Depression can be a debilitating condition. But with some proven and beneficial self-help techniques, you can develop specific skills for coping with depression. This will help you better manage your symptoms and start your journey towards recovery.
Devising Healthy Ways Of Coping With Depression
Suffering from major depressive disorder (MDD) can make you feel mentally and emotionally exhausted. You may feel empty, fatigued, and lose interest in your relationships, career, or other important aspects of your life.
As being depressed makes you feel overwhelmed with negative thoughts and feelings, you may also lack the will and energy 1 Orzechowska, A., Zajączkowska, M., Talarowska, M., & Gałecki, P. (2013). Depression and ways of coping with stress: a preliminary study. Medical science monitor : international medical journal of experimental and clinical research, 19, 1050–1056. https://doi.org/10.12659/MSM.889778 to improve yourself or seek treatment.
However, you must find the strength and work on improving your mental health and take steps for coping with depression. Start by taking small, meaningful steps and slowly work towards enhancing your overall well-being.
Instead of taking to damaging self-medication or unhealthy mechanisms for coping with depression—such as consuming alcohol or drugs, binge eating, or overworking—focus on certain activities that make you happier and relaxed. Some effective self-help strategies can enable you to overcome your depression naturally by building healthy, positive habits.
However, it is also important that you seek medical treatment, as these techniques are not adequate substitutes for medical attention. Instead, try taking those steps that support the treatment plan and facilitate the recovery process.
Research 2 Edraki, M., Rambod, M., & Molazem, Z. (2018). The Effect of Coping Skills Training on Depression, Anxiety, Stress, and Self-Efficacy in Adolescents with Diabetes: A Randomized Controlled Trial. International journal of community based nursing and midwifery, 6(4), 324–333. shows that “coping skills training reduced depression, anxiety, and stress, and improved the patients’ self-efficacy.”
Another 2018 study 3 van Grieken, R. A., van Tricht, M. J., Koeter, M., van den Brink, W., & Schene, A. H. (2018). The use and helpfulness of self-management strategies for depression: The experiences of patients. PloS one, 13(10), e0206262. https://doi.org/10.1371/journal.pone.0206262 found that different self-management techniques—including physical activities and strategies for engagement—are “most helpful” in recovering from this condition.
10 Self-help Tips For Coping With Depression
Here are some of the most effective strategies for coping with depression, stress, and anxiety, as well as boosting positive thinking:
1. Consult a therapist
The first step toward coping with depression involves talking to a mental health professional about your thoughts, feelings, and experiences.
This can help you significantly, for they make it easier for you to understand your symptoms and triggers and develop an effective treatment plan 4 Duval, F., Lebowitz, B. D., & Macher, J. P. (2006). Treatments in depression. Dialogues in clinical neuroscience, 8(2), 191–206. https://doi.org/10.31887/DCNS.2006.8.2/fduval involving therapies, medications, and common coping skills for depression.
Cooperate with your therapist to find the best treatment for your mood disorders and follow their instructions by taking medications regularly, attending therapy sessions, and going for follow-up appointments.
Read More About Therapy Here
2. Shift your mindset
MDD is a common condition that affects millions of people worldwide. Although experiences of the condition are subjective, people more or less experience the same difficulties and challenges.
So instead of giving up and giving in to your depression, accept that you have a mental illness; however, also remember that coping with depression and successfully recovering from it requires the right effort and determination.
Acknowledge your issues and be kind and loving to yourself. Understand that what you are going through now does not have to decide or dominate your future.
Change your perspective, be aware of your condition, and develop effective skills for coping with depression. Practice self-care and focus on building a positive mindset instead of dwelling on negative thoughts.
3. Connect with others
Instead of withdrawing or isolating yourself, focus on building a strong support network which can only happen when you –
- Talk to your loved ones
- Spend time with friends
- Enjoy some group activities, and
- Connect with your community or online groups.
