Addiction is a chronic mental health condition in which a person misuses and becomes dependent on a substance or non-substance, despite harmful consequences.
[wpb_childpages parent_page_id=”2206″ post_type=”topic” post_status=”publish” sort_pages=”post_name” title=”Subtopics” style=”#topicNav{height: 350px;}”]
What Is Addiction?
Addiction involves a physical and psychological dependence or compulsion to engage in certain unhealthy behaviors through consuming substances.
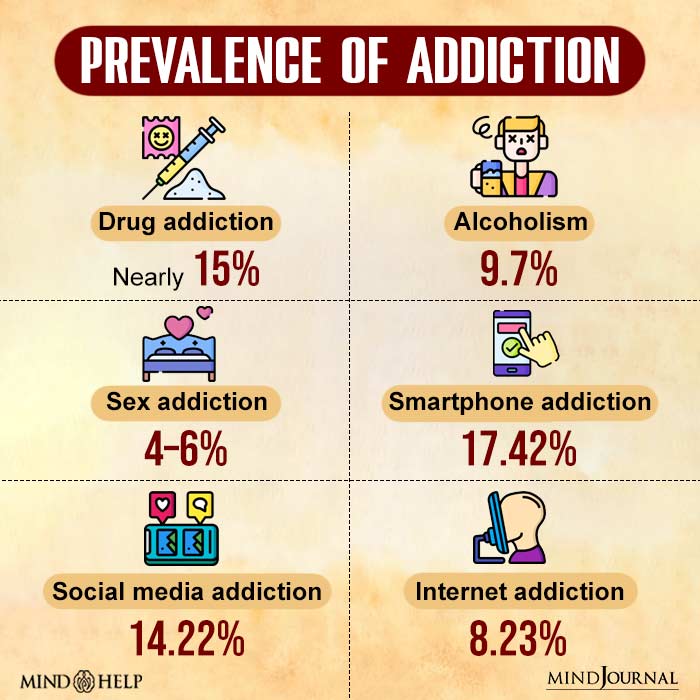
It can develop in response to a variety of substances or behaviors (such as drugs, alcohol, gambling, or internet use). It is one of the most chronic relapsing mental health conditions 1 Uhl, G. R., Koob, G. F., & Cable, J. (2019). The neurobiology of addiction. Annals of the New York Academy of Sciences, 1451(1), 5–28. https://doi.org/10.1111/nyas.13989 , besides depression and schizophrenia. It is usually characterized by:
- Craving or a strong desire or urge to use a substance or engage in such behavior.
- Loss of control over the use of a substance or engaging in a type of behavior
- Tolerance for the regular use of harmful substances
- Withdrawal or the development of physical or psychological symptoms when attempting to quit the use of a substance or behavior
- Disregarding negative consequences linked to the addiction like health problems, financial difficulties, or relationship problems
Is Addiction A disorder?
Addiction is a clinical syndrome marked by a compulsive need for and use of a habit-forming substance as well as periods of recovery and symptom recurrence (relapse).
