Autism is a complex developmental disability that significantly impacts an individual’s ability to communicate, behave, and interact with others. The severity of symptoms and related challenges can vary greatly among individuals affected by autism.
What Is Autism Spectrum Disorder?
Autism is a neurodevelopmental disorder that affects a person’s behavior, communication abilities, and social interaction.
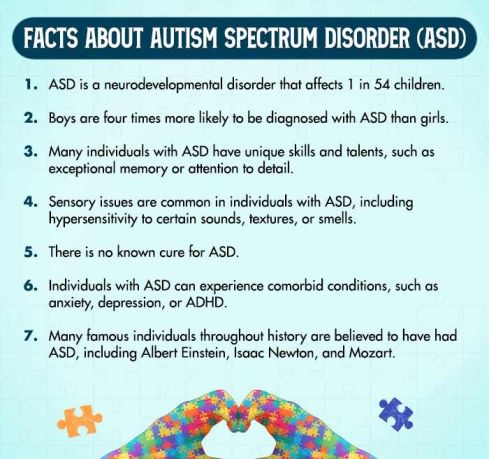
It is also known as autism spectrum disorder (ASD), as it is a complex and multifaceted disorder that can impact individuals differently and to varying degrees. It stands recognized 1 Wiggins, L. D., Rice, C. E., Barger, B., Soke, G. N., Lee, L. C., Moody, E., Edmondson-Pretzel, R., & Levy, S. E. (2019). DSM-5 criteria for autism spectrum disorder maximizes diagnostic sensitivity and specificity in preschool children. Social psychiatry and psychiatric epidemiology, 54(6), 693–701. https://doi.org/10.1007/s00127-019-01674-1 in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5).
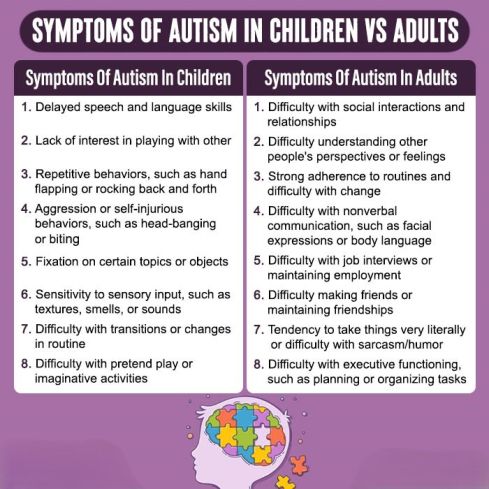
Autism can occur in both children and adults, albeit with different sets of symptoms that mandate different diagnosis and treatment.
Some individuals with ASD may have relatively mild symptoms and be able to live independently, while others may have more severe symptoms and require significant support and assistance throughout their lives. This complexity and variability can make it challenging to address the long-term impact of autism.
Prevalence of autism
Autism can be detected as early as 6-18 months of age 2 Lordan, R., Storni, C., & De Benedictis, C. A. (2021). Autism Spectrum Disorders: Diagnosis and Treatment (A. M. Grabrucker, Ed.). PubMed; Exon Publications. Available from: https://www.ncbi.nlm.nih.gov/books/NBK573609/ . An experienced professional can make a reliable diagnosis of the early signs of autism by age 2. However, many children are not diagnosed until much later in life.
Research, nonetheless, estimates that, worldwide, 1 in 100 children has autism 3 Salari, N., Rasoulpoor, S., Rasoulpoor, S., Shohaimi, S., Jafarpour, S., Abdoli, N., Khaledi-Paveh, B., & Mohammadi, M. (2022). The global prevalence of autism spectrum disorder: a comprehensive systematic review and meta-analysis. Italian Journal of Pediatrics, 48(1). https://doi.org/10.1186/s13052-022-01310-w . Around 2.22% of adults, worldwide 4 Dietz, P. M., Rose, C. E., McArthur, D., & Maenner, M. (2020). National and State Estimates of Adults with Autism Spectrum Disorder. Journal of autism and developmental disorders, 50(12), 4258–4266. https://doi.org/10.1007/s10803-020-04494-4 , also suffer from autism. The prevalence of autism has increased over the past few decades, which is partially attributed to changes in diagnostic criteria and increased awareness of the disorder.
Case Example
James, a 10-year-old boy, has been experiencing challenges in communication, struggling to understand others’ messages and social cues for the past 6 months. He also becomes hypersensitive to sound, light, touch, and other external sensations, and shows strong emotional outbursts when facing a situation similar to this.
