Dermatillomania is a mental health condition characterized by compulsive skin picking. It can profoundly impact an individual’s mental health, causing heightened anxiety, shame, and emotional distress.
What Is Dermatillomania?
Dermatillomania is a mental health condition (( Malayala, S. V., Rehman, H., & Vasireddy, D. (2021). Dermatillomania: A Case Report and Literature Review. Cureus, 13(1), e12932. https://doi.org/10.7759/cureus.12932 )) characterized by repetitive and compulsive picking at one’s own skin to the extent that it causes noticeable damage or distress. Dermatillomania symptoms typically go beyond normal grooming habits and can lead to skin injuries, scarring, and significant impairment in daily functioning.
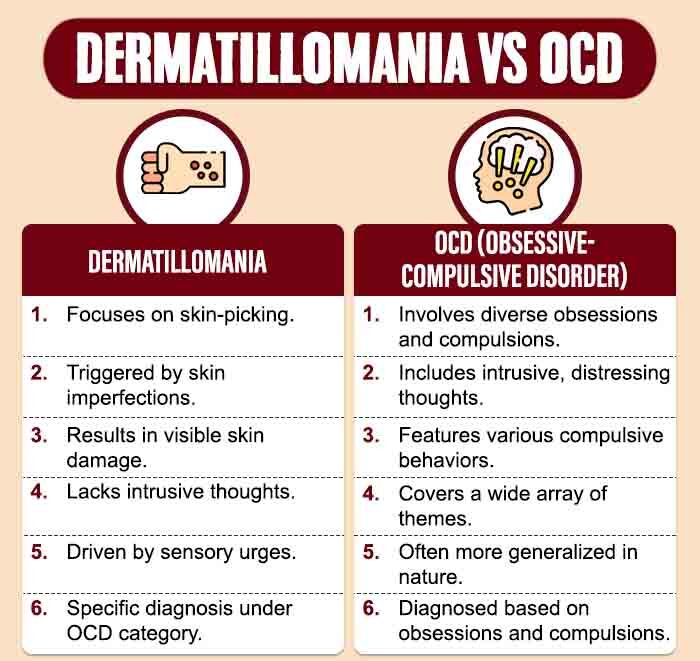
In the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (( Grant, J. E., & Chamberlain, S. R. (2020). Prevalence of skin picking (excoriation) disorder. Journal of psychiatric research, 130, 57–60. https://doi.org/10.1016/j.jpsychires.2020.06.033 )) (DSM-5), dermatillomania is classified under the category of obsessive-compulsive and related disorders. It is listed as excoriation (skin-picking) disorder and is characterized by recurrent skin picking that leads to skin lesions.
Dermatillomania In Films
Dermatillomania is rarely explored in films, save the critically lauded documentary Scars of Shame (2015). One notable movie is the coming-of-age movie Thirteen (2003), where the protagonist exhibits skin-picking behaviors as part of her overall teenage turmoil. In the indie movie Short Term 12 (2013), one of the characters struggles with self-harm and dermatillomania symptoms. The 2016 horror flick Are We Not Cats chronicles the romance between two individuals suffering from trichotillomania and dermatillomania.
Read More About Self-Harm Here
Prevalence Of Dermatillomania
Dermatillomania affects around 1-5% of the global population (( Grant, J. E., & Chamberlain, S. R. (2020). Prevalence of skin picking (excoriation) disorder. Journal of psychiatric research, 130, 57–60. https://doi.org/10.1016/j.jpsychires.2020.06.033 )) , though prevalence is not extensively documented. It can onset at any age but typically begins in adolescence or early adulthood. While it affects both genders, there might be a slight prevalence difference in favor of females (( Grant, J. E., & Chamberlain, S. R. (2022). Skin picking disorder: Does a person’s sex matter?. Annals of clinical psychiatry : official journal of the American Academy of Clinical Psychiatrists, 34(1), 15–20. https://doi.org/10.12788/acp.0049 )) . Prognosis varies, with some experiencing periods of improvement, while others may struggle long-term.