It is accepted as a mental illness in the diagnostic nomenclature, clinically referred to as substance use disorder (SUD) 2 National Institute of Mental Health. (2021). Substance use and co-occurring mental disorders. National Institute of Mental Health. Available from: https://www.nimh.nih.gov/health/topics/substance-use-and-mental-health . It generally involves a plethora of cognitive, behavioral, and conduct disorders that result in substantial health, social, and economic problems

Signs Of Addiction
Studies 3 Koob, G. F., & Volkow, N. D. (2016). Neurobiology of addiction: a neurocircuitry analysis. The lancet. Psychiatry, 3(8), 760–773. https://doi.org/10.1016/S2215-0366(16)00104-8 attribute the common symptoms of addiction to the following:
- Use of harmful substances that trigger cognitive and behavioral changes
- Seeking substance or behavior despite adverse physical or psychological effects
- Uncontrollable craving for such substances
- Frequently engaging in risky or damaging behaviors
- Constantly being preoccupied with addictive substances or behavior
- Maintaining secrecy or hiding substances from others
- Experiencing mood fluctuations and denial
- Unsuccessful attempts at consuming harmful substances
- Changes in personality
- Difficulty identifying or regulating emotions
- Changes in appetite and weight
- Sleep disturbances or insomnia
- Memory loss
- Increased sensitivity
- Physiological withdrawal symptoms 4 Piper M. E. (2015). Withdrawal: Expanding a Key Addiction Construct. Nicotine & tobacco research : official journal of the Society for Research on Nicotine and Tobacco, 17(12), 1405–1415. https://doi.org/10.1093/ntr/ntv048
Misuse Vs Addiction
Misuse and addiction are two related but distinct concepts 5 Leyton M. (2013). Are addictions diseases or choices?. Journal of psychiatry & neuroscience : JPN, 38(4), 219–221. https://doi.org/10.1503/jpn.130097 related to substance use. Misuse refers to using a substance inappropriately (at high doses or in inappropriate situations), whereas addiction is a complex and chronic condition 6 McLellan A. T. (2017). Substance Misuse and Substance use Disorders: Why do they Matter in Healthcare?. Transactions of the American Clinical and Climatological Association, 128, 112–130. characterized by compulsive substance seeking and use despite negative consequences.
Misuse 7 US Department of Health and Human Services. (2016, November). THE NEUROBIOLOGY OF SUBSTANCE USE, MISUSE, AND ADDICTION. Nih.gov; US Department of Health and Human Services. Available from: https://www.ncbi.nlm.nih.gov/books/NBK424849/ can occur due to a variety of reasons like forgetfulness or lack of knowledge, but addiction is a clinically recognized behavioral disorder mandating professional treatment.
Misuse can lead to negative consequences, such as health problems, relationship issues, and legal or financial troubles. However, not everyone who misuses a substance or behavior will develop an addiction.
Types Of Addiction
The common types 8 Gould T. J. (2010). Addiction and cognition. Addiction science & clinical practice, 5(2), 4–14. of addiction include:
1. Substance use disorders
Substance addiction or substance use disorder (SUD) 9 Fatayer, J. (2008). Addiction Types: A Clinical Sociology Perspective. Journal of Applied Social Science, 2(1), 88–93. https://doi.org/10.1177/193672440800200107 is the persistent and obsessive use of substances (like alcohol and drugs) that cause mental, physical, and behavioral problems. The substances commonly used for addiction include:
- Alcohol
- Cannabis
- Phencyclidine
- Opioids
- Tobacco
- Sedatives
- Cannabis
- Stimulant drugs like cocaine, ecstasy, etc.
2. Non-substance addiction
Non-substance addiction involves indulging in certain unhealthy behaviors. These behaviors are common in people with impulse control disorders 10 Schmitz, J. M. (2005). The Interface Between Impulse-Control Disorders and Addictions: Are Pleasure Pathway Responses Shared Neurobiological Substrates? Sexual Addiction & Compulsivity, 12(2-3), 149–168. https://doi.org/10.1080/10720160500203641 or who experience chronic difficulty in resisting the temptation of certain impulsive behaviors. It is also known as behavioral addiction 11 Grant, J. E., Potenza, M. N., Weinstein, A., & Gorelick, D. A. (2010). Introduction to behavioral addictions. The American journal of drug and alcohol abuse, 36(5), 233–241. https://doi.org/10.3109/00952990.2010.491884 to things like:
- The Internet
- Food
- Sex
- Pornography
- Technology use
- Working
- Exercising
- Spiritual obsession
- Self-harm
- Pain-seeking
- Video games
- Intermittent explosive disorder (IED)
- Kleptomania or compulsive stealing
- Pyromania or compulsive setting of fires
- Gambling
- Compulsive buying
- Chronic hoarding
Read More About Types Of Addiction Here
Stages Of Addiction
Addiction is a complex individualized experience 12 Volkow, N. D., Koob, G. F., & McLellan, A. T. (2016). Neurobiologic Advances from the Brain Disease Model of Addiction. The New England journal of medicine, 374(4), 363–371. https://doi.org/10.1056/NEJMra1511480 . However, an addict usually goes through the following 5 stages 13 Uhl, G. R., Koob, G. F., & Cable, J. (2019). The neurobiology of addiction. Annals of the New York Academy of Sciences, 1451(1), 5–28. https://doi.org/10.1111/nyas.13989 of addiction:
- First use
- Regular use/Continued use
- Risky use/Tolerance
- Dependence
- Addiction/Substance use disorder
Initially, a potential addict tries a substance or non-substance for the first time, experimenting in different contexts to see how it affects his/her life. Over time, its use becomes normalized on a regular basis, often as a way to cope with stress or other problems.