Your support network can provide you with motivation and encouragement when you need it the most, which in turn will help you in coping with depression. Studies 5 Matthews, T., Danese, A., Wertz, J., Odgers, C. L., Ambler, A., Moffitt, T. E., & Arseneault, L. (2016). Social isolation, loneliness and depression in young adulthood: A behavioural genetic analysis. Social Psychiatry and Psychiatric Epidemiology, 51(3), 339-348. https://doi.org/10.1007/s00127-016-1178-7 have found that isolation can make depressive disorders worse, whereas support groups can be substantially helpful 6 Pfeiffer, P. N., Heisler, M., Piette, J. D., Rogers, M. A., & Valenstein, M. (2011). Efficacy of peer support interventions for depression: A meta-analysis. General Hospital Psychiatry, 33(1), 29-36. https://doi.org/10.1016/j.genhosppsych.2010.10.002 .
Spending time with your loved ones and community will help you gain a sense of belonging and purpose and boost your well-being.
4. Manage stress
When you are coping with depression, try reducing your stress levels by eliminating avoidable and unnecessary stressors which can make your symptoms worse.
Stress leads to the production of the hormone cortisol which can make MDD a serious issue in the long run. Research 7 Dedovic, K., & Ngiam, J. (2015). The cortisol awakening response and major depression: examining the evidence. Neuropsychiatric disease and treatment, 11, 1181–1189. https://doi.org/10.2147/NDT.S62289 reveals “an important, but complex, association between CAR (cortisol awakening response) and vulnerability to depression.”
Apart from sticking to your treatment plan, making lifestyle changes and practicing stress reduction techniques (like deep breathing 8 Ma, X., Yue, Z. Q., Gong, Z. Q., Zhang, H., Duan, N. Y., Shi, Y. T., Wei, G. X., & Li, Y. F. (2017). The Effect of Diaphragmatic Breathing on Attention, Negative Affect and Stress in Healthy Adults. Frontiers in psychology, 8, 874. https://doi.org/10.3389/fpsyg.2017.00874 and meditation 9 Canter P. H. (2003). The therapeutic effects of meditation. BMJ (Clinical research ed.), 326(7398), 1049–1050. https://doi.org/10.1136/bmj.326.7398.1049 ) can help you manage your depressive symptoms like low self-esteem.
Read More About Stress Here
5. Set realistic goals
Recovery can take some time and patience. So make sure to set small, practical goals that you can achieve in a short period of time.
Not only achieving these small goals will help boost your confidence and self-esteem, but also it will motivate you to achieve more. So, take one small step at a time and use this approach in completing your daily tasks and chores as well. Over time, coping with depression will become easier!
6. Avoid substance use
The use of alcohol and drugs can make your depression a lot worse. In fact, substance use disorder 10 Davis, L., Uezato, A., Newell, J. M., & Frazier, E. (2008). Major depression and comorbid substance use disorders. Current Opinion in Psychiatry, 21(1), 14-18. https://doi.org/10.1097/yco.0b013e3282f32408 can become a comorbid condition for major depressive disorder.
Although substances, like drugs, alcohol, and nicotine may offer some temporary relief while coping with depression, they can make the symptoms more severe in the long run and increase the risk of suicide 11 Wu, P., Hoven, C. W., Liu, X., Cohen, P., Fuller, C. J., & Shaffer, D. (2004). Substance use, suicidal ideation and attempts in children and adolescents. Suicide & life-threatening behavior, 34(4), 408–420. https://doi.org/10.1521/suli.34.4.408.53733 .
“Those with depression and/or poor mental health functioning are at high risk for the physical and psychological consequences of substance use,” explains a 2012 study 12 Booth, B. M., Walton, M. A., Barry, K. L., Cunningham, R. M., Chermack, S. T., & Blow, F. C. (2011). Substance use, depression, and mental health functioning in patients seeking acute medical care in an inner-city ED. The journal of behavioral health services & research, 38(3), 358–372. https://doi.org/10.1007/s11414-010-9227-6 . Hence, it is crucial to avoid drugs and alcohol when you are depressed as it can fasten the recovery process.
Read More About Alcoholism Here
7. Build and follow a routine
As being depressed can affect your daily functioning, relationships, career, and personal life, it is important that you create a routine for coping with depression and stick to it. Following a regular, healthy routine will help build your self-esteem and motivate you to become more productive by avoiding disorganization and procrastination.
