Welcoming a new life into the world should be a joyous time, but for some, the experience can be overshadowed by Perinatal Mood and Anxiety Disorders (PMADs). PMADs are common and can impact both the mother’s and child’s health.
What Are PMADs?
Perinatal mood and anxiety disorders consist of mental health conditions experienced during and post-pregnancy. Perinatal depression and anxiety [mfn] McKee, K., Admon, L. K., Winkelman, T., Muzik, M., Hall, S., Dalton, V. K., & Zivin, K. (2020). Perinatal mood and anxiety disorders, serious mental illness, and delivery-related health outcomes, United States, 2006-2015. BMC women’s health, 20(1), 150. https://doi.org/10.1186/s12905-020-00996-6 [/mfn] are the most commonly occurring mental health problems in women after childbirth. A variety of symptoms are associated with these disorders, such as irritability, low mood, anger, constant worry, paranoia, delusions, etc.
Although a lot of women experience ‘baby blues’ that tend to go away with time, perinatal mental illness substantially impacts the daily life of the mother and causes significant distress.
If left untreated, it may lead to adverse outcomes for the mother as well as the baby. It is thus important to seek medical attention if a mother experiences emotional disturbances for more than two weeks after the delivery of a child.
According to the US Department of Health and Human Services (HHS [mfn] Office on Women’s Health. (2018, October 18). Postpartum depression. Womenshealth.gov. Available from: https://www.womenshealth.gov/mental-health/mental-health-conditions/postpartum-depression [/mfn]), almost 13% of new mothers experience depression during or after giving birth. Studies [mfn] McKee, K., Admon, L. K., Winkelman, T., Muzik, M., Hall, S., Dalton, V. K., & Zivin, K. (2020). Perinatal mood and anxiety disorders, serious mental illness, and delivery-related health outcomes, United States, 2006-2015. BMC women’s health, 20(1), 150. https://doi.org/10.1186/s12905-020-00996-6 [/mfn] have also found that the prevalence of Perinatal Mood and Anxiety Disorders increased from 18.4% to 40.4% between 2006-2007 and 2014-2015.
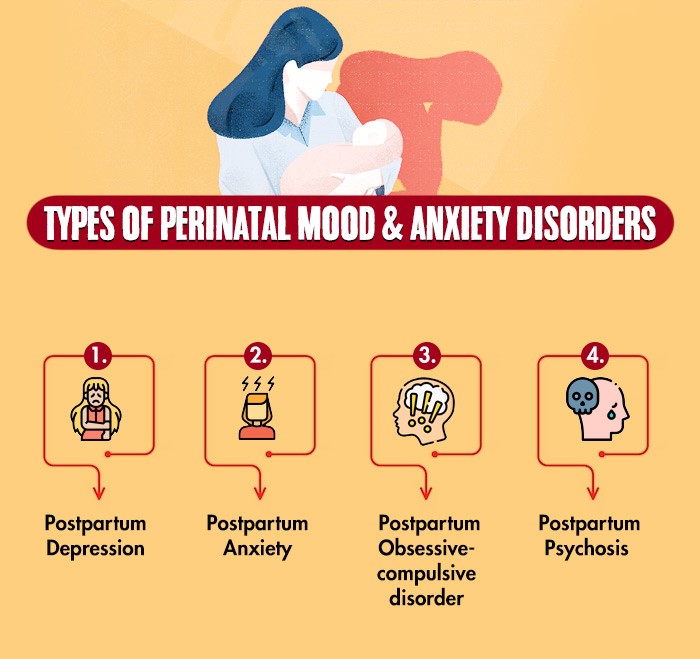
Types Of PMADs
PMADs may manifest in myriad ways. The symptoms of perinatal mood and anxiety disorders differ significantly depending on the type.
Let’s take a closer look at the different types of perinatal mood and anxiety disorders in women.
1. Perinatal/ Postpartum Depression
Postpartum depression is the most common psychological condition experienced by women after childbirth. It is characterized by symptoms such as:
- Persistent low mood or sadness
- Loss of interest or pleasure in previously pleasurable activities
- Lack of energy
- Difficulty concentrating
- Appetite or sleep problems
- Feelings of guilt, worthlessness, etc.
