Dysthymia is a form of depression with milder but more long-lasting symptoms. It is also known as persistent depressive disorder (PDD) or dysthymic disorder.
What Is Dysthymia?
Dysthymia, or dysthymic disorder is a mood disorder characterized by chronic but mild depressive symptoms. Dysthymia can lead to low self-esteem, feelings of worthlessness and hopelessness, decreased productivity, and loss of interest in daily activities. The symptoms can last for several years and can adversely affect one’s ability to pursue education, career, and relationships.
A 2009 study 1 Sansone, R. A., & Sansone, L. A. (2009). Dysthymic disorder: forlorn and overlooked?. Psychiatry ( Edgmont [Pa. : Township] ), 6(5), 46–51. described persistent depressive disorder as a “smoldering mood disturbance” of a long duration (at least two years in adults) with transient periods of normal mood. Two of the undeniable markers of dysthymia are apathy and anhedonia (or a loss of interest in activities).
Most of the time, people with dysthymic disorder symptoms harbor extreme negativity, guilt, and self-criticism—because of which, they resort to socially withdrawn destructive conduct.
They also experience cognitive impairment. This makes them irritable and lacking in concentration and, most of the time, they end up with poorly made decisions or poorly handled conflicts.
This harms their personal, professional, and social functioning. Nonetheless, the depressive symptoms experienced in dysthymia are mild. This makes the disorder easily manageable, even though it may persist throughout a person’s lifetime.
According to a 2021 study, 2 Patel RK, Rose GM. Persistent Depressive Disorder. [Updated 2021 Jul 1]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK541052/ depression as a whole significantly impacts morbidity and mortality, and is a common cause of global disease burden and disability all over the world. Persistent depressive disorder affects 12% 3 Patel RK, Rose GM. Persistent Depressive Disorder. [Updated 2021 Jul 1]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK541052/ of the global population.
It is also associated with a very low prognosis rate, greater severity of depression & anxiety, and complex somatic symptoms in comparison to major depression. Nonetheless, despite its life-long prevalence, it can be effectively managed with therapy, medication, and self-help strategies.
Origin Of Dysthymia
The conceptual origin of dysthymia in psychiatry can be traced back to C.F. Fleming 4 Brieger, P., & Marneros, A. (1995). Das Dysthymiekonzept: Aktuelles und Geschichtliches–ein Uberblick [The dysthymia concept: current and historical aspects–an overview]. Fortschritte der Neurologie-Psychiatrie, 63(10), 411–420. https://doi.org/10.1055/s-2007-996643 , an American psychiatrist, around 1844. But the term actually gained popularity in the 1970s, thanks to another American psychiatrist, Robert Spitzer, one of the creators of the Diagnostic and Statistical Manual of Mental Disorders (DSM).
Spitzer borrowed the term “dysthymia” from the Greek words, dys meaning “ill/bad” and thymia meaning “mind/emotions”. He used the term in the DSM to replace “depressive personality” and elaborately ‘label’ all types of chronic depression.
However, years later, the revised versions of the DSM 5 American Psychiatric Association. (2022). Diagnostic and Statistical Manual of Mental Disorders. https://doi.org/10.1176/appi.books.9780890425787 brought together dysthymic and cyclothymic depressive disorders into an affective category called “persistent depressive disorder” (PDD). Today, PDD is clinically distinguished from major depressive disorder (MDD) and is used to denote a mild, chronic state of depression.
Read More About Major Depressive Disorder Here
Symptoms Of Dysthymia
The symptoms of dysthymic disorder vary from person to person. Because of its close resemblance to major depressive disorder (MDD), the two are often confused. However, research 6 Patel RK, Rose GM. Persistent Depressive Disorder. [Updated 2021 Jul 1]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK541052/ and medical practice shows dysthymia has fewer but longer lasting symptoms than MDD.
