Addiction is a chronic mental health condition marked by the physical and psychological dependence on certain substances or the compulsion to engage in certain unhealthy behaviors—despite adverse consequences. However, unlike other mental illnesses, there are no specific causes of addiction.
Complex and multi-faceted “addictive conditions” progress and develop over time, most often due to several genetic and psychosocial factors. However, for most addicts, it starts out as an experimentation out of peer pressure or curiosity, while for others, it can be a coping mechanism to deal with stress and mental distress.
What Are The Causes Of Addiction?
Research 1 Justinova, Z., Panlilio, L. V., & Goldberg, S. R. (2009). Drug addiction. Current topics in behavioral neurosciences, 1, 309–346. https://doi.org/10.1007/978-3-540-88955-7_13 attributes the causes of addiction to substances or non-substances to a combination of biological, environmental, and spiritual factors. The main causes of addiction include:
I. Biological causes of addiction
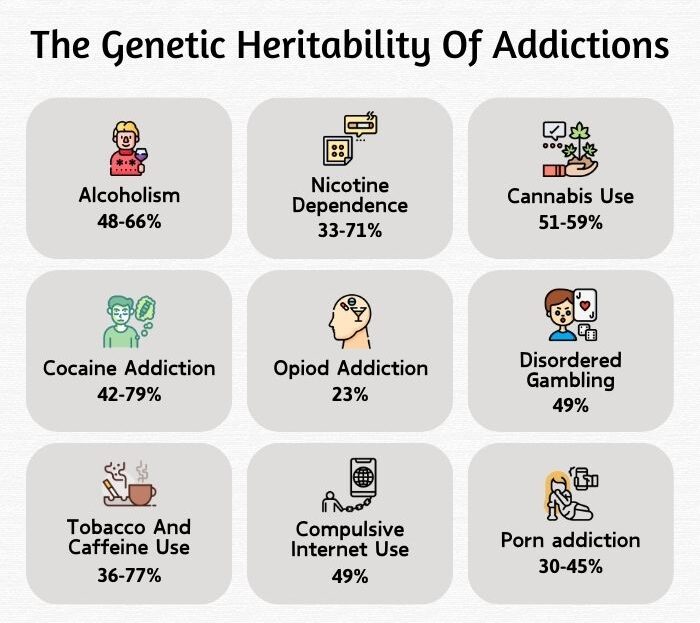
Genetics is regarded as a major influencing factor in addiction. Addiction can run in the family, as a person with a parent, sibling, or first-degree relative who is a substance or behavioral addict is at a greater risk of developing a similar addiction. Twin studies 2 Deak, J. D., & Johnson, E. C. (2021). Genetics of substance use disorders: a review. Psychological medicine, 51(13), 2189–2200. https://doi.org/10.1017/S0033291721000969 particularly reveal that often both twins tend to be addicted due to similar or identical genetics.
This is because substance addiction and misuse of certain non-substances create functional and structural changes in the brain, specifically brain areas that regulate mood, pleasure, and reward.
These changes modify behavior, mood and cognition, response to stress, reward-seeking behavior, and impulsivity. Such characteristics get transmitted, either through genetic heritability or through learned behavior due to psychosocial orientation.
In some cases, traumatic brain injury can create dysfunctional brain pathways and chemical imbalances 3 Erickson, C. K., & Wilcox, R. E. (2001). Neurobiological Causes of Addiction. Journal of Social Work Practice in the Addictions, 1(3), 7–22. https://doi.org/10.1300/j160v01n03_02 that cause addiction.
II. Psychological causes of addiction
People with a family history of mental health conditions 4 Grant, J. E., & Chamberlain, S. R. (2020). Family history of substance use disorders: Significance for mental health in young adults who gamble. Journal of behavioral addictions, 9(2), 289–297. https://doi.org/10.1556/2006.2020.00017 are more vulnerable to developing an addiction. Substance use disorder (SUD) or chronic dependence on non-substances can also be attributed to low self-esteem, poor psychological resilience, maladaptive coping strategies, and undiagnosed mental health conditions 5 National Institutes on Drug Abuse. (2020). Common Comorbidities with Substance Use Disorders Research Report. In PubMed. National Institutes on Drug Abuse (US). Available from: https://www.ncbi.nlm.nih.gov/books/NBK571451/ , such as:
- Depression
- Bipolar disorders
- Stress disorders
- Untreated trauma
- Anxiety disorder
- Eating disorders
- Gambling disorder
- Grief, etc.
