Trichotillomania, also known as hair-pulling disorder, is a mental health condition characterized by a recurrent, irresistible urge to pull out one’s own hair, typically from the scalp, eyebrows, eyelashes, or other parts of the body.
Key features:
- Repetitive hair-pulling that leads to noticeable hair loss.
- Often preceded by tension or anxiety, followed by relief or gratification after pulling.
- Can result in distress, social embarrassment, and functional impairment.
- Frequently co-occurs with other conditions like anxiety, depression, or OCD.
Causes may include:
- Genetic factors
- Brain chemistry imbalances
- Stress or trauma
- Behavioral conditioning
Treatment options:
- Cognitive-behavioral therapy (CBT), especially Habit Reversal Training (HRT)
- Medication (like SSRIs in some cases)
- Support groups and psychoeducation
It falls under Obsessive-Compulsive and Related Disorders in the DSM-5.
What Is Trichotillomania?
Trichotillomania is a mental health condition 1 Pereyra, A. D., & Saadabadi, A. (2021). Trichotillomania. PubMed; StatPearls Publishing. Available from: https://www.ncbi.nlm.nih.gov/books/NBK493186/ characterized by a recurrent and irresistible urge to pull out one’s hair, resulting in noticeable hair loss and distress. This condition falls under the category of Obsessive-Compulsive and Related Disorders 2 Administration, S. A. and M. H. S. (2016, June 1). Table 3.27, DSM-IV to DSM-5 Trichotillomania (Hair-Pulling Disorder) Comparison. Www.ncbi.nlm.nih.gov. Available from: https://www.ncbi.nlm.nih.gov/books/NBK519704/table/ch3.t27/ in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5).
Trichotillomania is classified as an impulse control disorder, characterized by a persistent struggle to resist the urge to pull out one’s own hair. This behavior is often triggered by emotional states such as stress, anxiety, boredom, or tension. While hair-pulling can affect any part of the body, it most commonly targets the scalp, eyebrows, and eyelashes.
Trichotillomania In Films
Unlike more commonly portrayed mental health conditions such as anxiety or depression, trichotillomania receives limited representation in film and television. In Young Adult (2011), Charlize Theron’s character, Mavis Gary, grapples with trichotillomania and the emotional toll it takes on her personal life. In Creep 2 (2017), the protagonist—who is a serial killer—appears to ‘inherit’ the disorder after killing a man who struggled with it. Other portrayals include Friend Request (2016), Alice, Darling (2022), and the psychological drama series Sharp Objects (2018), all of which feature characters dealing with the compulsion to pull out their own hair.
Prevalence Of Trichotillomania
Trichotillomania is a relatively common disorder affecting 1-2% of the global population 3 Franklin, M. E., Zagrabbe, K., & Benavides, K. L. (2011). Trichotillomania and its treatment: a review and recommendations. Expert review of neurotherapeutics, 11(8), 1165–1174. https://doi.org/10.1586/ern.11.93 . It exhibits a notable gender difference, with a higher prevalence in females, compared to males. Research suggests that approximately 70-90% of diagnosed cases are female. The typical age of onset is around 9-13 years old 4 Grant J. E. (2019). Trichotillomania (hair pulling disorder). Indian journal of psychiatry, 61(Suppl 1), S136–S139. https://doi.org/10.4103/psychiatry.IndianJPsychiatry_529_18 , although some individuals may develop the signs of trichotillomania in adulthood.
Signs Of Trichotillomania
Research 5 Cisoń, H., Kuś, A., Popowicz, E., Szyca, M., & Reich, A. (2018). Trichotillomania and Trichophagia: Modern Diagnostic and Therapeutic Methods. Dermatology and therapy, 8(3), 389–398. https://doi.org/10.1007/s13555-018-0256-z attributes the common signs of trichotillomania to the following:
- Recurrent hair-pulling
- Noticeable hair loss
- Focused on specific body areas (e.g., scalp, eyebrows)
- Tension or anxiety before pulling
- Pleasure, relief, or gratification during pulling
- Attempts to stop or reduce hair-pulling
- Social or occupational impairment
- Significant distress or emotional impact
What Causes Trichotillomania?
Studies 6 Parakh, P., & Srivastava, M. (2010). The many faces of trichotillomania. International journal of trichology, 2(1), 50–52. https://doi.org/10.4103/0974-7753.66916 on what causes trichotillomania have pointed to the following factors:
- Genetics
- Stress and emotional triggers
- Family history of a similar disorder
- Neurotransmitter imbalances
Read More About Genetics Here
The Mental Health Impact Of Trichotillomania
Trichotillomania can have a profound and often debilitating impact 7 França, K., Kumar, A., Castillo, D., Jafferany, M., Hyczy da Costa Neto, M., Damevska, K., Wollina, U., & Lotti, T. (2019). Trichotillomania (hair pulling disorder): Clinical characteristics, psychosocial aspects, treatment approaches, and ethical considerations. Dermatologic therapy, 32(4), e12622. https://doi.org/10.1111/dth.12622 on an individual’s mental health. Those affected often experience intense feelings of shame, embarrassment, and frustration due to their inability to control the hair-pulling impulses. The visible hair loss can lead to lowered self-esteem, body image issues, and social withdrawal, further exacerbating their emotional distress.