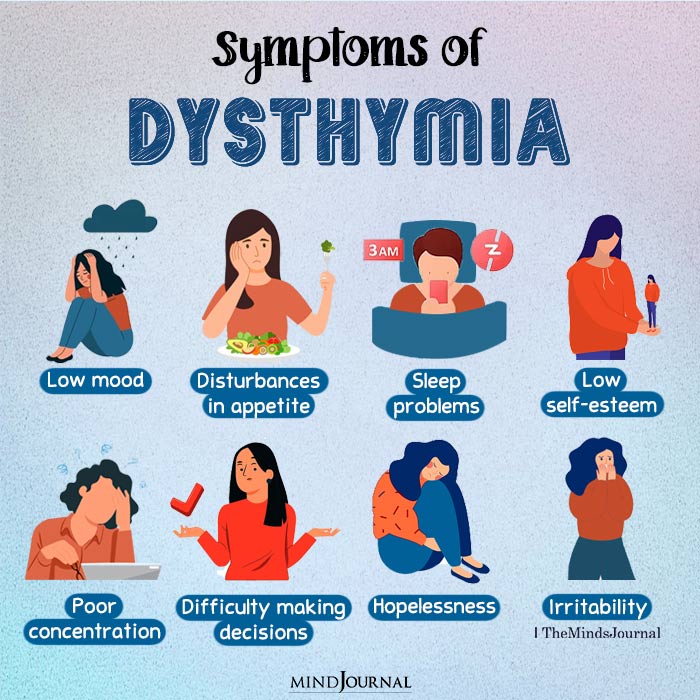
As per the Diagnostic and Statistical Manual of Mental Disorders (DSM) 5 7 American Psychiatric Association. (2022). Diagnostic and Statistical Manual of Mental Disorders. (5th ed.). https://doi.org/10.1176/appi.books.9780890425787 , the main symptoms of persistent depressive disorder include:
- Low mood for most of the day
- Poor appetite or overeating
- Lack of sleep or oversleeping
- Low self-esteem
- Poor concentration
- Difficulty making decisions
- Feelings of hopelessness
- Irritability (mostly seen in children)
As per the DSM 5 criteria, two or more of these symptoms along with constant low mood need to persist continuously for at least two years to qualify for the diagnosis.
Read More About DSM 5 Here
Case Example
Rhea, a 19 year old university student, was referred to her college counselor, as her performance seemed to be suffering. Rhea had been routinely struggling with assignment deadlines and tests, even though professors found her answers in class to be quite intelligent. According to her classmates, Rhea was smart, but lazy.
When the counselor asked Rhea about her frequent late submissions, she stated that it was difficult for her to sustain concentration for too long, and that she would get tired and sleepy soon after starting work.
However, the frustration of not being at par with the rest of the class also distressed Rhea and she often thought she was undeserving of her seat.
On being asked about her predominant mood, Rhea expressed that she was mostly unhappy- about herself and her life, and that’s how it had been for as long as she could remember. She rarely smiled, or did things for fun, but often found comfort in sleeping long hours or eating junk food.
After speaking to Rhea about her family and school life among other things, the counselor explained to her that she might have persistent depressive disorder, and encouraged her to start therapy once a week.
Causes Of Dysthymia
Some of the most common risk factors for persistent depressive disorder, or dysthymia include:
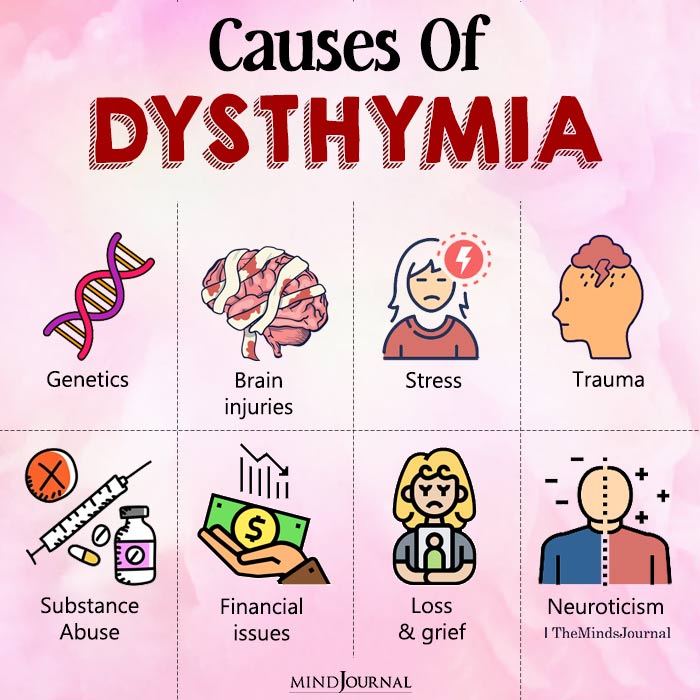
1. Genetics
Dysthymia tends to run in families. In fact, a person with a family history of depression, bipolar disorder, or substance abuse is more vulnerable to PDD. According to a 2013 study 8 Kovanen, L., Kaunisto, M., Donner, K., Saarikoski, S. T., & Partonen, T. (2013). CRY2 genetic variants associate with dysthymia. PloS one, 8(8), e71450. https://doi.org/10.1371/journal.pone.0071450 , “four CRY2 (circadian clock) genetic variants” are significantly related to dysthymia. This makes it a highly genetically transmitted disease.