III. Social causes of addiction
The social and environmental factors in addiction include a combination of several negative life experiences resulting from:
1. Parental neglect and abuse
People with experiences of parental abuse, neglect, and abandonment are prone to substance use. A lack of parental discipline, supervision, or control while growing up can also be a contributing factor.
Particularly children from families with an addicted or absent parent 6 Eslami-Shahrbabaki, A., Eslami-Shahrbabaki, M., & Kalantari, M. (2013). Association between Parental Addiction and Types of Child Abuse in High-School Students of Kerman, Iran. Addiction & health, 5(3-4), 108–114. tend to display behavioral and cognitive disturbances (like emotional dysfunction, violence, conflict, unhealthy attachment patterns, role reversal, trust issues, etc.) and they may resort to substance use as a maladaptive coping mechanism.
2. Childhood abuse
Children who grow up in a dysfunctional or toxic family environment are at a greater risk of addiction. This is because they are frequently exposed to adverse childhood experiences (ACEs) 7 Elmore, A. L., & Crouch, E. (2020). The Association of Adverse Childhood Experiences With Anxiety and Depression for Children and Youth, 8 to 17 Years of Age. Academic pediatrics, 20(5), 600–608. https://doi.org/10.1016/j.acap.2020.02.012 linked to domestic violence, financial insecurity, damaged support systems, maltreatment, as well as physical, emotional, and sexual abuse.
They develop a shame for moral and interpersonal failure 8 Flanagan O. (2013). The shame of addiction. Frontiers in psychiatry, 4, 120. https://doi.org/10.3389/fpsyt.2013.00120 and can take to substance use to cope with their unpleasant realities and family stress.
3. Peer pressure
Peer rejection, low self-worth, and social withdrawal can lead a person toward substance use. Inversely, peer use of substances and peer pressure can also be contributing factors to addiction.
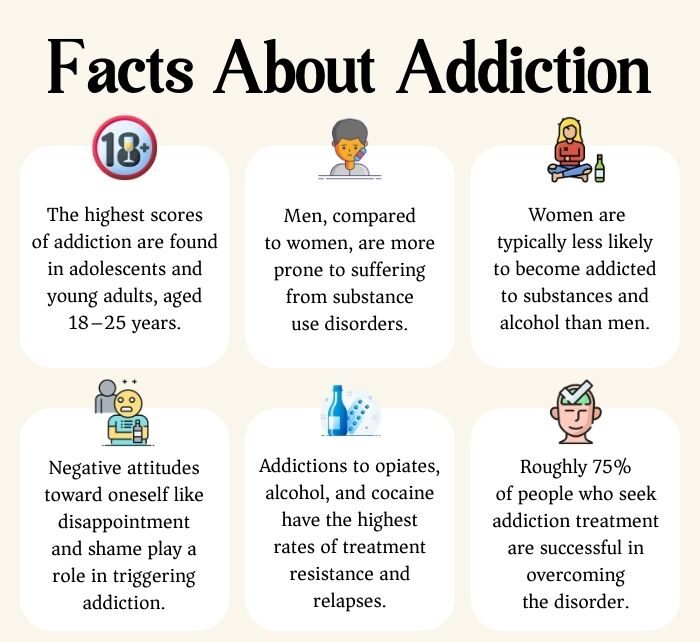
Social demands 9 Keyzers, A., Lee, S. K., & Dworkin, J. (2020). Peer Pressure and Substance Use in Emerging Adulthood: A Latent Profile Analysis. Substance use & misuse, 55(10), 1716–1723. https://doi.org/10.1080/10826084.2020.1759642 like the need to fit in and avoid unpopularity can make a person susceptible to the influence of friends, peers, and acquaintances, particularly in adolescence and early adulthood.