However, make sure your daily routine is structured, simple, and gentle—this should balance the different aspects of life without making you feel stressed or overwhelmed.
8. Exercise regularly
Research 13 Shaphe, M. A., & Chahal, A. (2020). Relation of Physical Activity with the Depression: A Short Review. Journal of lifestyle medicine, 10(1), 1–6. https://doi.org/10.15280/jlm.2020.10.1.1 shows that physical exercise can be a viable mechanism for coping with depression without medication.
Staying physically active and engaging in regular exercise is perhaps one of the most effective strategies for coping with depression. Getting 20-60 minutes of exercise daily 14 Craft, L. L., & Perna, F. M. (2004). The Benefits of Exercise for the Clinically Depressed. Primary care companion to the Journal of clinical psychiatry, 6(3), 104–111. https://doi.org/10.4088/pcc.v06n0301 —whether it’s cardio training, weight lifting, biking, swimming, or simply going for a walk—can help to improve your mood, confidence, and self-esteem and relieve depressive symptoms.
Moderate or high-intensity training can provide significant emotional and physiological benefits in reducing your stress levels, apart from its obvious physical benefits.
According to a 2018 study 15 Belvederi Murri, M., Ekkekakis, P., Magagnoli, M., Zampogna, D., Cattedra, S., Capobianco, L., Serafini, G., Calcagno, P., Zanetidou, S., & Amore, M. (2019). Physical Exercise in Major Depression: Reducing the Mortality Gap While Improving Clinical Outcomes. Frontiers in psychiatry, 9, 762. https://doi.org/10.3389/fpsyt.2018.00762 , “exercise offers numerous physical benefits, which can counteract several mechanisms postulated to increase mortality risk in depression,” and “if prescribed and delivered correctly, exercise can be as effective as other first-line treatments, while being mostly free of adverse side-effects.”
9. Practice better sleep hygiene
Sleep is closely associated with your mood regulation and sound mental health. Studies 16 Soehner, A. M., Kaplan, K. A., & Harvey, A. G. (2014). Prevalence and clinical correlates of co-occurring insomnia and hypersomnia symptoms in depression. Journal of Affective Disorders, 167, 93-97. https://doi.org/10.1016/j.jad.2014.05.060 show that most sufferers experience sleep disturbances and hypersomnia; in fact, insomnia is closely associated with major depressive episodes. This is why you must build a healthier sleep routine to get at least 8-9 hours of sleep every day.
Although falling asleep 17 Rahimi, A., Ahmadpanah, M., Shamsaei, F., Cheraghi, F., Sadeghi Bahmani, D., Holsboer-Trachsler, E., & Brand, S. (2016). Effect of adjuvant sleep hygiene psychoeducation and lorazepam on depression and sleep quality in patients with major depressive disorders: results from a randomized three-arm intervention. Neuropsychiatric disease and treatment, 12, 1507–1515. https://doi.org/10.2147/NDT.S110978 or getting out of bed can be difficult for depressed individuals, practicing a healthy sleep hygiene 18 Rezaei, M., Khormali, M., Akbarpour, S., Sadeghniiat-Hagighi, K., & Shamsipour, M. (2018). Sleep quality and its association with psychological distress and sleep hygiene: a cross-sectional study among pre-clinical medical students. Sleep science (Sao Paulo, Brazil), 11(4), 274–280. https://doi.org/10.5935/1984-0063.20180043 regime can help you overcome these problems.
For coping with depression consider the following sleep hygiene tips:
- Make sure to go to sleep at a reasonable time daily
- Use a dim light in the bedroom
- Avoid using technology (like your smartphone before bedtime)
- Avoid working before going to sleep.