Anxiety and depression are common co-occurring conditions in individuals with trichotillomania, largely due to the emotional strain the disorder imposes. The persistent urge to pull out hair—and the resulting physical damage—can significantly disrupt daily functioning, work, and personal relationships, compounding the overall mental health burden. Furthermore, the stigma and secrecy surrounding trichotillomania often discourage individuals from seeking help, which can intensify feelings of isolation and worsen psychological distress.
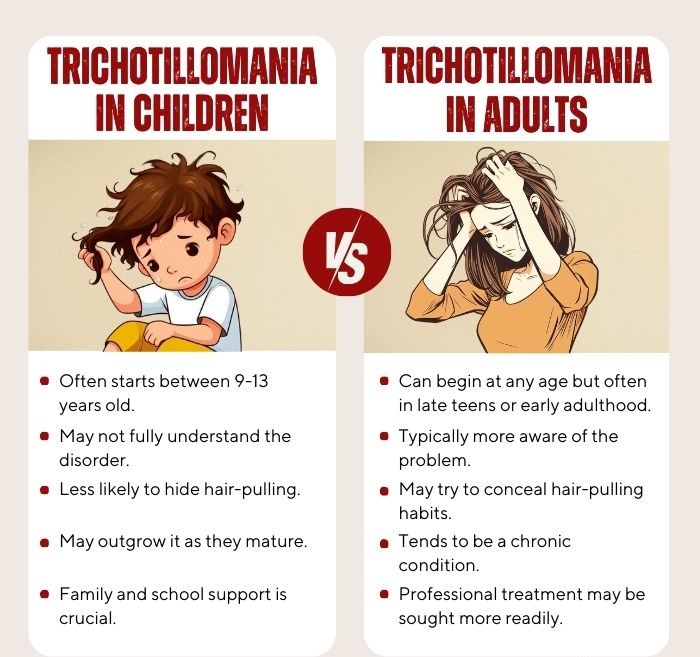
Trichotillomania In Children And Adults
Trichotillomania can manifest differently in children and adults, with unique considerations for each age group. In children, this condition often begins during pre-adolescence, around 9-13 years old 8 Walther, M. R., Ricketts, E. J., Conelea, C. A., & Woods, D. W. (2010). Recent Advances in the Understanding and Treatment of Trichotillomania. Journal of cognitive psychotherapy, 24(1), 46–64. https://doi.org/10.1891/0889-8391.24.1.46 , and can be challenging to detect, as children may try to conceal their hair-pulling behaviors. Parents and caregivers may notice unexplained hair loss, bald patches, or a decrease in the child’s self-esteem, academic performance, and social interactions.
In adults, the signs of trichotillomania can be equally distressing 9 Kaur, H., Chavan, B. S., & Raj, L. (2005). Management of trichotillomania. Indian journal of psychiatry, 47(4), 235–237. https://doi.org/10.4103/0019-5545.43063 . This condition may have persisted from childhood or developed in adulthood. Adults with trichotillomania may experience heightened self-consciousness, as the visible hair loss can be especially problematic in professional and social settings.
How Mental Illness Leads To Trichotillomania
Common mental health disorders associated with trichotillomania include 10 Huynh, M., Gavino, A. C., & Magid, M. (2013). Trichotillomania. Seminars in cutaneous medicine and surgery, 32(2), 88–94. https://doi.org/10.12788/j.sder.0007 :
1. Obsessive-compulsive disorder (OCD):
Commonalities include repetitive, compulsive behaviors and obsessive thoughts related to hair-pulling.
Read More About Obsessive-Compulsive Disorder (OCD) Here
2. Anxiety disorders:
Frequently co-occur with trichotillomania, including generalized anxiety disorder, social anxiety disorder, and panic disorder.
Read More About Anxiety Here
3. Depressive disorders:
Emotional distress from trichotillomania can lead to depression due to lowered self-esteem and sadness.
4. Body dysmorphic disorder (BDD):
Trichotillomania may be linked to concerns about hair imperfections, a component of BDD.
5. Skin picking (excoriation disorder):
Both involve repetitive, self-injurious behaviors often driven by emotional distress.
6. Substance use disorders:
Some individuals with trichotillomania may turn to substances like alcohol or drugs as a way to cope with emotional challenges, leading to potential substance use disorders.
