Rapid Eye Movement (REM), is a stage of sleep, which constitutes about 25% of the total time spent in sleep. It is of interest due to the high neural activity observed during this stage, and its impact on various psychological states.
What Is REM Sleep
Rapid Eye Movement (REM) sleep is a phase of erratic movement of the eyes during the sleep cycles of mammals, birds and reptiles, marked by muscle relaxation and tendency of the sleeper to dream more vividly. Rapid Eye Movement sleep “is associated with active dreaming,” explains a 2016 study 1 Carley, D. W., & Farabi, S. S. (2016). Physiology of Sleep. Diabetes spectrum : a publication of the American Diabetes Association, 29(1), 5–9. https://doi.org/10.2337/diaspect.29.1.5 .
This sleep stage is also identified as desynchronized sleep and paradoxical sleep (PS) as this phase of sleep resembles waking states. During REM sleep, the eyes stop sending information to the visual cortex, which does not happen in other dream cycles. This stage usually sets in an hour and half after a person falls asleep, and is notable for having the greatest frequency and vividness of dreams experienced.
REM is preceded by NREM (non-rapid eye movement) sleep, which is a dreamless state. In NREM sleep, cognitive activity is low, with the individual progressing into deeper sleep as time passes. It should be noted that REM and NREM sleep are physiologically distinct from each other.
However, both sleep stages occur during a single sleep cycle and tend to last for about 90 minutes in an adult individual. With the progress of the sleep cycle, REM sleep tends to expand in proportion which can cause certain physical changes, such as electrical bursts known as Ponto-geniculo-occipital (PGO 2 Lim, A. S., Lozano, A. M., Moro, E., Hamani, C., Hutchison, W. D., Dostrovsky, J. O., Lang, A. E., Wennberg, R. A., & Murray, B. J. (2007). Characterization of REM-sleep associated ponto-geniculo-occipital waves in the human pons. Sleep, 30(7), 823–827. https://doi.org/10.1093/sleep/30.7.823 ) waves in the brain. It can also cause the sudden loss of muscle tone, which is identified as REM atonia 3 Brooks, P. L., & Peever, J. H. (2008). Unraveling the mechanisms of REM sleep atonia. Sleep, 31(11), 1492–1497. https://doi.org/10.1093/sleep/31.11.1492 .
Understanding REM Sleep
It has been observed that when we sleep, we go through 4 separate stages of sleep that involve both rapid eye movement and non-rapid eye movement sleep. During sleep, we cycle around 4-6 times through these stages with each sleep phase lasting for around 90 minutes. A recent 2021 research paper 4 Jawabri KH, Raja A. Physiology, Sleep Patterns. [Updated 2021 May 9]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK551680/ explains that the REM stage is the “final stage of the sleep, where the skeletal muscle is atonic and immobile, except for the eyes and the diaphragmatic breathing muscle in which they remain active.”
The researchers add that this phase begins after 90 minutes of sleep. The first cycle tends to last for around 10 minutes and eventually increases in duration to reach 1 hour throughout the night. The stage occurs multiple times in a night and involves about 25% of an adult person’s sleep cycle, while covering more than 50% of a child’s.
This sleep stage is associated with vivid dreams, mood, memory and learning. According to a 2018 study 5 Voss, U., & Klimke, A. (2018). Dreaming during REM sleep: autobiographically meaningful or a simple reflection of a Hebbian-based memory consolidation process?. Archives italiennes de biologie, 156(3), 99–111. https://doi.org/10.12871/00039829201832 , it is “a state of desynchronized electrophysiological activity of the brain,” which is related to mental activities involving complex visual experiences or dreaming. Dreams during this stage tend to be incohesive, bizarre and highly emotional involving major life events, like attachment figures and abuse. “REM sleep dreams are often subjectively perceived as story-like and autobiographically meaningful,” adds the study.
However, studies 6 Purves D, Augustine GJ, Fitzpatrick D, et al., editors. Neuroscience. 2nd edition. Sunderland (MA): Sinauer Associates; 2001. The Possible Functions of REM Sleep and Dreaming. Available from: https://www.ncbi.nlm.nih.gov/books/NBK11121/ have found that this sleep stage or the lack of it for at least two weeks does not lead to any significant impact on behavior. However, less rapid eye movement sleep or frequent awakenings can adversely affect sleep quality & performance accuracy 7 Della Monica, C., Johnsen, S., Atzori, G., Groeger, J. A., & Dijk, D. J. (2018). Rapid Eye Movement Sleep, Sleep Continuity and Slow Wave Sleep as Predictors of Cognition, Mood, and Subjective Sleep Quality in Healthy Men and Women, Aged 20-84 Years. Frontiers in psychiatry, 9, 255. https://doi.org/10.3389/fpsyt.2018.00255 in adults. Due to rapid eye movement muscle atonia, we typically do not act out our dreams 8 Farooq M, Anjum F. Sleep Paralysis. [Updated 2021 Jun 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK562322/ . Although our brain remains active during this phase, our breathing tends to become irregular and rapid.