Read More About Genetics Here
2. Biological causes
Research 9 Ishizaki, J., & Mimura, M. (2011). Dysthymia and apathy: diagnosis and treatment. Depression research and treatment, 2011, 893905. https://doi.org/10.1155/2011/893905 shows that the onset of the dysthymia can be caused by certain structural and functional changes in the brain, particularly in the:
- Corpus callosum
- Frontal lobe
- Amygdala
- Insula
- Cingulate gyrus
Certain brain injuries may affect the functioning of these areas. Studies 10 Patel, R. K., & Rose, G. M. Persistent Depressive Disorder. [Updated 2021 Jul 1]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK541052/ also show that dysfunctional regulation of neurotransmitters like corticotropin-releasing hormone (CRH), arginine vasopressin (AVP), and forebrain serotonergic mechanisms can make people vulnerable to persistent depressive disorder.
Moreover, hormone imbalances and chronic physical illnesses 11 Klein, D. N., Riso, L. P., Donaldson, S. K., Schwartz, J. E., Anderson, R. L., Ouimette, P. C., Lizardi, H., & Aronson, T. A. (1995). Family study of early-onset dysthymia. Mood and personality disorders in relatives of outpatients with dysthymia and episodic major depression and normal controls. Archives of general psychiatry, 52(6), 487–496. can also make a person more vulnerable to persistent depressive disorder.
3. Psychosocial causes
Certain environmental and psychosocial factors 12 Sansone, R. A., & Sansone, L. A. (2009). Dysthymic disorder: forlorn and overlooked?. Psychiatry (Edgmont [Pa. : Township]), 6(5), 46–51. contribute to a person’s suffering from persistent depressive disorder symptoms. Some of these factors include:
- Stress
- Loss and grief
- Parental neglect and abandonment
- A history of violence, abuse, and trauma
- A history of substance use
- Negative developmental experiences
- Other traumatic experiences
- Specific personality types, such as neurotic and anxious types
- Financial hardships, etc.
Read More About Stress Here
Diagnosis Of Persistent Depressive Disorder
Experts have long noted the variation in the symptoms and origins of dysthymia across different age groups. For instance, while adults experience apathy and low moods, children suffering from dysthymic disorder tend to experience irritability more than depressive symptoms. Because of this, dysthymia diagnosis is different, based on the patient’s age group and other factors such as:
- Signs and symptoms of the disorder
- Severity of illness
- Chronicity of illness
- Comorbid conditions
- Medical and family history
- Causes of illness
According to the DSM-5 criteria for persistent depressive disorder 13 American Psychiatric Association. (2022). Diagnostic and Statistical Manual of Mental Disorders. (5th ed.). https://doi.org/10.1176/appi.books.9780890425787 , the first step of diagnosis usually involves a mental health professional examining the patient’s medical history, running a few laboratory tests, asking the patient to fill out psychiatric questionnaires, and outlining a working diagnosis.