Continue Reading About Postpartum Depression Here
2. Perinatal/ Postpartum Anxiety
While it is quite usual for new mothers to experience anxiety after giving birth, postpartum anxiety disorder is a more severe condition that interferes with their daily functioning to a significant extent.
Reports [mfn] Depression in pregnant women and mothers: How children are affected. (2004). Paediatrics & child health, 9(8), 584–601. https://doi.org/10.1093/pch/9.8.584 [/mfn] suggest that 1 in every 10 women goes through postpartum anxiety after giving birth and 6% of women tend to experience it while pregnant. The symptoms of this condition include:
- Constant worry and anticipation
- Disturbance of sleep and appetite
- Dizziness
- Heart palpitations
- Nausea
- Shortness of breath
- Chest pain
If unaddressed, postpartum anxiety can severely affect the mother-child relationship [mfn] Goodman, J. H., Watson, G. R., & Stubbs, B. (2016). Anxiety disorders in postpartum women: A systematic review and meta-analysis. Journal of affective disorders, 203, 292–331. https://doi.org/10.1016/j.jad.2016.05.033 [/mfn].
Know More About Anxiety Disorders Here
3. Perinatal/ Postpartum Obsessive Compulsive Disorder (OCD)
Sometimes, mothers may experience OCD after childbirth even despite having no previous diagnoses of anxiety disorders. A woman suffering from postpartum OCD usually experiences the following symptoms [mfn] Miller, E. S., Chu, C., Gollan, J., & Gossett, D. R. (2013). Obsessive-compulsive symptoms during the postpartum period. A prospective cohort. The Journal of reproductive medicine, 58(3-4), 115–122. [/mfn] within 12 months of giving birth:
- Persistent intrusive and repetitive thoughts, or mental images regarding the baby
- A sense of fear related to the obsessive thoughts
- Repetitive acts or compulsions such as constantly cleaning, checking things, or counting and reordering things
- Fear of being left alone with the child
- Hypervigilance related to protecting the infant
It is important to keep in mind that mothers with this condition understand the nature of their thoughts and are quite disturbed by them.
Read More About OCD Here
4. Postpartum Psychosis
Postpartum psychosis involves delusions or hallucinations that are usually related to the child. This condition, however, is rare, affecting only 0.1 to 0.2% [mfn] VanderKruik, R., Barreix, M., Chou, D., Allen, T., Say, L., Cohen, L. S., & Maternal Morbidity Working Group (2017). The global prevalence of postpartum psychosis: a systematic review. BMC psychiatry, 17(1), 272. https://doi.org/10.1186/s12888-017-1427-7 [/mfn] of women. The symptoms of postpartum psychosis include:
- Delusions or strange beliefs that are not real
- Hallucinations or seeing or hearing things that are not there
- Feeling disconnected from reality
- Decreased need for or inability to sleep
- Paranoia and suspiciousness, etc.
Continue Reading About Postpartum Psychosis Here
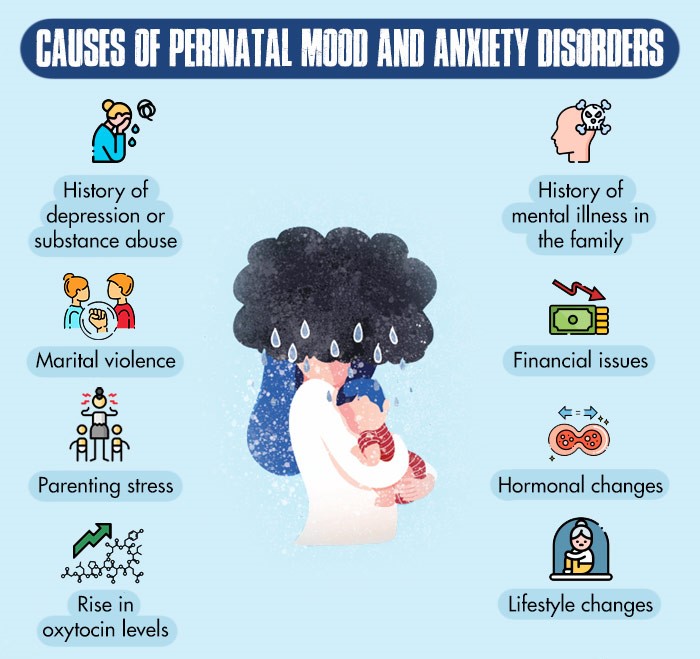
Causes Of PMADs
Several factors can lead to the development of perinatal mood and anxiety disorders in women.