Stages Of Sleep
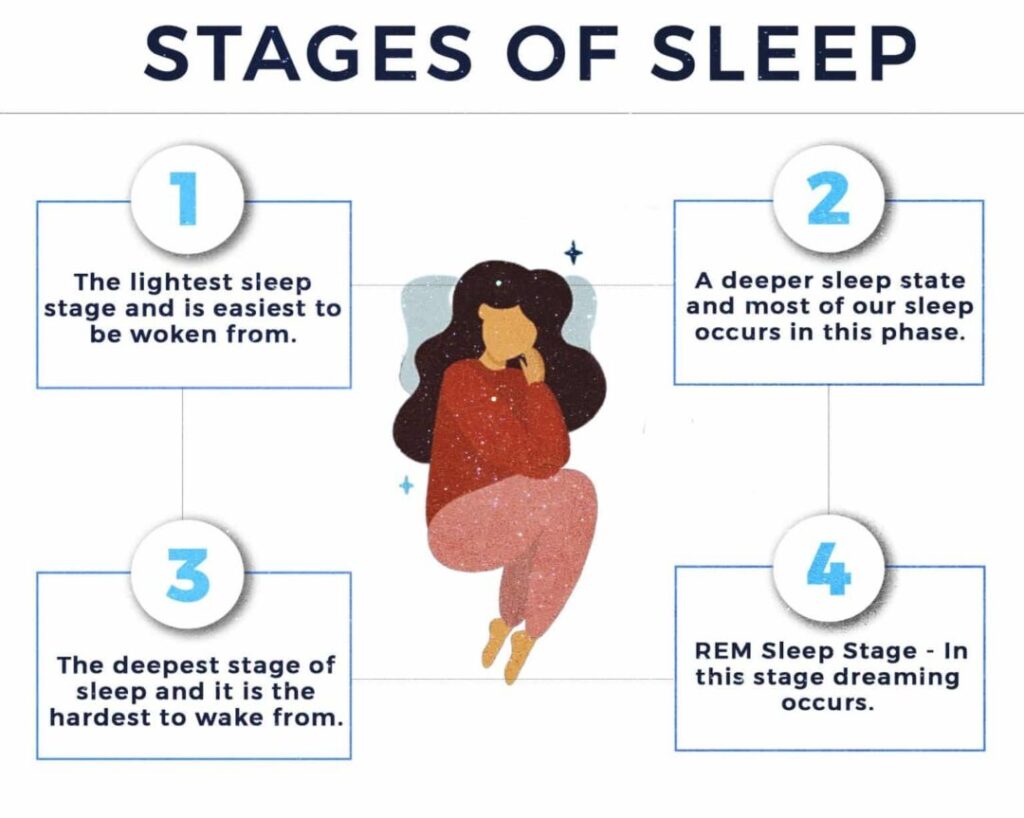
According to a recent study 9 Patel AK, Reddy V, Araujo JF. Physiology, Sleep Stages. [Updated 2021 Apr 22]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK526132/ , humans experience a cycle of 4 different stages that involve both rapid eye movement and non rapid eye movement sleep. These stages are categorized as follows –
A. Stage 1
Identified as N1, it is the lightest sleep stage. Typically, it lasts between one and five minutes and comprises around 5% of the total sleep cycle. “There is muscle tone present in the skeletal muscle, and breathing tends to occur at a regular rate,” states the study. It involves regular breathing patterns and is easiest to be woken from.
B. Stage 2
This stage is known as N2 and most of our sleep occurs in this phase. It is a deeper sleep state which includes reduced body temperature and heart rate. It usually makes up 50% of sleep, with neural activity shifting to delta waves. This stage can last for around 25 minutes in the first cycle and expands with successive cycles.
C. Stage 3
The third stage or N3 is the deepest stage of sleep, it is the hardest to wake from, and is the reparative stage. Time spent in this stage decreases with age, and being awoken during this stage results in sleep inertia, where mental performance is impaired from 30 minutes to an hour. The study adds “This is the stage when the body repairs and regrows its tissues, builds bone and muscle, and strengthens the immune system.”