In the process, non-users can be persuaded to try out and experiment with substances and non-substances, sometimes against their better judgment. Studies 10 Keyzers, A., Lee, S. K., & Dworkin, J. (2020). Peer Pressure and Substance Use in Emerging Adulthood: A Latent Profile Analysis. Substance use & misuse, 55(10), 1716–1723. https://doi.org/10.1080/10826084.2020.1759642 , over the years, have affirmed that peer pressure encourages the use of addictive substances and harmful behavior in adolescents, making them vulnerable to health risks in adulthood.
4. The ready availability of substances
The easy availability of substances 11 Hadland, S. E., Marshall, B. D., Kerr, T., Lai, C., Montaner, J. S., & Wood, E. (2012). Ready access to illicit drugs among youth and adult users. The American journal on addictions, 21(5), 488–490. https://doi.org/10.1111/j.1521-0391.2012.00257.x in the community, neighborhood, home, or at school is a significant environmental factor that causes addiction. When an individual is repeatedly exposed to the use of intoxicating substances, alcohol, or tobacco, he/she feels encouraged to experiment with them, eventually becoming regular users.
Several studies 12 Substance Abuse and Mental Health Services Administration (US, & Office of the Surgeon General (US. (2016, November). HEALTH CARE SYSTEMS AND SUBSTANCE USE DISORDERS. Nih.gov; US Department of Health and Human Services. Available from: https://www.ncbi.nlm.nih.gov/books/NBK424848/ show that people with long-term chronic physical illnesses can also develop a disposition toward drug misuse.
Caregivers dealing with the physical and psychological burden of diseases and ready accessibility to medication are prone to addiction. Moreover, living in communities engrossed in poverty and/or criminality can also trigger addiction.
5. Detrimental life events
Negative life experiences involving displacement, invasion, war, and natural calamities can also be contributing factors in addiction development. Studies 13 Agyapong, B., Shalaby, R., Eboreime, E., Obuobi-Donkor, G., Owusu, E., Adu, M. K., Mao, W., Oluwasina, F., & Agyapong, V. I. O. (2022). Cumulative trauma from multiple natural disasters increases mental health burden on residents of Fort McMurray. European journal of psychotraumatology, 13(1), 2059999. https://doi.org/10.1080/20008198.2022.2059999 , for instance, show that refugees with post-traumatic stress disorder (PTSD) are prone to developing substance use disorder (SUD).
IV. Spiritual causes of addiction
Research 14 Grant Weinandy, J. T., & Grubbs, J. B. (2021). Religious and spiritual beliefs and attitudes towards addiction and addiction treatment: A scoping review. Addictive behaviors reports, 14, 100393. https://doi.org/10.1016/j.abrep.2021.100393 opines that a spiritual disconnection or emptiness and a lack of piety can also cause addiction. People experiencing such a void often resort to substance use as an attempt to gain a transcendental state (A mood/teparamental state which is beyond common, mundane/ordinary experiences).
They are prone to experimenting with such intoxicants till the misuse of the same is no longer recreational or medical, but rather a reliant substance of choice.
Certain world religions and cultural systems 15 Somasundaram, O., Raghavan, D. V., & Murthy, A. G. (2016). Drinking habits in ancient India. Indian journal of psychiatry, 58(1), 93–96. https://doi.org/10.4103/0019-5545.174396 also include the use of addictive substances in their social practices and religious rituals. Hinduism, for example, allows the ritualized use of cannabis 16 Morningstar P. J. (1985). Thandai and chilam: traditional Hindu beliefs about the proper uses of Cannabis. Journal of psychoactive drugs, 17(3), 141–165. https://doi.org/10.1080/02791072.1985.10472336 to facilitate concentration, relaxation, and social cohesion in the evening or on holidays.
While the occasional social use of drugs does not guarantee the development of addiction, it does open avenues for introduction to and experimentation with certain addictive substances.
