlm.nih.gov/books/NBK215119/ that may contribute to depression at night:
1. Heredity
A family history of depression may increase the likelihood 9 Shadrina, M., Bondarenko, E. A., & Slominsky, P. A. (2018). Genetics Factors in Major Depression Disease. Frontiers in psychiatry, 9, 334. https://doi.org/10.3389/fpsyt.2018.00334 of experiencing depression at night.
2. Hormonal Imbalances
Hormones that regulate mood, such as melatonin and serotonin 10 Nautiyal, K. M., & Hen, R. (2017). Serotonin receptors in depression: from A to B. F1000Research, 6, 123. https://doi.org/10.12688/f1000research.9736.1 , can become imbalanced due to disruptions in circadian rhythm, exposure to artificial light, or other factors, contributing to depression at night.
3. Disruption in Circadian Rhythm
Irregular sleep patterns or nighttime shift work can disrupt circadian rhythms 11 Reddy, S., Reddy, V., & Sharma, S. (2020). Physiology, Circadian Rhythm. PubMed; StatPearls Publishing. Available from: https://www.ncbi.nlm.nih.gov/books/NBK519507/#:~:text=Circadian%20rhythm%20is%20the%2024 , leading to depression and other mood disorders.
4. Excessive Rumination
During the night, people may have more time 12 Armstead, E. A., Votta, C. M., & Deldin, P. J. (2019). Examining rumination and sleep: A transdiagnostic approach to depression and social anxiety. Neurology, Psychiatry and Brain Research, 32, 99–103. https://doi.org/10.1016/j.npbr.2019.05.003 to dwell on negative thoughts and emotions, which can contribute to depression.
5. Lifestyle Factors
Poor sleep hygiene, such as consuming caffeine 13 Clark, I., & Landolt, H. P. (2017). Coffee, caffeine, and sleep: A systematic review of epidemiological studies and randomized controlled trials. Sleep medicine reviews, 31, 70–78. https://doi.org/10.1016/j.smrv.2016.01.006 close to bedtime, can disrupt sleep and contribute to depression at night. Additionally, lack of exercise, poor nutrition, and social isolation can also contribute 14 Cui, N., Cui, J., Xu, X., Aslam, B., Bai, L., Li, D., Wu, D., Ma, Z., Sun, J., & Baloch, Z. (2021). Health Conditions, Lifestyle Factors and Depression in Adults in Qingdao, China: A Cross-Sectional Study. Frontiers in psychiatry, 12, 508810. https://doi.org/10.3389/fpsyt.2021.508810 to depression and other mood disorders.
Read More About Mood Disorders Here
6. Trauma
Trauma, such as physical or emotional abuse 15 Vitriol, V., Cancino, A., Weil, K., Salgado, C., Asenjo, M. A., & Potthoff, S. (2014). Depression and psychological trauma: an overview integrating current research and specific evidence of studies in the treatment of depression in public mental health services in chile. Depression research and treatment, 2014, 608671. https://doi.org/10.1155/2014/608671 , can lead to depression at night and other mental health conditions.
7. Artificial Light Exposure
Exposure to artificial light 16 Bedrosian, T. A., & Nelson, R. J. (2017). Timing of light exposure affects mood and brain circuits. Translational psychiatry, 7(1), e1017. https://doi.org/10.1038/tp.2016.262 , particularly blue light emitted by electronic devices, can disrupt the natural production of melatonin and disrupt sleep-wake cycles, which can lead to depression.
Anxiety And Depression At Night
Anxiety and depression at night are closely linked 17 Tiller J. W. (2013). Depression and anxiety. The Medical journal of Australia, 199(S6), S28–S31. https://doi.org/10.5694/mja12.10628 mental health challenges that can significantly impact an individual’s quality of life. Those who experience these conditions are at greater risk of irritability, suicidality, and sleep disturbance, which can exacerbate symptoms such as breathing issues, rapid heart rate, and nightmares during attempts to fall asleep.
The tendency to awaken at night with intrusive thoughts 18 Tiller J. W. (2013). Depression and anxiety. The Medical journal of Australia, 199(S6), S28–S31. https://doi.org/10.5694/mja12.10628 is a major factor that worsens nighttime depression and anxiety symptoms, disrupting sleep and leading to a cycle of worsening symptoms. Lack of distraction 19 Roelofs, J., Rood, L., Meesters, C., te Dorsthorst, V., Bögels, S., Alloy, L. B., & Nolen-Hoeksema, S. (2009). The influence of rumination and distraction on depressed and anxious mood: a prospective examination of the response styles theory in children and adolescents. European child & adolescent psychiatry, 18(10), 635–642. https://doi.org/10.1007/s00787-009-0026-7 at night can further imbalance an individual’s state of mind, making it difficult to manage symptoms and achieve restful sleep.
