Post-traumatic stress disorder (PTSD) can develop after a person experiences a life-threatening or traumatic event that impairs their ability to function. A proper and accurate diagnosis of post-traumatic stress disorder is important for an effective treatment plan to be devised.
Table of Contents
DSM 5 Diagnosis Of Post-Traumatic Stress Disorder
PTSD can be diagnosed by a trained mental health professional such as a psychologist or a psychiatrist. However, people suffering from PTSD are often reluctant to recall traumatic events or discuss their symptoms, which can make the process of PTSD diagnosis difficult.
For a person to be given a diagnosis of PTSD, their symptoms must be severe and disrupt their daily functioning, while interfering with their work, education, and interpersonal relationships.
According to the DSM 5, you must meet the following diagnostic criteria 1 Center for Substance Abuse Treatment (US). (2014). Exhibit 1.3-4, DSM-5 Diagnostic Criteria for PTSD. Nih.gov; Substance Abuse and Mental Health Services Administration (US). Available from: https://www.ncbi.nlm.nih.gov/books/NBK207191/box/part1_ch3.box16/ for PTSD
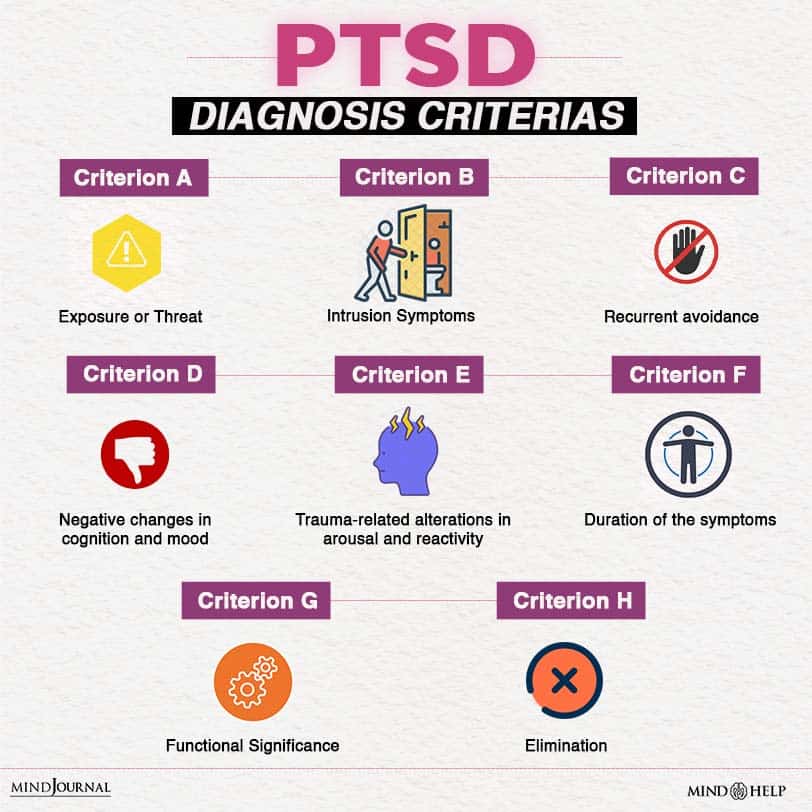
1. Exposure to Trauma
You must have been exposed to one or multiple traumatic events that involve real or threatened death, injury, or even sexual violence through one or more of the ways mentioned below:
- Direct exposure to or experiencing the traumatic event(s)
- Personally witnessing someone else go through a traumatic event(s)
- Learning about the occurrence of the traumatic event(s) to a family member, close relative, or friend.
- Indirect, extreme, and repeated exposure to aversive details of the traumatic event(s). For instance, police officers and first responders. This does not involve exposure through electronic media, television, pictures, or movies unless such exposure is related to work.
2. Intrusive Symptoms
For a proper diagnosis of post-traumatic stress disorder, you must have experienced at least one of the following symptoms linked with the traumatic event(s), after the occurrence of the event:
- Involuntary, recurrent & intrusive distressing thoughts and memories associated with the traumatic event(s). In children above 6 years of age, this can be expressed through repetitive play involving aspects or themes of the traumatic event(s).
- Distressing and recurrent nightmares with the content of the disturbing dreams associated with the traumatic event(s). Children can experience terrifying dreams and they may be unable to recognize the content.
- Dissociative reactions, like flashbacks, wherein you think, feel, or behave as if the traumatic event(s) were recurring. These reactions may take place on a continuum which can vary from minor responses to a total loss of awareness of themselves or their surroundings. For children, trauma-specific reenactment can take place while in play.
- Prolonged or severe psychological distress when exposed to external or internal reminders that may resemble or symbolize aspects of the traumatic event(s).
- Marked physiological reactions when exposed to traumatic reminders, such as high blood pressure or increased heart rate.
3. Avoidance
Additionally, you would have been experiencing recurrent avoidance of cues or reminders related to the event(s) starting after the trauma, as exhibited by one or both of these:
- Avoidance or attempts to avoid difficult and distressing thoughts, feelings, or memories associated with the traumatic event(s).
- Avoidance or attempts to avoid external stimuli or reminders, like places, activities, people, objects, situations, or conversations which can trigger or provoke distressing emotions, memories, or thoughts about the event(s).