This is followed by a risky misuse/tolerance of the substance or non-substance which negatively impacts his/her personal and professional lives and social relationships.
Gradually the person develops a physical and/or psychological dependence on the abused substance or non-substance and consequently develops a clinical condition of addiction.
Read More About Stages Of Addiction Here
Causes of addiction
Research 14 Herman, M. A., & Roberto, M. (2015). The addicted brain: understanding the neurophysiological mechanisms of addictive disorders. Frontiers in integrative neuroscience, 9, 18. https://doi.org/10.3389/fnint.2015.00018 attributes the common causes of addiction to the following factors 15 National Institute on Drug Abuse. (2020). Drug Misuse and Addiction. National Institute on Drug Abuse. Available from: https://nida.nih.gov/publications/drugs-brains-behavior-science-addiction/drug-misuse-addiction :
- Genetics
- Chemical imbalances in the brain
- A family history of addiction
- Peer pressure
- Ready availability of addictive substances and non-substances
- Childhood trauma and maltreatment
- Parental abuse, neglect, and abandonment
- Negative life experiences like poverty, war, invasion, etc.
- A family history of mental health disorders (like depression, anxiety, etc.)
Read More About Causes Of Addiction Here
Complications Associated With Addiction
Addiction, when left unaddressed or untreated, can cause certain serious long-term complications 16 National Institute of Mental Health. (2021). Substance use and co-occurring mental disorders. National Institute of Mental Health. Available from: https://www.nimh.nih.gov/health/topics/substance-use-and-mental-health , such as:
- Physical health problems related to cardiovascular diseases, liver disease, brain injury, mortality, etc.
- Enhanced symptoms of comorbid mental health conditions like depression, anxiety, etc.
- Impaired daily functioning linked to decreased productivity, absenteeism, or job loss.
- Relationship issues 17 Lander, L., Howsare, J., & Byrne, M. (2013). The impact of substance use disorders on families and children: from theory to practice. Social work in public health, 28(3-4), 194–205. https://doi.org/10.1080/19371918.2013.759005 like broken intimate relationships, reduced social interaction, self-imposed isolation, etc.
- Legal problems associated with financial insecurity, arrest and incarceration, etc.
- Risk of overdose, suicidality, and accidental death.
Read More About Complications Of Addiction Here
How Does Addiction Affect The Brain?
Addiction is a complex and chronic mental health disorder that affects the brain 18 Institute of Medicine (US) Committee on Opportunities in Drug Abuse Research. (1996). Pathways of Addiction: Opportunities in Drug Abuse Research. In PubMed. National Academies Press (US). Available from: https://www.ncbi.nlm.nih.gov/books/NBK232975/ and can lead to changes in behavior, mood, and cognition. Substance addiction and misuse of certain non-substances can create functional and structural changes in the brain, specifically brain areas that regulate mood, pleasure, and reward.
Read More About Addiction And The Brain Here
How does addiction affect mental health?
Addiction also impairs cognitive function, leading to maladaptive behavior, memory impairment, poor decision-making skills, and chronic irritability. Research 19 Information, N. C. for B., Pike, U. S. N. L. of M. 8600 R., MD, B., & Usa, 20894. (2013). MENTAL HEALTH AND SUBSTANCE USE DISORDERS: TREATMENT LANDSCAPE. In www.ncbi.nlm.nih.gov. Substance Abuse and Mental Health Services Administration (US). Available from: https://www.ncbi.nlm.nih.gov/books/NBK174675/ also closely links addictive behavior to the onset of mental health disorders like:
- Mood disorders like depression, bipolar disorder, etc.