- Consult with your therapist about any sleep problems you may be facing
10. Have a healthier, nutritious diet
Diet and nutrition 19 Sarris, J., Logan, A. C., Akbaraly, T. N., Amminger, G. P., Balanzá-Martínez, V., Freeman, M. P., Hibbeln, J., Matsuoka, Y., Mischoulon, D., Mizoue, T., Nanri, A., Nishi, D., Ramsey, D., Rucklidge, J. J., Sanchez-Villegas, A., Scholey, A., Su, K., & Jacka, F. N. (2015). Nutritional medicine as mainstream in psychiatry. The Lancet Psychiatry, 2(3), 271-274. https://doi.org/10.1016/s2215-0366(14)00051-0 have a direct influence on your mood.
“Poor nutrition may be a causal factor in the experience of low mood, and improving diet may help to protect not only the physical health but also the mental health of the population,” explains a recent 2020 study 20 Firth, J., Gangwisch, J. E., Borisini, A., Wootton, R. E., & Mayer, E. A. (2020). Food and mood: how do diet and nutrition affect mental wellbeing?. BMJ (Clinical research ed.), 369, m2382. https://doi.org/10.1136/bmj.m2382 .
There is no doubt that having a better, more nutritious diet can help you improve your physical and mental health. According to nutritional psychiatry 21 Adan, R., van der Beek, E. M., Buitelaar, J. K., Cryan, J. F., Hebebrand, J., Higgs, S., Schellekens, H., & Dickson, S. L. (2019). Nutritional psychiatry: Towards improving mental health by what you eat. European neuropsychopharmacology : the journal of the European College of Neuropsychopharmacology, 29(12), 1321–1332. https://doi.org/10.1016/j.euroneuro.2019.10.011 , eating a healthier diet can help us better manage mood disorders, such as depression and anxiety.
A diet heavy in omega-3 fatty acids and devoid of sugar and trans fat can help you better in coping with depression. You can also add the following food items to your diet when coping with depression22 Francis, H. M., Stevenson, R. J., Chambers, J. R., Gupta, D., Newey, B., & Lim, C. K. (2019). A brief diet intervention can reduce symptoms of depression in young adults – A randomised controlled trial. PLOS ONE, 14(10), e0222768. https://doi.org/10.1371/journal.pone.0222768 :
- Fish
- Protein (poultry, eggs, etc.)
- Fruits and vegetables
- Nuts and seeds spices
- Wholegrain cereals
- Olive oil
In fact, one 2019 study 23 Huang, Q., Liu, H., Suzuki, K., Ma, S., & Liu, C. (2019). Linking What We Eat to Our Mood: A Review of Diet, Dietary Antioxidants, and Depression. Antioxidants (Basel, Switzerland), 8(9), 376. https://doi.org/10.3390/antiox8090376 states, “Balanced dietary patterns such as the Mediterranean diet and certain foods such as fish, fresh vegetables, and fruits have been associated with a lower risk of depression or depressive symptoms, while high-fat Western diets and sugar-sweetened beverages have been associated with higher risk of depression or depressive symptoms.”
Other Self-help Strategies For Coping With Depression
Apart from the aforementioned self-managed ways for coping with depression and anxiety, try considering some non-medical and leisurely ways to deal with your depressive symptoms.
Self-help tips for coping with depression may include:
1. Spending time outside in nature
Step outside and get some exposure to the sun. Studies 24 Pearson, D. G., & Craig, T. (2014). The great outdoors? Exploring the mental health benefits of natural environments. Frontiers in Psychology, 5. https://doi.org/10.3389/fpsyg.2014.01178 have shown that spending time in nature can improve your mental health and cognition and reduce depressive symptoms. So, try nature therapy for coping with depression.
2. Cuddling with a pet
Being with a pet 25 Thelwell E. (2019). Paws for Thought: A Controlled Study Investigating the Benefits of Interacting with a House-Trained Dog on University Students Mood and Anxiety. Animals : an open access journal from MDPI, 9(10), 846. https://doi.org/10.3390/ani9100846 can offer you companionship, comfort, and emotional support. Moreover, taking care of your pet will give you a sense of purpose and allow you to use your energy positively. A 2018 study 26 Brooks, H. L., Rushton, K., Lovell, K., Bee, P., Walker, L., Grant, L., & Rogers, A. (2018). The power of support from companion animals for people living with mental health problems: a systematic review and narrative synthesis of the evidence. BMC psychiatry, 18(1), 31. https://doi.org/10.1186/s12888-018-1613-2 states “pets provide benefits to those with mental health conditions.” Both nature and pet therapy are proven to boost skills for coping with depression.