Symptoms Of Dermatillomania
The common dermatillomania symptoms include (( Lochner, C., Roos, A., & Stein, D. J. (2017). Excoriation (skin-picking) disorder: a systematic review of treatment options. Neuropsychiatric disease and treatment, 13, 1867–1872. https://doi.org/10.2147/NDT.S121138 )) :
- Repetitive skin picking
- Skin lesions, wounds, and scarring
- An irresistible urge to pick the skin
- Pre-picking tension and post-picking relief
- Excessive time spent on skin picking
- Failed attempts to stop
- Impairment in daily life and physical harm.
Types Of Dermatillomania Symptoms
Dermatillomania symptoms are typically not classified into different types like most other mental health conditions. However, it can manifest in various forms and severity levels (( Hawatmeh, A., & Al-Khateeb, A. (2017). An unusual complication of dermatillomania. Quantitative imaging in medicine and surgery, 7(1), 166–168. https://doi.org/10.21037/qims.2016.12.02 )) , with specific features or triggers varying from one individual to another:
1. Mild to severe:
The disorder can range in severity from mild, where skin picking is relatively manageable, to severe, where it leads to significant damage and impairment.
2. Focused areas:
Individuals may focus their skin picking on specific areas of the body, such as the face, arms, or legs.
3. Trigger-related:
Some people with dermatillomania may have specific triggers or situations that exacerbate their skin-picking behavior, such as stress, anxiety, or perceived imperfections in the skin.
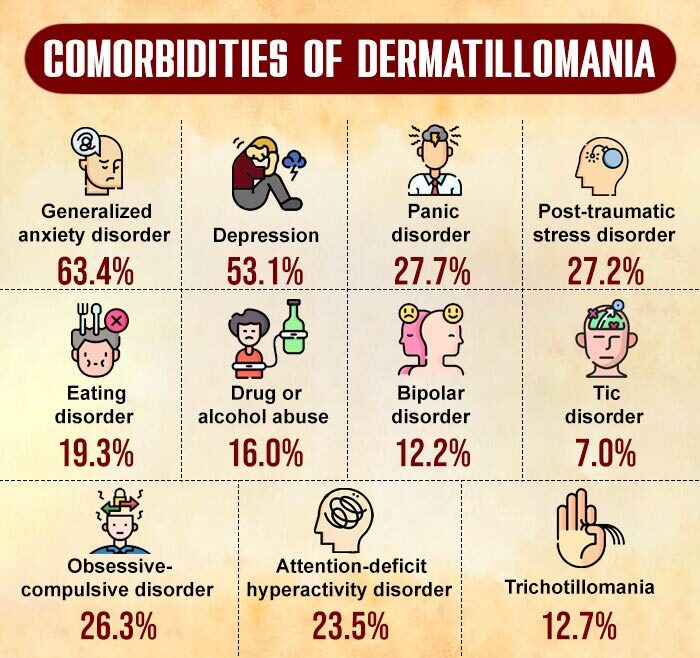
4. Comorbid conditions:
Dermatillomania symptoms can co-occur with other mental health conditions, (( Grant, J. E., & Chamberlain, S. R. (2021). Trichotillomania and Skin-Picking Disorder: An Update. Focus (American Psychiatric Publishing), 19(4), 405–412. https://doi.org/10.1176/appi.focus.20210013 )) such as obsessive-compulsive disorder (OCD), body dysmorphic disorder (BDD), or trichotillomania (hair-pulling disorder).
Read More About Trichotillomania Here
Causes Of Dermatillomania
The common causes (( Gallinat, C., Stürmlinger, L. L., Schaber, S., & Bauer, S. (2021). Pathological Skin Picking: Phenomenology and Associations With Emotions, Self-Esteem, Body Image, and Subjective Physical Well-Being. Frontiers in psychiatry, 12, 732717. https://doi.org/10.3389/fpsyt.2021.732717 )) for developing dermatillomania symptoms include:
- Genetics
- A family history of OCD or related disorders
- An imbalance in certain neurotransmitters (such as serotonin)
- A history of trauma or abuse
- High levels of stress, anxiety, or perfectionism
- Tendency to develop unhealthy coping mechanisms for managing negative emotions
- Mental health disorders like body dysmorphic disorder (BDD), trichotillomania, autism, etc.