- Anxiety, particularly social anxiety
- Schizoaffective disorders
- Personality disorders
- Eating disorders
- Sleep disorders
- Stress and trauma disorders like PTSD, etc.
- Psychosis
- Psychopathy
- Self-harm
- Suicidality
Diagnosis Of Addiction
Addiction diagnosis 20 Heilig, M., MacKillop, J., Martinez, D., Rehm, J., Leggio, L., & Vanderschuren, L. J. M. J. (2021). Addiction as a brain disease revised: why it still matters, and the need for consilience. Neuropsychopharmacology : official publication of the American College of Neuropsychopharmacology, 46(10), 1715–1723. https://doi.org/10.1038/s41386-020-00950-y is carried out based on the medical evaluation of physical and behavioral symptoms, according to the Diagnostic and Statistical Manual of Mental Disorders (DSM-5). A person must show two or more characteristics of addictive behavior over at least a period of 12 months to be diagnosed.
A general physician carries out a physical examination of the affected person. This may involve blood tests, urine tests, or other diagnostic tests to assess the individual’s overall health and to rule out any underlying medical conditions.
Based on the results, the patient is referred to a mental health professional (MHP). The MHP assesses his/her symptoms of addiction (like cravings, withdrawal signs, etc.) as well as risk factors (such as stressful life events, a family history of addiction, and so forth).
The four C’s of addiction 21 Koob, G. F., & Volkow, N. D. (2016). Neurobiology of addiction: a neurocircuitry analysis. The lancet. Psychiatry, 3(8), 760–773. https://doi.org/10.1016/S2215-0366(16)00104-8 (compulsion, cravings, consequences, and control) is a common clinical tool used to distinguish addiction from other mental health disorders with similar symptoms. The evaluation determines the specifics of the patient’s treatment plan.
Treatment Of addiction
The treatment of addiction typically involves a comprehensive, individualized approach that combines several medical, behavioral, and psychological interventions 22 Inanlou, M., Bahmani, B., Farhoudian, A., & Rafiee, F. (2020). Addiction Recovery: A Systematized Review. Iranian journal of psychiatry, 15(2), 172–181. . The first step involves detoxification or the process of removing the substance from the body while managing withdrawal symptoms. This is followed up with:
1. Counseling and behavioral therapies
Therapies like cognitive-behavioral therapy (CBT) and multidimensional family therapy help the addicted to modify their behavior and develop coping skills to prevent relapse.
Additionally, motivational interviewing 23 Bischof, G., Bischof, A., & Rumpf, H. J. (2021). Motivational Interviewing: An Evidence-Based Approach for Use in Medical Practice. Deutsches Arzteblatt international, 118(7), 109–115. https://doi.org/10.3238/arztebl.m2021.0014 and contingency management 24 Higgins, S. T., & Petry, N. M. (1999). Contingency management. Incentives for sobriety. Alcohol research & health : the journal of the National Institute on Alcohol Abuse and Alcoholism, 23(2), 122–127. can help people with addiction maximize their willingness to change and make adjustments to their behaviors.
2. Rehabilitation programs
Support group interventions 25 Center for Substance Abuse Treatment. (2013). 2 Types of Groups Commonly Used in Substance Abuse Treatment. Nih.gov; Substance Abuse and Mental Health Services Administration (US). Available from: https://www.ncbi.nlm.nih.gov/books/NBK64214/ in in-patient and out-patient facilities provide a safe and supportive environment for individuals to share their experiences, receive encouragement, and connect with others who are also in the process of recovery.
3. Pharmacotherapy
Medication 26 Douaihy, A. B., Kelly, T. M., & Sullivan, C. (2013). Medications for substance use disorders. Social work in public health, 28(3-4), 264–278. https://doi.org/10.1080/19371918.2013.759031 supplements therapies to help manage cravings and withdrawal symptoms associated with addiction, as well as block the effects of certain drugs. However, the type of pharmacotherapy administered can vary depending on the specific substance or behavior being abused and the severity of the addiction.