D. Stage 4: REM Sleep
In this stage 10 Ferri, R., Rundo, F., Silvani, A., Zucconi, M., Bruni, O., Ferini-Strambi, L., Plazzi, G., & Manconi, M. (2017). REM Sleep EEG Instability in REM Sleep Behavior Disorder and Clonazepam Effects. Sleep, 40(8), 10.1093/sleep/zsx080. https://doi.org/10.1093/sleep/zsx080 dreaming occurs and is characterized by atonic skeletal muscles and prevention of movement. “The exception is the eye and diaphragmatic breathing muscles, which remain active,” adds the recent study. The initial period is around 10 minutes but may extend upto one hour.
Signs Of REM Sleep
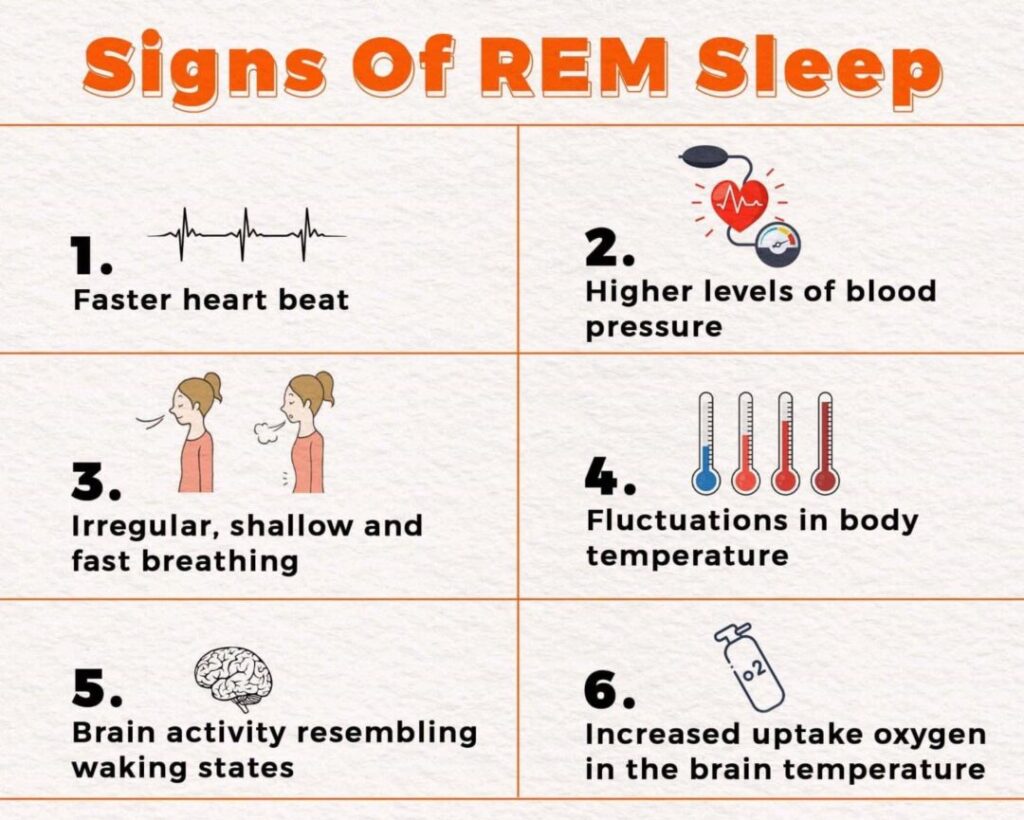
Both the brain and the body go through a series of changes that are particular to REM sleep. Some of these changes include:
- Rapid, ballistic eye movements with sudden changes in the center of fixation
- Faster heart beat
- Higher levels of blood pressure
- Irregular, shallow and fast breathing
- Fluctuations in body temperature
- Brain activity resembling waking states
- Increased uptake oxygen in the brain
- Twitching limbs and facial muscles
- Temporary muscle paralysis or atonia
- Sexual arousal in male and female adults
Causes Of REM Sleep Loss
The exact causes for the lack of rapid eye movement sleep is not yet well understood but it can be influenced by a number of different factors such as, older age, being female gender, degenerative neurological conditions like Parkinson’s disease, narcolepsy, dementia, stroke, brain tumors, multiple system atrophy and use of antidepressants 11 Wichniak, A., Wierzbicka, A., Walęcka, M., & Jernajczyk, W. (2017). Effects of Antidepressants on Sleep. Current psychiatry reports, 19(9), 63. https://doi.org/10.1007/s11920-017-0816-4 . Sleep patterns can also be severely affected by alcohol or substance abuse, with cannabis and antidepressant medication being prime contenders. Other significant substances include:
- Caffeine
- Lithium
- Benzodiazepines
- Opioids
- Methamphetamines
When these are taken medicinally, the impact on sleep can be outweighed by the potential benefits of the substance, but substance abuse can lead to long-term disruption of sleep cycles 12 Roehrs, T. A., & Roth, T. (2015). Sleep Disturbance in Substance Use Disorders. The Psychiatric clinics of North America, 38(4), 793–803. https://doi.org/10.1016/j.psc.2015.07.008 . These specifically impact REM sleep, as evidenced by users reporting their lack of dreams during sleep. Physical conditions like sleep apnea, narcolepsy, and brain damage can also cause REM sleep disturbance, though it is usually treatable by repairing the causal factors. Stress is also commonly attributed to a lack of quality sleep, though this does not always become a chronic condition.