- Extra-sensory factors (such as itching or discomfort)
- Peer influence in social or family settings
Read More About Genetics Here
Mental Health Impact Of Dermatillomania
Dermatillomania symptoms can have a significant and adverse impact on an individual’s mental health and overall well-being. The constant preoccupation with skin picking, coupled with the distress it can cause, often leads to heightened anxiety, shame, and feelings of guilt (( Grant, J. E., & Chamberlain, S. R. (2021). Trichotillomania and Skin-Picking Disorder: An Update. Focus (American Psychiatric Publishing), 19(4), 405–412. https://doi.org/10.1176/appi.focus.20210013 )) .
The dermatillomania symptoms can also trigger mental health disorders like Tourette syndrome, borderline personality disorder, Prader-Willi syndrome, Lesch-Nyhan syndrome, Smith-Magenis syndrome, etc.
These emotional factors can further exacerbate the condition and may contribute to a decline in self-esteem, self-image, and body dysmorphia. Moreover, the physical consequences of skin picking can lead to increased social isolation, avoidance of social activities, and decreased quality of life.
Diagnosis For Dermatillomania
In the diagnosis (( Jafferany, M., & Patel, A. (2019). Skin-Picking Disorder: A Guide to Diagnosis and Management. CNS drugs, 33(4), 337–346. https://doi.org/10.1007/s40263-019-00621-7 )) of dermatillomania symptoms, a clinical assessment is conducted by mental health professionals to gather information about the individual’s symptoms, medical history, and potential contributing factors. Clinicians use the DSM-5 criteria to determine if the individual meets the diagnostic criteria.
Additionally, a differential diagnosis is performed to rule out other possible mental health causes of the symptoms. Psychological assessments, often involving self-report questionnaires, help assess the severity and impact of the disorder. In some cases, a medical examination is recommended to exclude underlying medical conditions contributing to skin picking, and collaboration with healthcare professionals like dermatologists may be involved in assessing physical consequences.
How Is Dermatillomania Treated?
Dermatillomania symptoms can be treated through a combination of approaches (( Spiegel, D. R., & Finklea, L. (2009). The recognition and treatment of pathological skin picking: a potential neurobiological underpinning of the efficacy of pharmacotherapy in impulse control disorders. Psychiatry (Edgmont (Pa. : Township)), 6(2), 38–42. )) that address the psychological and behavioral aspects of the disorder:
1. Psychotherapy (Cognitive-Behavioral Therapy):
Cognitive-behavioral therapy (CBT) is one of the most effective treatments for dermatillomania. CBT, besides support group therapy, helps individuals identify and modify the thoughts, emotions, and behaviors associated with skin picking. Specifically, habit reversal training (HRT), a type of CBT, is often used to replace skin picking with healthier coping strategies.
Read More About Psychotherapy Here
2. Alternative Therapies:
Some individuals find relief from the symptoms of dermatillomania through alternative therapies like mindfulness, relaxation techniques, or biofeedback. These approaches can help manage stress and anxiety, reducing the urge to pick at the skin.
3. Medication:
In some cases, healthcare providers may prescribe medication, such as selective serotonin reuptake inhibitors (SSRIs) (( Machado, M. O., Köhler, C. A., Stubbs, B., Nunes-Neto, P. R., Koyanagi, A., Quevedo, J., Soares, J. C., Hyphantis, T. N., Marazziti, D., Maes, M., Stein, D. J., & Carvalho, A. F. (2018). Skin picking disorder: prevalence, correlates, and associations with quality of life in a large sample. CNS spectrums, 23(5), 311–320. https://doi.org/10.1017/S1092852918000871 )) , to help manage the underlying anxiety or obsessive-compulsive symptoms that may contribute to skin picking.
4. Dermatological Interventions:
Collaboration with dermatologists may be necessary to address the physical consequences of skin picking, such as wound care and scar management.