4. Non-pharmacological treatment methods
The treatment of addiction is often a long-term process and has high scores of relapse. Because of this, the recovery process is made better and surer by availing holistic therapy approaches 27 Breslin, K. T., Reed, M. R., & Malone, S. B. (2003). An holistic approach to substance abuse treatment. Journal of psychoactive drugs, 35(2), 247–251. https://doi.org/10.1080/02791072.2003.10400006 (such as yoga, meditation, and acupuncture).
These equip individuals with addiction to manage stress well and improve their overall well-being. However, recovery from addiction is a lifelong process 28 Junyue, J., Siyu, C., Xindong, W., Qinge, X., Jingchun, Z., Liming, L., & Guohua, L. (2021). Complementary and Alternative Medicine for Substance Use Disorders: A Scientometric Analysis and Visualization of Its Use Between 2001 and 2020. Frontiers in psychiatry, 12, 722240. https://doi.org/10.3389/fpsyt.2021.722240 that requires ongoing commitment, support, and hard work.
Recovery And Coping With Addiction
Coping with an addiction involves developing new coping skills and strategies to manage cravings, avoid triggers, and prevent relapse. Consider the following tips to manage your addiction treatment and recovery 29 Laudet, A. B., Savage, R., & Mahmood, D. (2002). Pathways to long-term recovery: a preliminary investigation. Journal of psychoactive drugs, 34(3), 305–311. https://doi.org/10.1080/02791072.2002.10399968 better:
- Consult a healthcare provider or a specialist in addiction to manage your symptoms of addiction.
- If needed, consider taking support from addiction rehabilitation.
- Closely stick to the treatment plan. This includes attending therapy sessions, following medication plans, and participating in support groups.
- Identify the people, places, or situations that may trigger cravings or lead to relapse.
- Develop healthy coping strategies that aid you during treatment, recovery, or emergencies.
- Practice self-care by getting quality sleep, eating a healthy diet, and engaging in activities that bring you joy and fulfillment.
- Build a strong support system and communicate openly. This may include family, friends, healthcare providers, or support groups.
Takeaway
Addictions can be extremely crippling. Ensure that you get timely support for addiction treatment and address its symptoms and consequences. Also, remember that the path of recovery and personal care isn’t a straight line, so don’t let discouragement take over when you struggle.
At A Glance
- Addiction is a mental health condition wherein a person compulsively uses a substance or engages in harmful behavior.
- It is one of the most chronic relapsing mental health conditions.
- It is a brain dysfunction that affects our memory, motivation, attitudes, and reward system of the brain.
- The chief symptom involves repeated use of a substance or compulsive engagement in a particular habit-forming activity that impairs daily functioning.
- Addiction can be treated with several therapies, medication, and self-help strategies.
Frequently Asked Questions (FAQs)
1. What is the most serious form of addiction?
Heroin addiction is the most serious form of addiction.
2. What are the “Four C’s” of addiction?
The “Four C’s of addiction are compulsion, cravings, consequences, and control.
3. How addictive is sugar?
Sugar is a substance that releases opioids and dopamine and impacts our brain pathways and reward systems. It is a potentially addictive substance for people with food addictions and obesity.
4. Are addictions genetic?
Studies affirm that there is a genetic predisposition to substance use addiction and chronic alcoholism.
5. What is the most critical risk factor in addiction?
A family history of addiction and lack of family involvement comprises the most critical risk factor in addiction.
6. Is addiction a disease?
Addiction is a complex disease of the brain and body that involves the compulsive use of one or more substances, at the cost of serious health consequences. It is clinically referred to as substance use disorder (SUD).
7. Can you become addicted to a person?
While the concept of being “addicted” to a person is common, it does not exist. Certain people may experience intense emotional attachment or dependence on a specific person. Such unhealthy attachment patterns do not qualify for full-blown mental health conditions and are symptoms of underlying mental health conditions like social anxiety, dependent personality disorder (DPD), etc.