Some of the screening scales 14 Rashed, S., Kamel, S., Hassan, M., & Mahfouz, A. (2001). Psychometric study of dysthymic patients and their first-degree relatives. The Journal of the Egyptian Public Health Association, 76(1-2), 89–105. used for diagnosing persistent depressive disorder include:
- Hamilton Depression Rating Scale (HDRS 15 Worboys M. (2013). The Hamilton Rating Scale for Depression: The making of a “gold standard” and the unmaking of a chronic illness, 1960-1980. Chronic illness, 9(3), 202–219. https://doi.org/10.1177/1742395312467658 )
- Beck’s Depression Inventory 16 Beck, A. T., Steer, R. A., & Brown, G. (1996). Beck Depression Inventory–II (BDI-II) [Database record]. APA PsycTests. https://doi.org/10.1037/t00742-000
- Patient Health Questionnaire (PHQ 17 National Collaborating Centre for Mental Health (UK). Depression in Adults with a Chronic Physical Health Problem: Treatment and Management. Leicester (UK): British Psychological Society (UK); 2010. (NICE Clinical Guidelines, No. 91.) Appendix 12, The classification of depression and depression rating scales/questionnaires. Available from: https://www.ncbi.nlm.nih.gov/books/NBK82926/ )
- Hospital Anxiety and Depression Scale (HADS 18 Snaith R. P. (2003). The Hospital Anxiety And Depression Scale. Health and quality of life outcomes, 1, 29. https://doi.org/10.1186/1477-7525-1-29 )
The patient’s performance in the physical tests and psychometric questionnaires is used to determine the nature of their disorder. Accordingly, they are referred to a mental health professional (MHP) for persistent depressive disorder treatment.
Treatment Of Dysthymia/PDD
Dysthymia is a persistent and crippling mental disorder. However, its timely diagnosis and proper treatment can help you better manage the symptoms, take control over the course of the disorder, and lead a happier life. Thankfully, several dysthymia treatment options are available, including:
1.Therapy
Psychotherapy is the cornerstone of treatment for persistent depressive disorder. It has yielded promising treatment outcomes for patients with both chronic and acute depressive disorders.
A 2011 study 19 Ishizaki, J., & Mimura, M. (2011). Dysthymia and apathy: diagnosis and treatment. Depression research and treatment, 2011, 893905. https://doi.org/10.1155/2011/893905 elaborates on its core procedure ‘situational analysis’ which is a highly structured technique that teaches patients with persistent depression to handle difficult interpersonal encounters.
To treat the symptoms, correct the patient’s thought processes and emotional disturbances, and help them develop effective strategies for coping with dysthymia, a variety of long-term psychotherapies are used, including:
- Cognitive-behavioral therapy (CBT 20 Hofmann, S. G., Asnaani, A., Vonk, I. J., Sawyer, A. T., & Fang, A. (2012). The Efficacy of Cognitive Behavioral Therapy: A Review of Meta-analyses. Cognitive therapy and research, 36(5), 427–440. https://doi.org/10.1007/s10608-012-9476-1 )
- Cognitive-behavioral analysis system of psychotherapy (CBASP 21 Swan, J. S., Macvicar, R., Christmas, D., Durham, R., Rauchhaus, P., McCullough, J. P., Jr, & Matthews, K. (2014). Cognitive Behavioural Analysis System of Psychotherapy (CBASP) for chronic depression: clinical characteristics and six month clinical outcomes in an open case series. Journal of affective disorders, 152-154, 268–276. https://doi.org/10.1016/j.jad.2013.09.024 )
- Schema therapy 22 Ishizaki, J., & Mimura, M. (2011). Dysthymia and apathy: diagnosis and treatment. Depression research and treatment, 2011, 893905. https://doi.org/10.1155/2011/893905
- Psychodynamic psychotherapy 23 Ribeiro, Â., Ribeiro, J. P., & von Doellinger, O. (2018). Depression and psychodynamic psychotherapy. Revista brasileira de psiquiatria (Sao Paulo, Brazil : 1999), 40(1), 105–109. https://doi.org/10.1590/1516-4446-2016-2107
- Interpersonal psychotherapy 24 Rajhans, P., Hans, G., Kumar, V., & Chadda, R. K. (2020). Interpersonal Psychotherapy for Patients with Mental Disorders. Indian journal of psychiatry, 62(Suppl 2), S201–S212. https://doi.org/10.4103/psychiatry.IndianJPsychiatry_771_19
Read More About Cognitive Behavioral Therapy (CBT) Here
2. Medication
Since people suffering from dysthymia usually experience long-term depressive symptoms, medical professionals often turn to long-term pharmacological therapy for its treatment. Medications used to treat the symptoms of persistent depressive disorder include:
- Antidepressants 25 von Wolff A, Holzel LP, Westphal A, et al. Selective serotonin reuptake inhibitors and tricyclic antidepressants in the acute treatment of chronic depression and dysthymia: a systematic review and meta-analysis. 2012. In: Database of Abstracts of Reviews of Effects (DARE): Quality-assessed Reviews [Internet]. York (UK): Centre for Reviews and Dissemination (UK); 1995-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK115979/ (like SSRIs, SNRIs, NaSSAs, DNRIs, tetracyclic and tricyclic antidepressants, etc.)