Adverse Effects Of Inadequate REM Sleep
Here are some of the most common physical and psychological effects of lacking rapid eye movement sleep –
1. Physical effects
Lack of adequate sleep can manifest in a number of undesirable physical outcomes, with research 13 Roehrs, T., Hyde, M., Blaisdell, B., Greenwald, M., & Roth, T. (2006). Sleep loss and REM sleep loss are hyperalgesic. Sleep, 29(2), 145–151. https://doi.org/10.1093/sleep/29.2.145 indicating that loss of REM sleep can even increase a person’s sensitivity to pain. Other notable physical symptoms include:
- Increased risk of obesity 14 Liu, X., Forbes, E. E., Ryan, N. D., Rofey, D., Hannon, T. S., & Dahl, R. E. (2008). Rapid eye movement sleep in relation to overweight in children and adolescents. Archives of general psychiatry, 65(8), 924–932. https://doi.org/10.1001/archpsyc.65.8.924 : Lack of engagement in activity can cause obesity.
- Increased inflammatory response 15 Yehuda, S., Sredni, B., Carasso, R. L., & Kenigsbuch-Sredni, D. (2009). REM sleep deprivation in rats results in inflammation and interleukin-17 elevation. Journal of interferon & cytokine research : the official journal of the International Society for Interferon and Cytokine Research, 29(7), 393–398. https://doi.org/10.1089/jir.2008.0080 : Greater feelings of pain in individuals with low REM sleep.
- Constant drowsiness 16 Salvo, F. D., & Victoria, G. (2020). The Effects of Sleep Deprivation on Mental Health and Neurological Disorders. STARS – Showcase of Text, Archives, Research & Scholarship at UCF. https://stars.library.ucf.edu/cgi/viewcontent.cgi?article=1829&context=honorstheses : Individuals reported falling heavy-eyed, dosy and sleepy.
- Lethargy 17 Neu, D., Mairesse, O., Verbanck, P., Linkowski, P., & Le Bon, O. (2014). Non-REM sleep EEG power distribution in fatigue and sleepiness. Journal of psychosomatic research, 76(4), 286–291. https://doi.org/10.1016/j.jpsychores.2014.02.002 : Individuals reported feeling tired all the time.
- Poor balance and motor coordination 18 Walker, M. P., Brakefield, T., Seidman, J., Morgan, A., Hobson, J. A., & Stickgold, R. (2003). Sleep and the time course of motor skill learning. Learning & memory (Cold Spring Harbor, N.Y.), 10(4), 275–284. https://doi.org/10.1101/lm.58503 : Children who slept properly showed better development than those who did not.
- Weakened immune system 19 Imeri, L., & Opp, M. R. (2009). How (and why) the immune system makes us sleep. Nature reviews. Neuroscience, 10(3), 199–210. https://doi.org/10.1038/nrn2576 : Individuals reported more frequent instances of falling sick when they were sleep deprived.
- Increased blood pressure 20 Grote, L., Radeck, A., Heitmann, J., Althaus, W., Ploch, T., Peter, J. H., & Wichert, P. V. (1995). Nächtliche Hypertonie und Schlafapnoe: Effekt des ACE-Hemmers Cilazapril auf apnoe-induzierte Blutdruckanstiege im Schlaf [Nocturnal hypertension and sleep apnea: effect of the ACE inhibitor cilazapril on apnea-induced blood pressure increases during sleep]. Pneumologie (Stuttgart, Germany), 49 Suppl 1, 170–174. : Increased stress can lead to hypertension.