His parents noticed that James is not communicating in a typical way, avoiding eye contact, not responding to greetings, and lacking interest in social interactions.
James also exhibits rigid interests, continues to play with the same object even when it breaks down, and likes to wear the same color every day even when the dress is not clean. He also struggles to adapt to school, unable to follow instructions and make friends with his classmates.
Case Analysis
Based on this case, it can be observed that James experiences significant difficulties in reciprocal communication and mutual interaction, exhibits rigid, restricted interests, high sensitivity to specific stimuli, challenges in understanding emotions, and non-verbal behaviors, and difficulty in establishing social relationships. All of these behaviors indicate that James has significant signs of Autism Spectrum Disorder.
Symptoms Of Autism Spectrum Disorder (ASD)
The symptoms of autism in adults and children differ. However, certain symptoms 5 Boat, T. F., Wu, J. T., to, C., Board, Board, Institute of Medicine, and, B., & The. (2015, October 28). Clinical Characteristics of Autism Spectrum Disorder. Nih.gov; National Academies Press (US). Available from: https://www.ncbi.nlm.nih.gov/books/NBK332891/ are central to the disorder, such as:
- Difficulties with social interaction and communication, such as difficulty with eye contact, facial expressions, and body language
- Repetitive behaviors or interests, such as lining up toys, repeating words or phrases, or having a strong attachment to certain objects
- Difficulty with changes in routine or environment
- Sensory sensitivities, such as being overly sensitive or under-sensitive to certain sounds, textures, or smells
- Difficulty with motor skills, such as delays in crawling, walking, or running
Types Of Autism Spectrum Disorder (ASD)
The different types 6 Masi, A., DeMayo, M. M., Glozier, N., & Guastella, A. J. (2017). An Overview of Autism Spectrum Disorder, Heterogeneity and Treatment Options. Neuroscience bulletin, 33(2), 183–193. https://doi.org/10.1007/s12264-017-0100-y of ASD are classified based on their symptoms and characteristics. These include:
1. Autistic disorder (Classic autism)
This is the most well-known and severe form of ASD. It is characterized by significant impairments in communication, social interaction, and behavior, as well as the presence of stereotyped or repetitive behaviors.
2. Asperger’s syndrome (AS)
This is the most well-known and severe form of ASD. It is characterized by significant impairments in communication, social interaction, and behavior, as well as the presence of stereotyped or repetitive behaviors.
However, people with AS are said to have “high-functioning autism”, because of which they do not have the severe language or cognitive impairments that characterize people with autism.
Read More About Asperger’s Syndrome Here
3. Pervasive developmental disorder – not otherwise specified (PDD-NOS)
This type of ASD is used to describe individuals who have significant impairments in social interaction and communication, but who do not meet the full criteria for classic autism or Asperger’s syndrome.
4. Rett syndrome
This is a rare genetic disorder that affects females. It is characterized by a loss of cognitive and social skills, as well as the presence of stereotyped hand movements.
5. Childhood disintegrative disorder (CDD)
This is a rare type of ASD in which children appear to develop normally for the first few years of life, but then experience a significant loss of skills and abilities in multiple areas, including social interaction, communication, and behavior.
Autism And Mental Health
Autism and mental health are intricately connected 7 Lai, A. G., Chang, W. H., & Skuse, D. (2022). Autism and mental illness in children and young people require standardised approaches for assessment and treatment. The Lancet regional health. Europe, 16, 100360. https://doi.org/10.1016/j.lanepe.2022.100360 , with one often influencing the other. Individuals with ASD can experience a range of mental health challenges, including anxiety, depression, and ADHD. Conversely, the symptoms and impairments associated with ASD can also impact mental health and well-being.
The symptoms and impairments associated with ASD can also impact mental health and well-being, including social isolation, sensory overload, difficulty with emotional regulation, and difficulty with transitions.
Individuals with ASD are at a higher risk for developing co-occurring mental health conditions 8 Mosner, M. G., Kinard, J. L., Shah, J. S., McWeeny, S., Greene, R. K., Lowery, S. C., Mazefsky, C. A., & Dichter, G. S. (2019). Rates of Co-occurring Psychiatric Disorders in Autism Spectrum Disorder Using the Mini International Neuropsychiatric Interview. Journal of autism and developmental disorders, 49(9), 3819–3832. https://doi.org/10.1007/s10803-019-04090-1 than the general population. These mental health disorders include:
- Anxiety [Read more]
- Depression [Read more]
- Attention Deficit Hyperactivity Disorder (ADHD) [Read more]
- Obsessive-Compulsive Disorder (OCD) [Read more]
- Eating disorders [Read more]
- Sleep disorders [Read more]
What Causes Autism?