Some of the common risk factors for PMADs are:
- History of depression [mfn] Lee, D. T., Yip, A. S., Leung, T. Y., & Chung, T. K. (2000). Identifying women at risk of postnatal depression: prospective longitudinal study. Hong Kong medical journal = Xianggang yi xue za zhi, 6(4), 349–354. [/mfn] or substance abuse
- Family history [mfn] Mathisen, S. E., Glavin, K., Lien, L., & Lagerløv, P. (2013). Prevalence and risk factors for postpartum depressive symptoms in Argentina: a cross-sectional study. International journal of women’s health, 5, 787–793. https://doi.org/10.2147/IJWH.S51436 [/mfn] of mental illness
- Inadequate support [mfn] Landman-Peeters, K. M., Hartman, C. A., van der Pompe, G., den Boer, J. A., Minderaa, R. B., & Ormel, J. (2005). Gender differences in the relation between social support, problems in parent-offspring communication, and depression and anxiety. Social science & medicine (1982), 60(11), 2549–2559. https://doi.org/10.1016/j.socscimed.2004.10.024 [/mfn] from family and friends
- Problems in previous pregnancies [mfn] Gaillard, A., Le Strat, Y., Mandelbrot, L., Keïta, H., & Dubertret, C. (2014). Predictors of postpartum depression: prospective study of 264 women followed during pregnancy and postpartum. Psychiatry research, 215(2), 341–346. https://doi.org/10.1016/j.psychres.2013.10.003 [/mfn]
- Marital [mfn] Ludermir, A. B., Lewis, G., Valongueiro, S. A., de Araújo, T. V., & Araya, R. (2010). Violence against women by their intimate partner during pregnancy and postnatal depression: a prospective cohort study. Lancet (London, England), 376(9744), 903–910. https://doi.org/10.1016/S0140-6736(10)60887-2 [/mfn] violence
- Financial [mfn] Miyake, Y., Tanaka, K., Sasaki, S., & Hirota, Y. (2011). Employment, income, and education and risk of postpartum depression: the Osaka Maternal and Child Health Study. Journal of affective disorders, 130(1-2), 133–137. https://doi.org/10.1016/j.jad.2010.10.024 [/mfn] problems
- Becoming a mother at a young age [mfn] Silva, R., Jansen, K., Souza, L., Quevedo, L., Barbosa, L., Moraes, I., Horta, B., & Pinheiro, R. (2012). Sociodemographic risk factors of perinatal depression: a cohort study in the public health care system. Revista brasileira de psiquiatria (Sao Paulo, Brazil : 1999), 34(2), 143–148. https://doi.org/10.1590/s1516-44462012000200005 [/mfn]
- Parenting stress [mfn] Leigh, B., & Milgrom, J. (2008). Risk factors for antenatal depression, postnatal depression and parenting stress. BMC psychiatry, 8, 24. https://doi.org/10.1186/1471-244X-8-24 [/mfn]
- Hormonal changes [mfn] Aishwarya, S., Rajendiren, S., Kattimani, S., Dhiman, P., Haritha, S., & Ananthanarayanan, P. H. (2013). Homocysteine and serotonin: association with postpartum depression. Asian journal of psychiatry, 6(6), 473–477. https://doi.org/10.1016/j.ajp.2013.05.007 [/mfn] during pregnancy
- High oxytocin levels [mfn] Neumann, I. D., & Landgraf, R. (2012). Balance of brain oxytocin and vasopressin: implications for anxiety, depression, and social behaviors. Trends in neurosciences, 35(11), 649–659. https://doi.org/10.1016/j.tins.2012.08.004 [/mfn] mid-pregnancy
