Chronic pain is a debilitating condition that extends beyond physical discomfort to profoundly impact emotional well-being. Understanding the diverse types of chronic pain is essential in comprehending their intricate connection to mental health.
Types Of Chronic Pain
Chronic pain generally refers to persistent discomfort 1 Dydyk, A. M., & Conermann, T. (2022). Chronic Pain. PubMed; StatPearls Publishing. Available from: https://www.ncbi.nlm.nih.gov/books/NBK553030/#:~:text=There%20are%20multiple%20categories%20and that lasts for an extended period, typically beyond the expected timeframe for healing or recovery. Unlike acute pain, which is a natural response to injury and generally subsides as the body heals, the types of chronic pain persist for weeks, months, or even years.
Chronic pain symptoms encompasses a diverse range of conditions, including arthritis, fibromyalgia, migraines, and lower back pain, to name a few. The enduring discomfort in different types of chronic pain often manifests as a persistent or recurring sensation characterized by aching, burning, stabbing, or throbbing.
Chronic Pain And Mental Health Disorders
The relationship between the different types of chronic pain and mental health is a complex and interwoven one 2 Crofford L. J. (2015). Chronic Pain: Where the Body Meets the Brain. Transactions of the American Clinical and Climatological Association, 126, 167–183. . Individuals who experience chronic pain often find themselves navigating not only the physical sensations but also the emotional and psychological toll it can take.
The relentless discomfort and limitations imposed by chronic pain can lead to a range of mental health challenges, including depression, anxiety, and reduced quality of life. Conversely, pre-existing mental health issues can also exacerbate the perception and management of chronic pain.
Read More About Depression Here
Different Types Of Chronic Pain
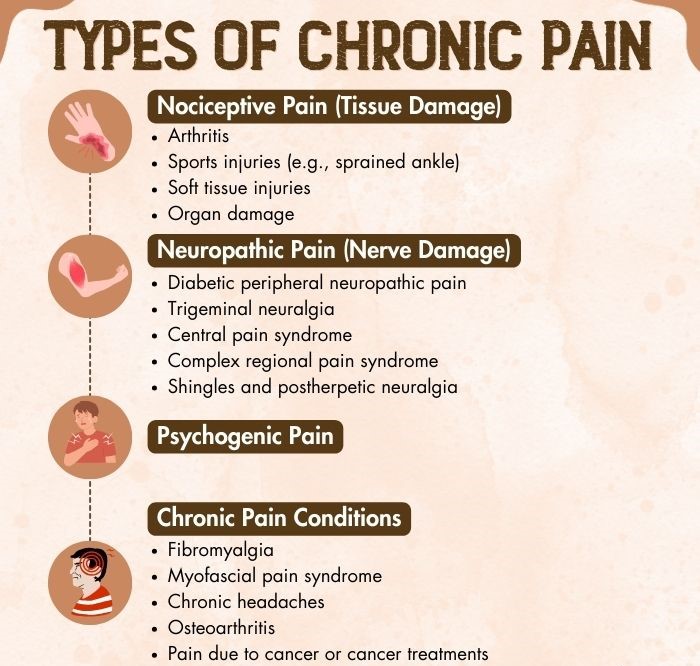
The basic classification of pain is acute (short-term) pain and chronic (long-term) pain. The different types of chronic pain are further classified into four types 3 Bonezzi, C., Fornasari, D., Cricelli, C., Magni, A., & Ventriglia, G. (2020). Not All Pain is Created Equal: Basic Definitions and Diagnostic Work-Up. Pain and therapy, 9(Suppl 1), 1–15. https://doi.org/10.1007/s40122-020-00217-w :
1. Nociceptive Pain (Tissue Damage)
This type of chronic pain is caused by injury or damage to specific body tissues 4 Armstrong, S. A., & Herr, M. J. (2022). Physiology, Nociception. PubMed; StatPearls Publishing. Available from: https://www.ncbi.nlm.nih.gov/books/NBK551562/#:~:text=%5B7%5D%5B8%5D%20Nociceptive (like bones, soft tissues, or organs). Examples include arthritis or sports injuries.
2. Neuropathic Pain (Nerve Damage)
The foremost of the types of chronic pain in mental health, neuropathic pain 5 Costigan, M., Scholz, J., & Woolf, C. J. (2009). Neuropathic pain: a maladaptive response of the nervous system to damage. Annual review of neuroscience, 32, 1–32. https://doi.org/10.1146/annurev.neuro.051508.135531 is caused by nerve damage that interferes with pain signal transmission. It is often described as burning, prickling, or electrical shock. Examples include:
- Diabetic Peripheral Neuropathic Pain: Chronic pain linked to diabetes, causing burning or stabbing sensations in extremities due to nerve damage.