2. Psychological effects
Psychological outcomes are also poor, as individuals with irregular sleep cycles experience a marked increase in their risk of developing disorders like anxiety or depression, and those with already existing mental conditions can risk excarberating their conditions further by not getting decent quality of sleep. Lack of REM sleep can aid the manifestation or worsen the symptoms of :
1. Depression
Difficulty taking care of oneself often leaves depressed individuals with poor sleep routines and unhygienic environments, which can reduce sleep quality, forming a negative feedback loop. Sleep-focused interventions might provide some benefit in these cases.
Read More About Major Depressive Disorder ( Depression ) Here
2. Attention deficit hyperactivity disorder (ADHD)
Individuals with ADHD have trouble falling asleep due to a greater chance of developing obstructive sleep apnea or circadian rhythm disruptions. Research indicates that this lack of sleep may in turn worsen the symptoms of ADHD. Controlling those aspects through medication could be helpful.
3. Schizophrenia
Schizophrenia features distortions of reality, and the frequent insomnia associated 21 Palmese, L. B., DeGeorge, P. C., Ratliff, J. C., Srihari, V. H., Wexler, B. E., Krystal, A. D., & Tek, C. (2011). Insomnia is frequent in schizophrenia and associated with night eating and obesity. Schizophrenia research, 133(1-3), 238–243. https://doi.org/10.1016/j.schres.2011.07.030 with it can be worsened by the medication prescribed. Proper sleep routines help bring back order to a person’s life, and should be pursued to aid recovery.
Read More About Schizophrenia Here
4. Anxiety
Chronic insomnia can be a significant risk factor 22 Neckelmann, D., Mykletun, A., & Dahl, A. A. (2007). Chronic insomnia as a risk factor for developing anxiety and depression. Sleep, 30(7), 873–880. https://doi.org/10.1093/sleep/30.7.873 for the development of anxiety in individuals. Sleep deprivation can also worsen 23 Goldstein, A. N., Greer, S. M., Saletin, J. M., Harvey, A. G., Nitschke, J. B., & Walker, M. P. (2013). Tired and apprehensive: anxiety amplifies the impact of sleep loss on aversive brain anticipation. The Journal of neuroscience : the official journal of the Society for Neuroscience, 33(26), 10607–10615. https://doi.org/10.1523/JNEUROSCI.5578-12.2013 the symptoms of an anxious person, and targeted sleep restoration can be potentially used therapeutically.
Read More Anxiety Here
REM Sleep Behavior Disorder
REM Sleep Behavior Disorder is a condition in which a person acts out their dreams while in rapid eye movement sleep. Normally, this would not be possible due to the atonia present that keeps the person’s body immobile, but the disorder usually manifests due to extraneous variables that affect the neurons that specifically do that.
According to a recent research paper 24 Khawaja I, Spurling BC, Singh S. REM Sleep Behavior Disorder. [Updated 2021 Apr 30]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK534239/ , “Rapid eye movement (REM) sleep behavior disorder is a parasomnia in which affected individuals act out their dreams while in the REM stage of sleep.” It can lead to violence and injury of self or others “without conscious awareness.” Common symptoms of the condition may include –
- Clear recollection of the dream after waking up
- Kicking, thrashing in bed, or any other form of movement caused as the result of acting out the dream
- Yelling, speaking, or more extreme versions of speech manifesting during sleep.
There are a variety of risk factors 25 Postuma, R. B., Montplaisir, J. Y., Pelletier, A., Dauvilliers, Y., Oertel, W., Iranzo, A., Ferini-Strambi, L., Arnulf, I., Hogl, B., Manni, R., Miyamoto, T., Mayer, G., Stiasny-Kolster, K., Puligheddu, M., Ju, Y., Jennum, P., Sonka, K., Santamaria, J., Fantini, M. L., Zucconi, M., … Wolfson, C. (2012). Environmental risk factors for REM sleep behavior disorder: a multicenter case-control study. Neurology, 79(5), 428–434. https://doi.org/10.1212/WNL.0b013e31825dd383 that can increase an individual’s chances of developing the disorder, which include
- Head Injury
- Narcolepsy
- Parkinson’s disease
- Smoking
- Pesticide exposure
Strategies To Improve REM Sleep

Fortunately, there are a number of ways an individual can improve the quality of their sleep. The easiest is to take note of the sleep environment, i.e. the pillows and mattress that are used during sleep. Maintaining a certain degree of care with regards to this can improve sleep quality by promoting relaxation and ease of sleep. Sleep quality can be improved by a marginal degree by focusing on the following:
1. Substance use
Controlling substance use and avoiding alcohol before sleeping can be beneficial to healthy sleep patterns.