- Lifestyle changes [mfn] Chatzi, L., Melaki, V., Sarri, K., Apostolaki, I., Roumeliotaki, T., Georgiou, V., Vassilaki, M., Koutis, A., Bitsios, P., & Kogevinas, M. (2011). Dietary patterns during pregnancy and the risk of postpartum depression: the mother-child ‘Rhea’ cohort in Crete, Greece. Public health nutrition, 14(9), 1663–1670. https://doi.org/10.1017/S1368980010003629 [/mfn] that involve changes in diet, sleep cycle, or exercise routines
Treatment For PMADs
Perinatal mood and anxiety disorders can be treated with a combination of therapy and medications. According to a 2007 study [mfn] Misri, S., & Kendrick, K. (2007). Treatment of perinatal mood and anxiety disorders: a review. Canadian journal of psychiatry. Revue canadienne de psychiatrie, 52(8), 489–498. https://doi.org/10.1177/070674370705200803 [/mfn], psychotherapeutic and pharmacological treatment can both offer “positive and negative outcomes” for PMADs and no treatment option is considered to be entirely free of risks.
Some of the most effective treatment options for perinatal mood and anxiety disorders have been discussed below:
1. Therapy
The common psychotherapies that are used for the treatment of PMADs are:
A. Cognitive Behavioral Therapy (CBT)
CBT has helped treat numerous patients with anxiety and mood disorders. A hybrid treatment [mfn] Sarid, O., Cwikel, J., Czamanski-Cohen, J., & Huss, E. (2017). Treating women with perinatal mood and anxiety disorders (PMADs) with a hybrid cognitive behavioural and art therapy treatment (CB-ART). Archives of women’s mental health, 20(1), 229–231. https://doi.org/10.1007/s00737-016-0668-7 [/mfn] consisting of cognitive behavioral and art therapy techniques was found to be quite beneficial for PMADs. Cognitive behavioral therapy can be conducted in groups as well as individually.
Continue Reading About CBT Here
B. Interpersonal Psychotherapy (IPT)
IPT is based on the idea that interpersonal and life events impact mood and vice versa. Its goal is to help people improve communication skills within relationships, develop social support, and set realistic expectations. This allows them to deal with the issues that may be contributing to their condition.
A 2014 study [mfn] Stuart S. (2012). Interpersonal psychotherapy for postpartum depression. Clinical psychology & psychotherapy, 19(2), 134–140. https://doi.org/10.1002/cpp.1778 [/mfn] reported that patients with major depression in primary care preferred interpersonal psychotherapy over antidepressant medication. IPT is a commonly used [mfn] Schiller, C.E., Thompson, K., Cohen, M.J., Geiger, P., Lundegard, L., Bonacquisti, A. (2021). Psychotherapy for Perinatal Mood and Anxiety Disorders. In: Cox, E. (eds) Women’s Mood Disorders. Springer, Cham. https://doi.org/10.1007/978-3-030-71497-0_17 [/mfn] therapeutic technique, especially for postpartum depression.
C. Dialectical Behavior Therapy (DBT)
DBT is a well-established therapeutic method for treating depression and anxiety. Several DBT skills such as mindfulness, emotion regulation, and distress tolerance have been incorporated in treating perinatal mood and anxiety disorders [mfn] Nunnery, R., Fauser, M., Hatchuel, E., & Jones, M. (2021). The Use of Dialectical Behavioral Therapy (DBT) Techniques Creatively in the Treatment of Perinatal Mood and Anxiety Disorders. Journal of Counseling Research and Practice, 6(2). https://doi.org/10.56702/UCKX8598/jcrp0602.3 [/mfn].