4. Negative Mood and Cognition
Another crucial criterion for diagnosis of post-traumatic stress disorder is negative changes in cognition and mood which started or got worse after the traumatic event(s), as indicated by two or more of the following:
- Incapability to remember certain crucial aspects of the traumatic event(s)
- Distorted, exaggerated, and persistent negative expectations or beliefs about yourself, others, or the world in general.
- Repeated distorted cognitions regarding the consequences or causes of the traumatic event(s), resulting in you blaming yourself or others.
- Constant negative emotional state, such as shame, guilt, fear, or anger.
- Noticeably reduced participation or interest in important activities which used to be enjoyable.
- Feelings of isolation, estrangement, or detachment from others.
- Persistent inability to experience or enjoy positive emotions, like feelings of love, satisfaction, inner peace, or happiness.
5. Arousal
Noticeable trauma-related alterations in arousal and reactivity which began or worsened after the occurrence of the traumatic event(s), as demonstrated by two (or more) of the following:
- Irritability and anger outbursts, with little or no stimuli, mostly expressed physically or verbally toward objects or people.
- Reckless or self-destructive behavior.
- Hypervigilance.
- Increased startle response.
- Difficulty concentrating.
- Sleep disturbances or trouble falling or staying asleep.
For DSM 5 diagnosis of PTSD, the symptoms must have persisted for a month or more and not have been caused by physiological effects of substance use, like alcohol, drugs, or medication, or due to another medical condition.
Read More About Symptoms Of PTSD Here
Differential Diagnosis Of PTSD
It is important to distinguish post-traumatic stress disorder from related conditions. Often, symptoms of PTSD may overlap with those of other disorders 2 Blank A. S., Jr (1994). Clinical detection, diagnosis, and differential diagnosis of post-traumatic stress disorder. The Psychiatric clinics of North America, 17(2), 351–383. , such as
- Depression [Read more]
- Dissociative amnesia
- Acute stress disorder [Read more]
- Schizophrenia [Read more]
- ADHD (in children 3 Weinstein, D., Staffelbach, D., & Biaggio, M. (2000). Attention-deficit hyperactivity disorder and posttraumatic stress disorder: differential diagnosis in childhood sexual abuse. Clinical psychology review, 20(3), 359–378. https://doi.org/10.1016/s0272-7358(98)00107-x ) [Read more]
- Sleep disorders, etc. [Read more]
The diagnosis of post-traumatic stress disorder should be given carefully and distinguished from a regular stress response.
How To Get PTSD Diagnosis?
Diagnosis of post-traumatic stress disorder usually follows an elaborate history-taking and evaluation of symptoms. Several instruments 4 Brewin C. R. (2005). Systematic review of screening instruments for adults at risk of PTSD. Journal of traumatic stress, 18(1), 53–62. https://doi.org/10.1002/jts.20007 are available for the screening of post traumatic stress disorder. One of the popular self-report scales is the Trauma Screening Questionnaire (TSQ 5 VA.gov | Veterans Affairs. (2014). Trauma Screening Questionnaire (TSQ). Va.gov. Available from: https://www.ptsd.va.gov/professional/assessment/screens/tsq.asp ) which is a 10-item symptom screen test.
Some clinician-administered screening instruments for the diagnosis of post-traumatic stress disorder include:
- Davidson Trauma Scale 6 Davidson, J. R., Book, S. W., Colket, J. T., Tupler, L. A., Roth, S., David, D., Hertzberg, M., Mellman, T., Beckham, J. C., Smith, R. D., Davison, R. M., Katz, R., & Feldman, M. E. (1997). Assessment of a new self-rating scale for post-traumatic stress disorder. Psychological medicine, 27(1), 153–160. https://doi.org/10.1017/s0033291796004229
- Distressing Event Questionnaire 7 Kubany, E. S., Leisen, M. B., Kaplan, A. S., & Kelly, M. P. (2000). Validation of a brief measure of posttraumatic stress disorder: the Distressing Event Questionnaire (DEQ). Psychological assessment, 12(2), 197–209. https://doi.org/10.1037//1040-3590.12.2.197
- Impact of Event Scale-Revised
- Trauma Symptom Checklist-40
- PTSD Checklist-Civilian Version 8 Blanchard, E. B., Jones-Alexander, J., Buckley, T. C., & Forneris, C. A. (1996). Psychometric properties of the PTSD Checklist (PCL). Behaviour research and therapy, 34(8), 669–673. https://doi.org/10.1016/0005-7967(96)00033-2
- Revised Civilian Mississippi Scale for PTSD 9 Norris, F. H., & Perilla, J. L. (1996). The revised Civilian Mississippi Scale for PTSD: reliability, validity, and cross-language stability. Journal of traumatic stress, 9(2), 285–298. https://doi.org/10.1007/BF02110661
- The Posttraumatic Stress Diagnostic Scale
Takeaway
Diagnosis of post-traumatic stress disorder is important for people to identify and understand their condition. A prompt and accurate diagnosis can not only help guide treatment but also improve the prognosis. If you find yourself relating to any of the criteria mentioned above, consult a mental health professional at the earliest.
At A Glance
- Diagnosis of post-traumatic stress disorder can be tricky and is always made by a mental health professional.
- There are 5 criteria for the diagnosis of PTSD.
- It is important to distinguish PTSD from conditions such as depression, schizophrenia, ADHD, and others.
- Many screening tools are available to diagnose PTSD, including self-report scales and clinician-administered assessments.
- PTSD diagnosis is crucial in guiding treatment.