Research 9 Almandil, N. B., Alkuroud, D. N., AbdulAzeez, S., AlSulaiman, A., Elaissari, A., & Borgio, J. F. (2019). Environmental and Genetic Factors in Autism Spectrum Disorders: Special Emphasis on Data from Arabian Studies. International journal of environmental research and public health, 16(4), 658. https://doi.org/10.3390/ijerph16040658 attributes the common causes of autism to the following factors:
1. Genetics
Autism is believed to have a strong genetic component 10 Rylaarsdam, L., & Guemez-Gamboa, A. (2019). Genetic causes and modifiers of autism spectrum disorder. Frontiers in Cellular Neuroscience, 13(13). https://doi.org/10.3389/fncel.2019.00385 , with research indicating that the condition may be inherited from family members who have a similar condition. Changes in gene expression can also be a prominent risk factor for ASD.
2. Brain development
Autism may be linked to differences or disruptions in the development of the brain, specifically in the areas of communication, social interaction, and sensory processing (like amygdala and insula).
3. Environmental factors
Certain environmental factors, such as exposure to toxins during pregnancy or complications during childbirth, may increase the risk of developing autism spectrum disorder. Specifically, prenatal and perinatal factors 11 Kolevzon, A., Gross, R., & Reichenberg, A. (2007). Prenatal and perinatal risk factors for autism: a review and integration of findings. Archives of pediatrics & adolescent medicine, 161(4), 326–333. https://doi.org/10.1001/archpedi.161.4.326 (such as maternal stress and addiction to substances or complications during childbirth) constitute predominant risk factors in its development.
4. Neurological differences
Individuals with autism may have neurological differences (linked to brain volume and symmetry) in the way their brains process information. This can affect their social and communication skills.
5. Other medical conditions
ASD has been linked to other medical conditions, such as epilepsy, gastrointestinal disorders, and immune system disorders. While these conditions are not direct causes, they may contribute to the development or severity of symptoms.
How Is Autism Diagnosed?
Early diagnosis 12 Webb, S. J., & Jones, E. J. (2009). Early Identification of Autism: Early Characteristics, Onset of Symptoms, and Diagnostic Stability. Infants and young children, 22(2), 100–118. https://doi.org/10.1097/IYC.0b013e3181a02f7f and intervention are crucial for improving treatment outcomes for individuals with ASD. The diagnosis of autism spectrum disorder (ASD) involves a comprehensive evaluation by a healthcare professional specializing in autism treatment.
It includes screening for developmental delays, evaluation of communication skills, social interaction, and behavior. Diagnostic criteria for ASD 13 Lordan, R., Storni, C., & De Benedictis, C. A. (2021). Autism Spectrum Disorders: Diagnosis and Treatment (A. M. Grabrucker, Ed.). PubMed; Exon Publications. Available From: https://www.ncbi.nlm.nih.gov/books/NBK573609/#:~:text=According%20to%20DSM%2D5%2C%20to are outlined in DSM-5 and an individual must meet specific criteria related to social communication and interaction and restricted, repetitive patterns of behavior.
There are also various diagnostic tools available for ASD 14 Lordan, R., Storni, C., & De Benedictis, C. A. (2021). Autism Spectrum Disorders: Diagnosis and Treatment (A. M. Grabrucker, Ed.). PubMed; Exon Publications. https://www.ncbi.nlm.nih.gov/books/NBK573609/ , including the Autism Diagnostic Interview-Revised (ADI-R), the Autism Diagnostic Observation Schedule (ADOS), and the Childhood Autism Rating Scale (CARS).
These tools can help to provide a more standardized and objective assessment of an individual’s symptoms and behaviors and can assist in making an accurate diagnosis of ASD.
Autism Treatment
Autism treatment methods typically involve a combination of therapies and interventions 15 Faras, H., Al Ateeqi, N., & Tidmarsh, L. (2010). Autism spectrum disorders. Annals of Saudi medicine, 30(4), 295–300. https://doi.org/10.4103/0256-4947.65261 tailored to the individual’s specific needs. These include:
1. Behavioral therapies
Behavioral therapies, such as Applied Behavior Analysis (ABA), can help individuals with ASD improve their communication, social interaction, and behavior.
2. Speech and language therapy
Speech and language therapy can help individuals with ASD improve their communication skills and ability to express themselves.
3. Occupational therapy
Occupational therapy can help individuals with ASD develop the skills needed for daily living, such as dressing, eating, and grooming.