How To Diagnose Trichotillomania
Diagnosing trichotillomania involves a comprehensive assessment 11 Chamberlain, S. R., Odlaug, B. L., Boulougouris, V., Fineberg, N. A., & Grant, J. E. (2009). Trichotillomania: neurobiology and treatment. Neuroscience and biobehavioral reviews, 33(6), 831–842. https://doi.org/10.1016/j.neubiorev.2009.02.002 by a qualified mental health specialist, typically a psychologist or psychiatrist. This process begins with a clinical interview where the individual discusses their symptoms, behaviors, and medical and psychiatric history. The clinician then evaluates whether these experiences align with the specific diagnostic criteria outlined in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5).
Additionally, a physical examination may be conducted to rule out medical conditions contributing to hair loss, while psychological assessments, including questionnaires and psychometric tests, help assess symptom severity and screen for comorbid mental health disorders. An accurate diagnosis is crucial for developing an effective treatment plan and support system for individuals affected by trichotillomania.
How To Treat Trichotillomania
The methods 12 Christenson, G. A., & Crow, S. J. (1996). The characterization and treatment of trichotillomania. The Journal of clinical psychiatry, 57 Suppl 8, 42–49. concerning how to treat trichotillomania include:
1. Cognitive-behavioral therapy (CBT):
CBT is the primary psychotherapeutic approach, focusing on identifying triggers, developing coping strategies, and replacing hair-pulling behaviors with healthier alternatives.
Read More About Cognitive Behavioral Therapy (CBT) Here
2. Habit reversal training (HRT):
HRT is a specialized form of CBT, specifically tailored for trichotillomania. It helps individuals become more aware of hair-pulling triggers and provides techniques to interrupt and redirect the behavior.
3. Medication:
Pharmacotherapy in trichotillomania usually involves antidepressants (like SSRIs) and amino acid supplements [such as N-Acetylcysteine (NAC)] that have shown promise in reducing hair-pulling symptoms.
Coping With Trichotillomania
Consider the following tips 13 Woods, D. W., & Houghton, D. C. (2014). Diagnosis, evaluation, and management of trichotillomania. The Psychiatric clinics of North America, 37(3), 301–317. https://doi.org/10.1016/j.psc.2014.05.005 for coping with trichotillomania:
- Identify triggers: Recognize and understand what prompts hair-pulling urges.
- Self-awareness: Become more conscious of your hair-pulling habits to intervene effectively.
- Habit replacement: Find alternative actions to replace hair-pulling, like fidget tools.
- Stress management: Learn stress-reduction techniques like meditation and deep breathing.
- Support system: Seek emotional support from friends, family, or support groups.
- Professional help: Consult with a specialist for measures on how to treat trichotillomania (like therapy).
- Keep a journal: Document episodes, triggers, and emotions to spot patterns.
- Positive reinforcement: Reward yourself for periods without hair-pulling.
- Barrier methods: Use physical barriers like gloves to deter hair-pulling.
- Mindfulness: Practice staying present to manage impulses effectively.
- Medication: Take prescribed medication for symptom management.
- Education: Learn about trichotillomania to better understand and cope with the condition.
- Patience: Progress may be gradual, so be kind and patient with yourself as you work on managing trichotillomania.
Read More About Mindfulness Here

Takeaway
Trichotillomania is a complex and often distressing condition that can affect individuals across all age groups, significantly impacting daily functioning and emotional well-being. Although its exact causes are still being researched, effective management is possible through a combination of psychotherapy, medication, and self-help techniques.
Early diagnosis and timely intervention play a vital role in helping individuals regain control over their urges and improve their overall quality of life. With the right support system and a tailored treatment approach, those living with trichotillomania can find both relief and renewed hope on their path to recovery.
At A Glance
- Trichotillomania, also known as hair-pulling disorder, is a mental health condition marked by an uncontrollable urge to pull out one’s own hair.
- It commonly affects areas such as the scalp, eyebrows, and eyelashes, often leading to noticeable hair loss and emotional distress.
- Understanding what causes trichotillomania requires patience, empathy, and awareness of its psychological roots.
- For many, it functions as a coping mechanism for stress, anxiety, or emotional discomfort—making it difficult to stop without support.
- The disorder affects approximately 1–2% of the global population and can emerge at any age, though it often begins in childhood or adolescence.
- Effective treatment typically involves a combination of cognitive-behavioral therapy (CBT), medication, and self-help strategies.
- Coping approaches include identifying personal triggers, seeking professional guidance, and adopting stress-reduction techniques such as mindfulness or journaling.
Frequently Asked Questions (FAQs)
1. Is Trichotillomania A Coping Mechanism?
Trichotillomania can serve as a coping mechanism for some individuals to manage stress and emotional discomfort.
2. Is Trichotillomania Hard To Stop?
Trichotillomania can be challenging to stop due to the recurrent, compulsive nature of the behavior and the underlying emotional triggers.
3. Is Trichotillomania A Behavioural Addiction?
Trichotillomania is often considered a behavioral addiction, as it involves repetitive actions driven by psychological reinforcement.