- Trigeminal Neuralgia: Severe facial pain triggered by minimal stimulation along the trigeminal nerve.
- Central Pain Syndrome: Chronic pain from central nervous system damage, often due to stroke or multiple sclerosis, causing constant and widespread pain.
- Complex Regional Pain Syndrome (CRPS): Chronic pain syndrome following injury, with severe, burning pain and skin changes in the affected area.
- Shingles And Postherpetic Neuralgia: Painful conditions caused by the varicella-zoster virus, with shingles leading to rash and pain along nerve pathways, and postherpetic neuralgia resulting in chronic pain persisting after shingles.
3. Psychogenic Pain
Psychogenic pain is a complex form of chronic pain that can stem from physical sources but is strongly influenced by emotions and psychological states. Such a pain usually has a physical origin (such as tissue or nerve damage), but it is exacerbated and prolonged by emotional factors like fear, depression, stress, anxiety, addiction, etc. This type of pain highlights the intricate relationship between physical well-being and mental health.
4. Chronic Pain Conditions
Out of the different types of chronic pain, chronic pain conditions 6 Rama Yasaei, & Abdolreza Saadabadi. (2019, May 11). Chronic Pain Syndrome. Nih.gov; StatPearls Publishing. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470523/ originate from damage to the central nervous system. Examples include chronic headaches, fibromyalgia, Myofascial pain syndrome, osteoarthritis, among others.
Read More About Chronic Pain Here
Recovery From Chronic Pain
Recovery from the different types of chronic pain is a journey that varies depending on the type of chronic pain you are experiencing. The key to successful recovery from chronic pain lies in understanding the specific condition, seeking appropriate medical guidance 7 Center for Substance Abuse Treatment. (2019). Chronic Pain Management. Nih.gov; Substance Abuse and Mental Health Services Administration (US). Available from: https://www.ncbi.nlm.nih.gov/books/NBK92054/ , and implementing tailored treatment strategies 8 Mills, S. E. E., Nicolson, K. P., & Smith, B. H. (2019). Chronic pain: a review of its epidemiology and associated factors in population-based studies. British journal of anaesthesia, 123(2), e273–e283. https://doi.org/10.1016/j.bja.2019.03.023 .
Takeaway
Chronic pain, a prevalent challenge in physical health, often takes the spotlight in healthcare discussions. However, the parallel issue of different types of chronic pain in mental health is frequently overlooked, despite its profound impact. Unaddressed chronic pain in mental health can lead to a cascade of mental health consequences, including depression, anxiety, and reduced quality of life.
Consequently, recognizing and treating chronic pain in mental health is not only crucial for alleviating physical discomfort but also for preserving long-term mental well-being. It is imperative that healthcare providers and individuals acknowledge the interplay between physical and mental health and prioritize comprehensive pain management strategies to ensure recovery from chronic pain and holistic health.
At A Glance
- Chronic pain is persistent, long-lasting pain that typically lasts for at least three to six months.
- The different types of chronic pain can manifest in various forms.
- There are 4 types of chronic pain: Nociceptive, neuropathic, psychogenic, and chronic conditions.
- Understanding the diverse types of chronic pain is essential in comprehending their intricate connection to mental health.
- Recovery from chronic pain includes seeking appropriate medical guidance and implementing tailored treatment strategies.
Frequently Asked Questions (FAQs)
1. How Many Types Of Chronic Pain Are There?
There are 4 main types of chronic pain.
2. How Does Chronic Pain Differ In Physical And Mental Health?
Chronic pain can impact both physical and mental health, with physical symptoms causing discomfort and limitations while also contributing to emotional and psychological distress.
3. What Are The 4 A’s Of Chronic Pain?
The “4 A’s” of chronic pain management are Analgesia (pain relief), Activities of daily living (maintaining functionality), Adaptation (coping strategies), and Affect (addressing emotional aspects).
4. What Are The 6 D’s Of Chronic Pain?
The “6 D’s” of chronic pain assessment and management typically include Duration, Description, Development (how it started), Distribution (where it’s located), Disability (impact on daily life), and Distress (emotional and psychological aspects).