How To Overcome Dermatillomania
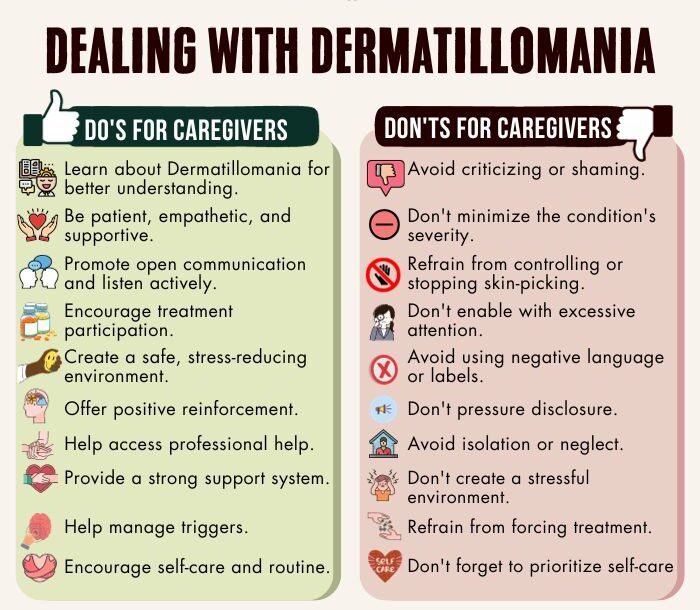
Measures (( Ravipati, P., Conti, B., Chiesa, E., & Andrieux, K. (2021). Dermatillomania: Strategies for Developing Protective Biomaterials/Cloth. Pharmaceutics, 13(3), 341. https://doi.org/10.3390/pharmaceutics13030341 )) on how to overcome dermatillomania typically involve:
- Education: Learn more about dermatillomania to gain insights and tools for self-management.
- Identify Triggers: Recognize the situations, emotions, or stressors that trigger skin-picking episodes.
- Replacement Behaviors: Develop alternative behaviors to replace skin picking, such as fidget toys or stress balls.
- Distraction Techniques: Engage in distracting activities or hobbies to divert your focus from skin picking.
- Mindfulness And Relaxation: Practice mindfulness techniques and relaxation exercises to manage anxiety and reduce the urge to pick.
- Create Barriers: Make it more difficult to engage in skin picking by covering mirrors or wearing gloves.
- Positive Reinforcement: Reward yourself for refraining from skin picking and achieving milestones.
- Establish A Routine: Create a consistent daily routine, including self-care practices, to reduce anxiety and enhance well-being.
- Keep A Journal: Maintain a diary to track your skin-picking episodes and identify patterns.
- Support System: Lean on friends, family, or support groups for encouragement and understanding.
Read More About Mindfulness Here
Takeaway
Dermatillomania can have a significant impact on an individual’s well-being, there is hope for recovery through a combination of therapies, medication, and self-help strategies. Understanding the disorder, seeking professional guidance, and having a strong support system can significantly contribute to the successful management and eventual overcoming of the symptoms of dermatillomania. With patience, persistence, and the right treatment plan, individuals affected by this condition can take positive steps toward a healthier and more fulfilling life.
At A Glance
- Dermatillomania is a mental health condition characterized by repetitive skin-picking behaviors.
- It is also known as excoriation disorder or skin-picking disorder.
- Dermatillomania affects around 1-5% of the global population.
- The symptoms of dermatillomania can manifest in various forms and severity levels.
- The causes of dermatillomania include genetic factors, neurobiological imbalances, psychological factors, etc.
- By seeking professional guidance and having a strong support system, individuals affected by dermatillomania can make significant progress.
- Measures on how to overcome dermatillomania involve self-help strategies, like psycho-education, hobbies, journaling, etc.
Frequently Asked Questions (FAQs)
1. Is dermatillomania a mental illness?
Yes, dermatillomania is considered a mental illness, specifically categorized as an obsessive-compulsive and related disorder.
2. How do I know if I have dermatillomania?
You may have dermatillomania if you exhibit recurrent and compulsive skin-picking behaviors leading to skin lesions and significant distress or impairment.
3. Is skin picking OCD or anxiety?
Skin picking can be related to both OCD and anxiety, as it may serve as a coping mechanism for managing emotional distress.
4. Are there any self-help techniques for coping with dermatillomania between therapy sessions?
Self-help techniques for coping with dermatillomania between therapy sessions include identifying triggers, practicing mindfulness, and employing replacement behaviors to divert the urge to pick.