3. Practicing self-care
Taking care of yourself 27 Pilkington, K., & Wieland, L. S. (2020). Self-care for anxiety and depression: a comparison of evidence from Cochrane reviews and practice to inform decision-making and priority-setting. BMC complementary medicine and therapies, 20(1), 247. https://doi.org/10.1186/s12906-020-03038-8 and practicing small acts of self-love is vital for your recovery from major depressive disorder.
With such a positive and self-nurturing mindset, you can boost your mood, self-esteem, and confidence – that will further accelerate coping with depression.
Read More About Self-Love Here
4. Practicing journaling
Keeping a journal can help you in coping with depression 28 Aselton, P. (2012). Sources of stress and coping in American College students who have been diagnosed with depression. Journal of Child and Adolescent Psychiatric Nursing, 25(3), 119-123. https://doi.org/10.1111/j.1744-6171.2012.00341.x by allowing you to express your innermost thoughts and beliefs without fearing judgment or criticism.
It can also help you identify triggers and develop healthier, more organized patterns of thought and behavior. “Expressive writing may be a useful supplement to existing interventions for depression,” found a 2013 study 29 Krpan, K. M., Kross, E., Berman, M. G., Deldin, P. J., Askren, M. K., & Jonides, J. (2013). An everyday activity as a treatment for depression: the benefits of expressive writing for people diagnosed with major depressive disorder. Journal of affective disorders, 150(3), 1148–1151. https://doi.org/10.1016/j.jad.2013.05.065 .
5. Practicing mindfulness
Mindfulness is the practice of bringing your awareness to the present moment without getting attached to negative thoughts and feelings. Research 30 Takahashi, T., Sugiyama, F., Kikai, T., Kawashima, I., Guan, S., Oguchi, M., Uchida, T., & Kumano, H. (2019). Changes in depression and anxiety through mindfulness group therapy in Japan: the role of mindfulness and self-compassion as possible mediators. BioPsychoSocial medicine, 13, 4. https://doi.org/10.1186/s13030-019-0145-4 shows that mindfulness can significantly help in decreasing anxiety and depressive symptoms.
Mindfulness meditation” focusing on reducing worry and rumination may be especially useful in reducing the risk of developing clinical depression,” explains a 2019 study 31 Parmentier, F., García-Toro, M., García-Campayo, J., Yañez, A. M., Andrés, P., & Gili, M. (2019). Mindfulness and Symptoms of Depression and Anxiety in the General Population: The Mediating Roles of Worry, Rumination, Reappraisal and Suppression. Frontiers in psychology, 10, 506. https://doi.org/10.3389/fpsyg.2019.00506 .