Read More About Addiction Here
Risk Factors Of Addiction
The common 17 Morales, A. M., Jones, S. A., Kliamovich, D., Harman, G., & Nagel, B. J. (2020). Identifying Early Risk Factors for Addiction Later in Life: A Review of Prospective Longitudinal Studies. Current addiction reports, 7(1), 89–98. https://doi.org/10.1007/s40429-019-00282-y risk factors that cause addiction include:
- Early, often untimely use of addictive substances and non-substances
- A family history of addiction
- Child abuse and lack of family involvement during growing up
- Undiagnosed mental health disorder
- Peer rejection
- Peer use of substances and pressure to do the same
- Negative environmental factors like poverty, invasion, war, etc.
Outcomes And Interventions
The treatment of addiction typically involves a comprehensive, individualized approach that combines several medical, behavioral, and psychological interventions.
The most common intervention in addiction treatment comprises psychosocial interventions 18 Jhanjee S. (2014). Evidence based psychosocial interventions in substance use. Indian journal of psychological medicine, 36(2), 112–118. https://doi.org/10.4103/0253-7176.130960 that can be administered in a variety of treatment settings either as stand-alone treatments or in combination with pharmacotherapy.
The first step involves detoxification or the process of removing the substance from the body while managing withdrawal symptoms. This is followed up with behavioral therapies like cognitive-behavioral therapy (CBT) that help the addicted modify their behavior and develop coping skills to prevent relapse.
In many cases, medication supplements therapies 19 Forray, A., & Sofuoglu, M. (2014). Future pharmacological treatments for substance use disorders. British journal of clinical pharmacology, 77(2), 382–400. https://doi.org/10.1111/j.1365-2125.2012.04474.x to help manage cravings and withdrawal symptoms associated with addiction.
The treatment of addiction is often a long-term process and has high scores of relapse 20 Menon, J., & Kandasamy, A. (2018). Relapse prevention. Indian journal of psychiatry, 60(Suppl 4), S473–S478. https://doi.org/10.4103/psychiatry.IndianJPsychiatry_36_18 . Because of this, the recovery process is made better and surer by availing support group interventions and holistic therapy approaches 21 Junyue, J., Siyu, C., Xindong, W., Qinge, X., Jingchun, Z., Liming, L., & Guohua, L. (2021). Complementary and Alternative Medicine for Substance Use Disorders: A Scientometric Analysis and Visualization of Its Use Between 2001 and 2020. Frontiers in psychiatry, 12, 722240. https://doi.org/10.3389/fpsyt.2021.722240 (such as yoga, meditation, and acupuncture).
These equip individuals with addiction to manage stress well and improve their overall well-being. However, recovery from addiction is a lifelong process that requires ongoing commitment, support, and hard work.
Takeaway
Addiction is a debilitating condition but it can be treated effectively under the guidance of a medical professional. So if you or a loved one is suffering from this condition, make sure to consult a doctor and seek professional help immediately.
With therapy and medication, one can overcome the symptoms and live a healthier and more stable life. Understanding the causes can help the doctor or therapist devise a more accurate and customized treatment plan for better and faster recovery.
At A Glance
- There are multiple causes of addiction involving biological and psychosocial factors.
- The biological causes largely entail genetic heritability and physical and mental health conditions.
- The social causes of addiction include parental neglect, childhood abuse, peer pressure, the ready availability of addictive substances, etc.
- Addiction can also be caused by religious or spiritual practices.
- A timely and proper diagnosis of addiction can help manage its symptoms and curb its long-term negative consequences.
Frequently Asked Questions (FAQs)
1. What is the main predictor of addiction?
Starting the use of alcohol, nicotine or other substance use at an early age is the main predictor of addiction.
2. What are the risk factors for using drugs?
Poverty, experiences of parental and childhood abuse, undiagnosed mental health problems, ready drug availability, and peer rejection or heavy drug use are common risk factors for drug use.
3. Is age a risk factor for substance abuse?
Changing social and physical circumstances could increase vulnerability to substance abuse as we age.
4. What age group is most likely to become addicted?
Among all age groups, young adults aged 18 to 25 have the highest addiction rate. Many adults may not address their addiction until they reach their 30s or 40s.