Diagnosis of Depression at Night
If symptoms last longer than two weeks, it is advised to seek help from a mental health professional 20 Depression in adults: treatment and management. (2022). In PubMed. National Institute for Health and Care Excellence (NICE). Available from: https://www.ncbi.nlm.nih.gov/books/NBK583074/ An MHP will evaluate your symptoms, consider any recent life events, review family history of mental illness, and explore other contributing factors to provide appropriate support.
They may use several self-assessment tests to outline an appropriate treatment plan, such as:
- The Hamilton Depression Rating Scale 21 Ma, S., Yang, J., Yang, B., Kang, L., Wang, P., Zhang, N., Wang, W., Zong, X., Wang, Y., Bai, H., Guo, Q., Yao, L., Fang, L., & Liu, Z. (2021). The Patient Health Questionnaire-9 vs. the Hamilton Rating Scale for Depression in Assessing Major Depressive Disorder. Frontiers in psychiatry, 12, 747139. https://doi.org/10.3389/fpsyt.2021.747139
- Minnesota Multiphasic Personality Inventory 22 Floyd, A. E., & Gupta, V. (2022, April 28). Minnesota Multiphasic Personality Inventory. PubMed; StatPearls Publishing. Available from: https://www.ncbi.nlm.nih.gov/books/NBK557525/
- Beck Depression Inventory 23 García-Batista, Z. E., Guerra-Peña, K., Cano-Vindel, A., Herrera-Martínez, S. X., & Medrano, L. A. (2018). Validity and reliability of the Beck Depression Inventory (BDI-II) in general and hospital population of Dominican Republic. PloS one, 13(6), e0199750. https://doi.org/10.1371/journal.pone.0199750
How To Stop Depression At Night?
Nighttime depression treatment 24 Duval, F., Lebowitz, B. D., & Macher, J. P. (2006). Treatments in depression. Dialogues in clinical neuroscience, 8(2), 191–206. https://doi.org/10.31887/DCNS.2006.8.2/fduval includes various forms of psychological treatment and medication. These are discussed below:
I. Therapy
Therapies can be an effective form to deal with individuals 25 Information, N. C. for B., Pike, U. S. N. L. of M. 8600 R., MD, B., & Usa, 20894. (2020). Treatments for depression. In www.ncbi.nlm.nih.gov. Institute for Quality and Efficiency in Health Care (IQWiG). Available from: https://www.ncbi.nlm.nih.gov/books/NBK279282/ with nighttime depression. It includes techniques like,
Read More About Therapy Here
- Cognitive Behavioral Therapy (CBT)
Cognitive Behavioral Therapy (CBT) is an evidence-based form of therapy that helps individuals recognize and change negative thought patterns and behaviors 26 Gautam, M., Tripathi, A., Deshmukh, D., & Gaur, M. (2020). Cognitive Behavioral Therapy for Depression. Indian journal of psychiatry, 62(Suppl 2), S223–S229. https://doi.org/10.4103/psychiatry.IndianJPsychiatry_772_19 For those struggling with nighttime depression, CBT can be especially helpful in identifying and challenging the unhelpful thoughts that often surface at night. It also equips individuals with practical strategies to manage and cope with distressing emotions during the evening hours.
Read More About Cognitive Behavioral Therapy (CBT) Here
- Light Therapy
Light therapy involves exposure to bright light 27 Campbell, P. D., Miller, A. M., & Woesner, M. E. (2017). Bright Light Therapy: Seasonal Affective Disorder and Beyond. The Einstein journal of biology and medicine : EJBM, 32, E13–E25. , which can help regulate circadian rhythms and improve mood. For those with nighttime depression, light therapy may involve exposure to bright light in the morning or early evening to help reset the body’s internal clock.
- Mindfulness-Based Therapy
Mindfulness-based therapies, like mindfulness-based cognitive therapy (MBCT 28 Tickell, A., Ball, S., Bernard, P., Kuyken, W., Marx, R., Pack, S., Strauss, C., Sweeney, T., & Crane, C. (2020). The Effectiveness of Mindfulness-Based Cognitive Therapy (MBCT) in Real-World Healthcare Services. Mindfulness, 11(2), 279–290. https://doi.org/10.1007/s12671-018-1087-9 ), can support individuals struggling with nighttime depression by increasing their awareness of thoughts and emotions. This heightened awareness can lead to healthier, more effective ways of coping with symptoms that tend to worsen at night.