Some more beneficial coping with depression strategies include:
- Socializing more often 32 Ozbay, F., Johnson, D. C., Dimoulas, E., Morgan, C. A., Charney, D., & Southwick, S. (2007). Social support and resilience to stress: from neurobiology to clinical practice. Psychiatry (Edgmont (Pa. : Township, 4(5), 35–40. [/mfn] and spending time with loved ones
- Being more creative 33 Andreasen N. C. (2008). The relationship between creativity and mood disorders. Dialogues in clinical neuroscience, 10(2), 251–255. https://doi.org/10.31887/DCNS.2008.10.2/ncandreasen by trying painting 34 Stuckey, H. L., & Nobel, J. (2010). The connection between art, healing, and public health: a review of current literature. American journal of public health, 100(2), 254–263. https://doi.org/10.2105/AJPH.2008.156497 , writing poetry or stories, or playing a musical instrument
- Rewarding yourself by appreciating your efforts and small achievements
- Listening to music or watching a movie
- Volunteering 35 Tabassum, F., Mohan, J., & Smith, P. (2016). Association of volunteering with mental well-being: a lifecourse analysis of a national population-based longitudinal study in the UK. BMJ open, 6(8), e011327. https://doi.org/10.1136/bmjopen-2016-011327 to help others who need support
- Practicing gratitude 36 Kini, P., Wong, J., McInnis, S., Gabana, N., & Brown, J. W. (2016). The effects of gratitude expression on neural activity. NeuroImage, 128, 1–10. https://doi.org/10.1016/j.neuroimage.2015.12.040 by writing about 3 things you’re thankful for each day
- Reading fictional or self-help books
- Taking a good, relaxing bath
- Arranging a get-together with friends
- Learning new skills
- Challenging and questioning negative thoughts
- Trying alternative coping with depression strategies like Yoga 37 Vorkapic C. F. (2016). Yoga and mental health: A dialogue between ancient wisdom and modern psychology. International journal of yoga, 9(1), 67–71. https://doi.org/10.4103/0973-6131.171720 , Tai Chi 38 Abbott, R., & Lavretsky, H. (2013). Tai Chi and Qigong for the treatment and prevention of mental disorders. The Psychiatric clinics of North America, 36(1), 109–119. https://doi.org/10.1016/j.psc.2013.01.011 , Qigong, and acupuncture 39 Samuels, N., Gropp, C., Singer, S. R., & Oberbaum, M. (2008). Acupuncture for psychiatric illness: a literature review. Behavioral medicine (Washington, D.C.), 34(2), 55–64. https://doi.org/10.3200/BMED.34.2.55-64
- Meeting new people by joining a club or an online group
- Practicing spirituality 40 Verghese A. (2008). Spirituality and mental health. Indian journal of psychiatry, 50(4), 233–237. https://doi.org/10.4103/0019-5545.44742 , such as saying prayers
- Doing things you enjoy
Read More About Mindfulness Here
What Are The Strategies For Coping With Depression At Work?
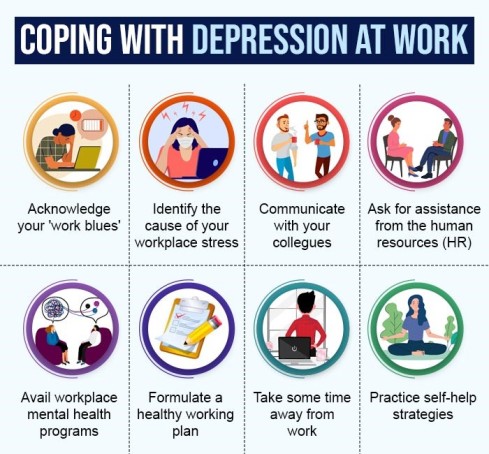
Depression cripples your everyday functioning, especially at work. When you suffer from depression, you may lag behind in meeting your professional goals and targets.
Most often, you will feel yourself losing concentration, lacking the energy to perform tasks, or missing important deadlines. At other times, you may give your workday a miss and develop a pathological habit to avoid your workplace at all costs.
To function effectively at work and achieve your personal and professional objectives, consider ways in which you can manage your ‘work blues’. For coping with depression at work, try the following measures:
1. Acknowledging your depression
The first step in coping with depression and workplace stress is acknowledging that you have depression. Come to terms with your feelings and try to figure out what it is that is causing you to feel that way.
For instance, serious workplace issues like harassment, discrimination, abuse, and bullying can lead to depressive symptoms. Sometimes job demands, the occupational culture, and job dissatisfaction can trigger depression.
Therefore, consider ways in which you can address and/or resolve these issues that are affecting your mental health.
2. Asking for assistance at work
Ask for assistance in your effort to do away with your work blues. For instance, try communicating with your colleagues and superiors, if you think you need help to better manage the job demands.
Turn to the department of human resources to address any concerns related to harassment or bullying. If you can afford it, try switching to jobs that offer job satisfaction without taking a toll on your mental health.