2. Environment
The use of ambient noise, or just improving the smell of the sleeping area can maximise the perceived benefits. Moreover, practicing healthy sleep hygiene 26 Yazdi, Z., Loukzadeh, Z., Moghaddam, P., & Jalilolghadr, S. (2016). Sleep Hygiene Practices and Their Relation to Sleep Quality in Medical Students of Qazvin University of Medical Sciences. Journal of caring sciences, 5(2), 153–160. https://doi.org/10.15171/jcs.2016.016 is also recommended.
3. Minimizing electronic usage
Reducing screen time before sleep can decrease the onset time for deep sleep, and reducing one’s reliance on alarms helps ensure uninterrupted sleep. Hence, it is advisable for individuals to set up their nightly routine with an adequate amount of time allocated to screen-free time before sleep.
4. Sleep consolidation
This involves restriction of the time spent falling asleep. Rather than spending hours tossing and turning in bed, it might actually be better to sleep at a later time by managing one’s sleep behaviors.
5. Melatonin
Consumption of melatonin before sleep has also been shown to improve the quality and duration of REM sleep, and is a possible avenue for those who are on medication that interferes with sleep.
6. Routine
Following a sleep schedule by maintaining consistency in the time going to and waking up from sleep improves the overall quality of sleep.
7. Dream journals
Remembering your dreams by writing them down as soon as you wake up supports healthy REM sleep. Practicing this on a regular basis may lead to a phenomenon called lucid dreaming 27 Voss, U., Holzmann, R., Tuin, I., & Hobson, J. A. (2009). Lucid dreaming: a state of consciousness with features of both waking and non-lucid dreaming. Sleep, 32(9), 1191–1200. https://doi.org/10.1093/sleep/32.9.1191 , where the dreamer is aware of the fact that they are in a dream.
8. Meditation
Practicing mindfulness meditation helps in reducing stress and improving overall quality of sleep. Meditating bears long term benefits 28 Lardone, A., Liparoti, M., Sorrentino, P., Rucco, R., Jacini, F., Polverino, A., Minino, R., Pesoli, M., Baselice, F., Sorriso, A., Ferraioli, G., Sorrentino, G., & Mandolesi, L. (2018). Mindfulness Meditation Is Related to Long-Lasting Changes in Hippocampal Functional Topology during Resting State: A Magnetoencephalography Study. Neural plasticity, 2018, 5340717. https://doi.org/10.1155/2018/5340717 like improved cognitive functions, and a reduction of age related brain degeneration.
9. Exercise
Regular exercise is also conducive to better sleep. The release of endorphins during physical activity has a positive effect on overall mood and sleep quality.
10. Diet
Maintaining a healthy diet is essential for both the body and the mind. Research 29 Binks, H., E Vincent, G., Gupta, C., Irwin, C., & Khalesi, S. (2020). Effects of Diet on Sleep: A Narrative Review. Nutrients, 12(4), 936. https://doi.org/10.3390/nu12040936 suggests that the consumption of certain foods, like fatty fish, almonds and milk can significantly improve sleep quality.
Takeaway
The importance of quality sleep had been well established by scientists in the past. Modern research 30 Patel, A. K., Reddy, V., & Araujo, J. F. (2021). Physiology, Sleep Stages. In StatPearls. StatPearls Publishing. has further identified the different cycles of sleep and their significance. REM sleep is a part of the sleep cycle that impacts memory consolidation and vivid dreams, and it is essential that the brain goes through this cycle for appropriate cognitive functioning.
REM sleep At A Glance
- Rapid Eye Movement (REM), is a stage of sleep, which constitutes about 25% of the total time spent in sleep.
- This sleep stage is associated with vivid dreams, mood, memory and learning.
- Dreams during this stage tend to be incohesive, bizarre and highly emotional involving major life events, like attachment figures and abuse.
- Both the brain and the body go through a series of changes that are particular to REM sleep.
- Physical conditions like sleep apnea, narcolepsy, and brain damage can also cause REM sleep disturbance.
- REM Sleep Behavior Disorder is a condition in which a person acts out their dreams while in rapid eye movement sleep.