II. Pharmacotherapy
Psychiatrists may prescribe various types of antidepressants 29 Information, N. C. for B., Pike, U. S. N. L. of M. 8600 R., MD, B., & Usa, 20894. (2020). Treatments for depression. In www.ncbi.nlm.nih.gov. Institute for Quality and Efficiency in Health Care (IQWiG). Available from: https://www.ncbi.nlm.nih.gov/books/NBK279282/ as a medication for nighttime depression, including:
Read More About Antidepressants Here
- Tricyclic and Tetracyclic Antidepressants (TCAs)
- Selective Serotonin Reuptake Inhibitors (SSRIs)
- Selective Serotonin and Noradrenaline Reuptake Inhibitors (SNRIs)
How to Fight Against Depression at Night
Consider the following tips for coping with 30 Goldman, L. S., Nielsen, N. H., & Champion, H. C. (1999). Awareness, diagnosis, and treatment of depression. Journal of general internal medicine, 14(9), 569–580. https://doi.org/10.1046/j.1525-1497.1999.03478.x depression at night:
- Consult a mental health professional if the symptoms persist for 2 weeks or more.
- Try to avoid mobile phone use or screen time 31 Hale, L., Kirschen, G. W., LeBourgeois, M. K., Gradisar, M., Garrison, M. M., Montgomery-Downs, H., Kirschen, H., McHale, S. M., Chang, A. M., & Buxton, O. M. (2018). Youth Screen Media Habits and Sleep: Sleep-Friendly Screen Behavior Recommendations for Clinicians, Educators, and Parents. Child and adolescent psychiatric clinics of North America, 27(2), 229–245. https://doi.org/10.1016/j.chc.2017.11.014 one hour before sleeping.
- Synchronize your biological clock 32 Wirz-Justice A. (2008). Diurnal variation of depressive symptoms. Dialogues in clinical neuroscience, 10(3), 337–343. https://doi.org/10.31887/DCNS.2008.10.3/awjustice to stabilize your mental health at night.
- Try to maintain a healthy diet which is beneficial for improving one’s frame of mind.
- Physical exercises and relaxation techniques, such as yoga or meditation 33 Parmentier, F. B. R., García-Toro, M., García-Campayo, J., Yañez, A. M., Andrés, P., & Gili, M. (2019). Mindfulness and Symptoms of Depression and Anxiety in the General Population: The Mediating Roles of Worry, Rumination, Reappraisal and Suppression. Frontiers in psychology, 10, 506. https://doi.org/10.3389/fpsyg.2019.00506 are advisable to cope with nighttime depression.
- Avoid intake of caffeine or substance use before sleeping.
- Write and maintain a sleep journal to improve your mood 34 Sohal, M., Singh, P., Dhillon, B. S., & Gill, H. S. (2022). Efficacy of journaling in the management of mental illness: a systematic review and meta-analysis. Family medicine and community health, 10(1), e001154. https://doi.org/10.1136/fmch-2021-001154 by expressing emotions like anger, pain, and other emotions.
- Communicating with your loved ones like, partners, friends or family can be also effective for individuals with nighttime depression.
Takeaway
For some people, the symptoms of depression get worse at night. In such cases, he or she should be watchful of conditions that trigger their mental health condition. A proper diagnosis and timely treatment are necessary for full recovery from nighttime depression. It is recommended to continue with the treatment until the individual feels fine by him/herself.
At a Glance
- Nighttime depression is a mental health condition where the symptoms of depression get worse at night.
- Nighttime depression symptoms can include feelings of sadness, hopelessness, and anxiety, as well as disrupted sleep patterns.
- Anxiety and depression frequently coexist in individuals.
- Different factors such as heredity, artificial light exposure, and overthinking play significant roles in nighttime depression.
- Communicating openly with loved ones can help in addressing depression at night.
- It can be addressed by treatment like medication or psychotherapies.
- Nighttime depression medication should be taken after seeking guidance from a qualified psychiatrist.
Frequently Asked Questions (FAQs)
1. Why do I get depressed at night?
There are several factors for this, including the tendency of overthinking which can be considered a major factor in developing nighttime depression.
2. How long can nighttime depression last?
The symptoms of nighttime depression can last for six to eight months.
3. Why do I get anxious at night?
Stressful life events such as sudden death in a family or work stress can be associated with anxiety during night time.