3. Availing your organization’s mental health programs
Labor laws 41 Goetzel, R. Z., Roemer, E. C., Holingue, C., Fallin, M. D., McCleary, K., Eaton, W., Agnew, J., Azocar, F., Ballard, D., Bartlett, J., Braga, M., Conway, H., Crighton, K. A., Frank, R., Jinnett, K., Keller-Greene, D., Rauch, S. M., Safeer, R., Saporito, D., Schill, A., … Mattingly, C. R. (2018). Mental Health in the Workplace: A Call to Action Proceedings From the Mental Health in the Workplace-Public Health Summit. Journal of occupational and environmental medicine, 60(4), 322–330. https://doi.org/10.1097/JOM.0000000000001271 warrant that both employees and employers can avail opportunities that help them take care of their physical and mental health—such as coping with depression, stress, and anxiety at the workplace.
Certain workplaces provide “mental health leaves” or occupational therapy programs 42 Hogg, B., Medina, J. C., Gardoki-Souto, I., Serbanescu, I., Moreno-Alcázar, A., Cerga-Pashoja, A., Coppens, E., Tóth, M. D., Fanaj, N., Greiner, B. A., Holland, C., Kõlves, K., Maxwell, M., Qirjako, G., de Winter, L., Hegerl, U., Pérez-Sola, V., Arensman, E., & Amann, B. L. (2021). Workplace interventions to reduce depression and anxiety in small and medium-sized enterprises: A systematic review. Journal of affective disorders, 290, 378–386. https://doi.org/10.1016/j.jad.2021.04.071 for employees’ welfare.
Try coping with depression at work using such programs; however, educate yourself beforehand about the details of the mental health program you would be participating in.
4. Formulating an effective working plan
Try formulating an effective working plan 43 Rajgopal T. (2010). Mental well-being at the workplace. Indian journal of occupational and environmental medicine, 14(3), 63–65. https://doi.org/10.4103/0019-5278.75691 to address your depressive symptoms at work.
You can try timing your tasks, scheduling small breaks, taking a power nap, or planning a lunch outside. These tiny techniques can help you refresh your mood and focus and renew your motivation to get tasks done.
5. Planning time away from work
If it gets extremely overwhelming, consider taking a small vacation. For instance, if you think your workplace is making you sick, distance yourself from it for some time. Communicate with your colleagues and say that you will not be responding to work calls or emails while you are away, as you need time for yourself to recharge and heal.
Spend some quality time with yourself, your family, and your friends. Try new activities or do old activities that make you feel happy and purposeful. Taking time away from work surely helps in coping with depression.
6. Practicing self-care strategies
Practice some self-care healthy ways of coping with depression at work. For example, psychologists 44 Umberson, D., & Montez, J. K. (2010). Social relationships and health: a flashpoint for health policy. Journal of health and social behavior, 51 Suppl(Suppl), S54–S66. https://doi.org/10.1177/0022146510383501 say that strong social ties at work positively influence mental health and work productivity.
You can try socializing with your colleagues. Spend time with them and build a good rapport. This may help you to better embrace your workspace and work culture. You can also try other measures for coping with depression at work, such as:
- Using stress balls during working hours
- Going out for a group lunch
- Attending leisurely events
- Hiking
- Gardening, etc.
Takeaway
Major depressive disorder is a severely debilitating disorder that impacts your quality of life and interpersonal relationships. Therefore, it is crucial that you must treat it timely and with the right diagnosis.
Having a personal understanding of how to cope with depression can help you recover from it more quickly. Mostly, a treatment plan under the guidance of a healthcare professional works best for depression treatment. Self-help strategies for coping with depression will help hasten the process of recovery.
However, not all the coping techniques mentioned here will be applicable or effective for you, but you need to try different options to see which ones work for you. It is also important that you have patience and determination to take small steps towards full recovery.
Coping With Depression At A Glance
- Depression is a challenging mental health disorder. But there are strategies for effectively coping with depression.
- Such coping with depression strategies involve therapy, medication, and self-help strategies.
- Consider following a disciplined and long-term treatment program for depression.
- Having a personal understanding of your depressive symptoms can help you have a better grasp of your recovery process.
- Try coping with depression with self-help strategies that are safe, fun, and mood-boosting.
- Build a social support system for coping with depression and quick recovery.