4. Sensory integration therapy
Sensory integration therapy can help individuals with ASD improve their ability to process and respond to sensory input.
5. Medication
Medication 16 Turner M. (2020). The role of drugs in the treatment of autism. Australian prescriber, 43(6), 185–190. https://doi.org/10.18773/austprescr.2020.054 may be used to treat co-occurring conditions, such as anxiety or ADHD, that can often accompany ASD.
Coping With Symptoms Of Autism As Adults
Consider the following tips 17 Muniandy, M., Richdale, A. L., Arnold, S. R. C., Trollor, J. N., & Lawson, L. P. (2022). Associations between coping strategies and mental health outcomes in autistic adults. Autism research : official journal of the International Society for Autism Research, 15(5), 929–944. https://doi.org/10.1002/aur.2694 for coping with autism spectrum disorder:
- Seek professional diagnosis and treatment to address the symptoms of autism spectrum disorder.
- Educate yourself on autism spectrum disorder through reputable sources.
- Build a support network of family, friends, and healthcare professionals.
- Consider developing coping strategies and social skills.
- Establish a daily routine for stability and predictability.
- Avoid triggers that may worsen symptoms.
- Practice self-care techniques 18 Ghanouni, P., & Quirke, S. (2023). Resilience and Coping Strategies in Adults with Autism Spectrum Disorder. Journal of autism and developmental disorders, 53(1), 456–467. https://doi.org/10.1007/s10803-022-05436-y to manage stress and promote well-being.
- Identify and utilize your strengths and interests.
- Connect with support groups or online communities.
- Advocate for your needs and raise awareness of autism spectrum disorder.
Coping Strategies For Caregivers Of Children With Autism
Consider the following tips 19 ALBusaidi, A. M. S., ALMasroori, S. A. S., Awladthani, B. M. S., ALKhaldi, S. A., Al Alawi, N., & Al Salmani, A. A. (2022). Quality of life and coping strategies used by parents of children with autism spectrum disorder in Oman. Autism & developmental language impairments, 7, 23969415221142262. https://doi.org/10.1177/23969415221142262 to develop healthy coping strategies as caregivers handling ASD in children:
- Educate yourself and research into autism to better understand the children’s condition and identify effective coping strategies.
- Work with a therapist to develop behavioral strategies that can help manage difficult behaviors and promote positive interactions.
- Avail family therapy to better relationships between the affected and his/her family members.
- Use clear and direct communication—breaking down tasks into manageable steps and using visual aids to support understanding.
- Provide “training” opportunities for socialization—modeling appropriate social behavior, and using role-playing exercises to help children practice social skills.
- Take breaks when needed by seeking support 20 Catalano, D., Holloway, L., & Mpofu, E. (2018). Mental Health Interventions for Parent Carers of Children with Autistic Spectrum Disorder: Practice Guidelines from a Critical Interpretive Synthesis (CIS) Systematic Review. International journal of environmental research and public health, 15(2), 341. https://doi.org/10.3390/ijerph15020341 from friends and family and taking care of your own physical and emotional health.
Takeaway
Autism spectrum disorder (ASD) is a complex group of disorders that can cause difficulties in communication, social interaction, and repetitive, restricted behaviors. Because the condition can manifest differently in each individual, it’s important to seek professional medical attention if you suspect your child may have ASD.
Effective therapies and medication can help manage symptoms, and enable your child to develop important life skills and live with more independence.
At A Glance
- Autism is a neurodevelopmental disorder that affects communication, social interaction, and behavior.
- It is recognized as a spectrum disorder.
- The symptoms of autism in adults and children include difficulty with social interaction and communication, repetitive behaviors, difficulty with changes in routine, sensory sensitivities, and difficulty with motor skills.
- Autism and mental health are intricately connected, with individuals with ASD experiencing a range of mental health challenges.
- The causes of ASD are believed to include genetics, brain development, environmental factors, neurological differences, and other medical conditions.
- Early diagnosis and intervention are crucial for improving autism treatment outcomes.
Frequently Asked Questions (FAQs)
1. Who are some famous people with autism?
Some famous people with autism include Temple Grandin, Dan Aykroyd, Daryl Hannah, Albert Einstein, Isaac Newton, and Mozart.
2. Is autism a disability?
Autism is considered a neurodevelopmental disorder, and for some individuals, it can be disabling, while for others, it may not significantly impact their daily lives.
3. How does autism start?
The early signs of autism start in childhood, usually due to a combination of genetic and environmental factors.