- Dopamine stimulants 26 Silva de Lima, M., & Hotopf, M. (2003). A comparison of active drugs for the treatment of dysthymia. The Cochrane database of systematic reviews, 2003(3), CD004047. https://doi.org/10.1002/14651858.CD004047 and agonists
- Antipsychotic agents 27 Wang, P., & Si, T. (2013). Use of antipsychotics in the treatment of depressive disorders. Shanghai archives of psychiatry, 25(3), 134–140. https://doi.org/10.3969/j.issn.1002-0829.2013.03.002
- Psychostimulants 28 Pary, R., Scarff, J. R., Jijakli, A., Tobias, C., & Lippmann, S. (2015). A Review of Psychostimulants for Adults With Depression. Federal practitioner : for the health care professionals of the VA, DoD, and PHS, 32(Suppl 3), 30S–37S. (like dopaminergic agents)
- Antidementia agents 29 Kogure, T., Tatsumi, T., & Oku, Y. (2010). Four cases of dysthymic disorder and general malaise successfully treated with traditional herbal (kampo) medicines: kamiuntanto. Integrative medicine insights, 5, 1–6. https://doi.org/10.4137/imi.s4586 (like cholinesterase inhibitors, pyrrolidone-type nootropic agents, etc.)
- Cerebral circulation and metabolism stimulants 30 Ballenger J. C. (2000). Anxiety and Depression: Optimizing Treatments. Primary care companion to the Journal of clinical psychiatry, 2(3), 71–79. https://doi.org/10.4088/pcc.v02n0301 (like ergot alkaloid, etc.)
- Antiplatelet drugs 31 Iqbal AM, Lopez RA, Hai O. Antiplatelet Medications. [Updated 2022 May 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK537062/ (like phosphodiesterase inhibitors)
Read More About Antidepressants Here
3. Other forms of treatment
More often than not, combination treatment involving both therapy and medication are used to successfully treat dysthymia. Studies 32 Klein, D. N., Shankman, S. A., & Rose, S. (2006). Ten-year prospective follow-up study of the naturalistic course of dysthymic disorder and double depression. The American journal of psychiatry, 163(5), 872–880. https://doi.org/10.1176/ajp.2006.163.5.872 show that 73.9% of patients showed recovery from dysthymic disorder due to combination treatment.
Because of the very persistent nature of the disorder, sometimes treatment augmentations are employed to aid the prognosis of a patient. Such augmentations include:
- Lithium pharmacology
- Thyroid hormone augmentation
- Amisulpride, buspirone, and bupropion stimulants
- Administration of mirtazapine
- Light therapy 33 Tuunainen, A., Kripke, D. F., & Endo, T. (2004). Light therapy for non-seasonal depression. The Cochrane database of systematic reviews, 2004(2), CD004050. https://doi.org/10.1002/14651858.CD004050.pub2
- Group therapy 34 Hellerstein, D. J., Little, S. A., Samstag, L. W., Batchelder, S., Muran, J. C., Fedak, M., Kreditor, D., Rosenthal, R. N., & Winston, A. (2001). Adding group psychotherapy to medication treatment in dysthymia: a randomized prospective pilot study. The Journal of psychotherapy practice and research, 10(2), 93–103. , etc.
Coping With Dysthymia
Dysthymia is a chronic psychiatric illness that has long-term consequences on our lives. Apart from therapeutic and pharmacological treatment, a large number of self-help strategies exist that can help you better manage the disorder in the long run.