D. Other Therapies
Certain other therapy techniques [mfn] Schiller, C.E., Thompson, K., Cohen, M.J., Geiger, P., Lundegard, L., Bonacquisti, A. (2021). Psychotherapy for Perinatal Mood and Anxiety Disorders. In: Cox, E. (eds) Women’s Mood Disorders. Springer, Cham. https://doi.org/10.1007/978-3-030-71497-0_17 [/mfn] can also be used to treat perinatal mood and anxiety disorders. For example,
- Acceptance and commitment therapy (ACT)
- Couples’ therapy
- Mindfulness-based therapy, etc.
2. Medications
Women with perinatal mood and anxiety disorders are often prescribed [mfn] Brooks, E., Cox, E., Kimmel, M., Meltzer-Brody, S., Ruminjo, A. (2021). Risk of Medication Exposures in Pregnancy and Lactation. In: Cox, E. (eds) Women’s Mood Disorders. Springer, Cham. https://doi.org/10.1007/978-3-030-71497-0_6 [/mfn]:
- Antidepressants, such as SSRIs and SNRIs
- Anti-anxiety medication, such as benzodiazepines
- Mood stabilizers, such as lithium
- Antipsychotics
However, a doctor should always be consulted before taking any psychotropic medication as several of them might have adverse side effects.
Coping Tips For PMADs
The support of friends and family and your significant other can go a long way in easing the symptoms of perinatal mood and anxiety disorders. If you find yourself struggling with PMAD, here are some self-help techniques that may help you:
- Asking someone to care for the baby while you sleep
- Exercising or going for a walk daily
- Eating balanced and nutritious meals every day
- Talking about your feelings with your partner or a friend
- Giving yourself permission to do less and let others help you
- Practicing self-care and hygiene
Are men affected by Perinatal Mood and Anxiety Disorders?
Although men are less affected than women by PMADs, they are still at risk of developing them. Men’s hormones fluctuate when their female partner is pregnant and even after they have given birth. Men with family histories of disorders, genetic risks, and previous diagnoses of mood disorders are more likely to develop such conditions. Some of the symptoms that men may experience are:
- Irritability
- Indecision
- Impulsivity
- Violent behavior
- Avoidance behavior
Research [mfn] Scarff J. R. (2019). Postpartum Depression in Men. Innovations in clinical neuroscience, 16(5-6), 11–14. [/mfn] on men experiencing these mental disorders is still in progress. However, studies [mfn] About Postpartum Depression (PPD) | Mass.gov. (n.d.). Www.mass.gov. Retrieved October 17, 2022, from https://www.mass.gov/service-details/about-postpartum-depression-ppd [/mfn] have found that 1 in 10 new fathers develop some form of PMAD.
Men are less likely to seek professional help to cope with their emotional problems though. Research [mfn] Branquinho, M., Canavarro, M. C., & Fonseca, A. (2019). Knowledge and attitudes about postpartum depression in the Portuguese general population. Midwifery, 77, 86–94. https://doi.org/10.1016/j.midw.2019.06.016 [/mfn] shows that there is also a lower intention to recommend professional help to men for postpartum depression as compared to women.
Takeaway
After childbirth, women experience a drop in their hormonal levels which can cause a huge rush of emotions associated with mood and anxiety. It is important to offer emotional assistance to the mother to ensure a successful recovery. With therapy and medication, it is possible to recover from perinatal mood and anxiety disorders.
At A Glance
- Perinatal mood and anxiety disorders (PMADs) are mental disorders that occur during pregnancy or after childbirth.
- Some of its types include postpartum depression, postpartum anxiety, postpartum OCD, and postpartum psychosis.
- PMADs can develop due to a variety of factors such as a family history of mental illness, hormonal changes, rise in oxytocin levels, financial issues, etc.
- PMADs can be treated using therapeutic techniques like CBT, IPT, DBT, etc.
- Medications such as antidepressants, benzodiazepines, and antipsychotics can also be used to treat PMADs.
- Some ways to cope with PMADs include eating balanced meals, exercising regularly, and sharing your feelings with loved ones.







Leave a Reply