Consider the following measures to help you manage stress, increase psychological resilience, boost self-esteem, and cope with persistent depressive disorder:
- Educate yourself about depression
- Identify the triggers
- Create a structured and disciplined routine
- Exercise regularly
- Eat a healthy and balanced diet
- Follow a sound sleep regime
- Avoid caffeine, alcohol, drugs, and other substances
- Try mindfulness techniques like yoga, meditation, etc.
- Pursue hobbies like cooking, gardening, hiking, etc.
- Try journaling and expressive writing
- Connect with your friends and family
- Socialize more often, both online and offline
- Revisit activities that you once liked
- Try new activities that challenge your existing knowledge and help you learn more
Practicing these coping skills alongside long-term therapy can bolster a steady recovery. Most importantly, remember to be patient and kind to yourself during the entire process of diagnosis, treatment, and recovery from dysthymia.
Takeaway
Dysthymia or persistent depressive disorder is a chronic, long-term type of depression that persists throughout a person’s lifetime. The patient may experience intermittent periods of recovery and relapse.
However, if the symptoms are not managed properly, it can negatively impact one’s quality of life and social relationships. Therefore, timely diagnosis and the right treatment options should be availed to address the negative consequences of this debilitating mental disorder.
At A Glance
- Dysthymia or persistent depressive disorder, is a chronic but mild depressive mood disorder.
- The common dysthymia symptoms include apathy, low moods, anhedonia, social isolation, low appetite, etc.
- Common causes for the development of dysthymia include genetics, biological factors, and psychosocial development.
- If untreated, it can negatively impact one’s quality of life and social relationships.
- Persistent depressive disorder treatment involves therapy and/or medication, as well as self-help strategies.
Frequently Asked Questions (FAQs)
1. Is persistent depressive disorder a disability?
Persistent depressive disorder is a crippling psychiatric disorder that interferes with our daily functioning and quality of life. It may lead to disability in a person.
2. What is the difference between major depressive disorder and dysthymic disorder?
While both are types of depression, these differ in their duration and the number of symptoms. Dysthymic disorder has fewer symptoms, but it lasts longer—sometimes for up to 2 years. Major depressive disorder (MDD), on the other hand, has more symptoms and it doesn’t necessarily last as long as dysthymia, before or after diagnosis.
3. How am I supposed to get out of dysthymia?
Dysthymia does not go away on its own, because of which you should avail certain measures to recover from it. Seek medical help and consider therapy. Certain self-help strategies (like gardening, developing a hobby, journaling, etc.) can also be used to address your dysthymia.
4. Can dysthymia last a lifetime?
If left untreated, dysthymia can sometimes last for the entire lifetime of a person. Since it is milder than acute depressive episodes, a person often learns to live with this condition.
5. Who is most at risk for dysthymic disorder?
As per research data, women under the age of 65, people who are unmarried and people in low income are most at risk for dysthymia. 35 Weissman, M. M., Leaf, P. J., Bruce, M. L., & Florio, L. (1988). The epidemiology of dysthymia in five communities: rates, risks, comorbidity, and treatment. The American journal of psychiatry, 145(7), 815–819. https://doi.org/10.1176/ajp.145.7.815
6. What percent of the population has dysthymic disorder?
Dysthymia occurs in about 1.5% of the global population. 36 Vos, T., Flaxman, A. D., Naghavi, M., Lozano, R., Michaud, C., Ezzati, M., Shibuya, K., Salomon, J. A., Abdalla, S., Aboyans, V., Abraham, J., Ackerman, I., Aggarwal, R., Ahn, S. Y., Ali, M. K., Alvarado, M., Anderson, H. R., Anderson, L. M., Andrews, K. G., Atkinson, C., … Memish, Z. A. (2012). Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet (London, England), 380(9859), 2163–2196. https://doi.org/10.1016/S0140-6736(12)61729-2
7. How to take care of someone with dysthymia?
If someone close to you is suffering from dysthymia, encourage them to seek help from a professional and help them adhere to the treatment. Let them know that you will be there to support them even if they are in a low mood, and try to listen without judgment.