Nightmare disorder is a psychiatric condition marked by repeated, extremely vivid and distressing nightmares. Although nightmares are common, some individuals can have frequent well-remembered nightmares that can affect their sleep and waking life. When left untreated, nightmares can affect the mental and physical well being of a person.
What Is A Nightmare?
A nightmare is a distressing, realistic, bad dream that disrupts a person’s sleep and causes the dreamer to be abruptly awakened from sleep. Nightmares are terrifying & vivid nocturnal episodes that can be bizarre and threatening. These can often involve well-organized dream sequences which appear increasingly disturbing and real. They often trigger a range of negative emotions, like terror, fear and anxiety. The U.S. National Library of Medicine defines “A nightmare is a bad dream that brings out strong feelings of fear, terror, distress, or anxiety.” Such dreams can also induce feelings of disgust, embarrassment, rage or anger.
Most people have bad dreams occasionally, but when it occurs frequently, it can affect their ability to function in daily life. Although these usually do not lead to any physical harm, they can be psychologically and emotionally disturbing and prevent a person from getting proper sleep. In extreme cases, it may lead to sleep deprivation. According to sleep medicine, nightmares are different from bad dreams as only the former can cause the sufferer to wake up from sleep. Although the subject of the dream depends on the person, repetitive nightmares tend to have some similar themes, such as unable to escape danger, feeling trapped or lost or falling down from a height.
Understanding Nightmare Disorder
Nightmare disorder, formerly called dream anxiety disorder, is a form of parasomnia or sleep disorder that is characterized by frequent and repeated frightening nightmares & dreams causing awakenings from deep sleep. People suffering from this psychological condition experience terrifying nightmares with severe frequency and disruptions in sleep & wakefulness. It is classified as a cluster of diagnoses known as sleep-wake disorders.
Mind Help explains that the disorder involves “frequent nightmares that impair daytime and nighttime function. These repeated extended, severely dysphoric, and well-remembered dreams revolve around upsetting themes of threats to survival, security, or physical integrity, leading to abrupt awakenings and alertness.” The condition tends to cause –
- Mood disturbances & behavioral problems
- Sleep resistance & bedtime anxiety
- Cognitive impairments
- Impairment in important areas of functioning
- Impairment in interpersonal & social functioning
- Adverse effect on family functioning and stress on caregiver
- Low energy, fatigue & daytime sleepiness
Dream anxiety disorder usually does not result in any serious clinical impairments but the sufferer is highly likely to experience severe distress. However, if the condition results in sleep avoidance and sleep deprivation, it may lead to impaired functioning, performance and concentration during the daytime.
A 2019 study [mfn] Gieselmann, A., Ait Aoudia, M., Carr, M., Germain, A., Gorzka, R., Holzinger, B., Kleim, B., Krakow, B., Kunze, A. E., Lancee, J., Nadorff, M. R., Nielsen, T., Riemann, D., Sandahl, H., Schlarb, A. A., Schmid, C., Schredl, M., Spoormaker, V. I., Steil, R., van Schagen, A. M., … Pietrowsky, R. (2019). Aetiology and treatment of nightmare disorder: State of the art and future perspectives. Journal of sleep research, 28(4), e12820. https://doi.org/10.1111/jsr.12820 [/mfn] defines nightmare disorder as “the repeated occurrence of nightmares that cause clinically significant distress or impairment in social, occupational or other important areas of functioning, which are not attributable to the physiological effects of a substance (e.g. drug abuse or medication) and which cannot be adequately explained by coexisting mental and medical disorders.”
The condition is often caused by stress, anxiety, depression, trauma, medications or substance abuse and other psychiatric disorders, like posttraumatic stress disorder (PTSD), depression. It can be physically, emotionally, socially and occupationally disabling for the sufferer, if left untreated.
How Nightmares Affect Us
Although nightmares usually begin by age 10, these disturbing psychological experiences may occur at any age. It usually takes place during REM (rapid eye movement), sleep, the sleep stage involving intense dreams, and causes sudden awakenings from sleep. Nightmares usually occur in the latter stages of sleep when REM sleep is longer. The sufferer can often be sharply aware of the dream after waking up from the nightmare and feel severely anxious, worried or upset. The person may also experience –
- Disorientation or confusion
- Sweating
- Heart palpitations
- Shortness of breath
- Elevated periodic leg movements
They may also find it hard to fall asleep again after an episode due to intense negative emotions, such as fear, shame and sadness. These emotions and physiological symptoms can be experienced while having the dreams, after awakening from the nightmares or while recollecting the dream experience later. Nightmares associated with past traumatic experiences can make the person feel like they are realistically reliving the experience. Frequent episodes of a nightmare can also cause insomnia, disturbances in the sleep cycle and may also lead to difficulty in functioning during daytime. Research [mfn] Levin R, Fireman G. Nightmare prevalence, nightmare distress, and self-reported psychological disturbance. Sleep. 2002 Mar 15;25(2):205-12. PMID: 11902430. [/mfn] reveals that the incidence of nightmares is associated with higher psychological disturbance and poorer waking functioning.
Prevalence Of Nightmares
Nightmare disorder is a rare condition even though nightmares are common among the general people. A nightmare is considered as an extended and severe dysphoric dream involving desperate attempts to avoid survival threats. Involving outlandish plots, these dreams tend to be more common in women than men. It has been reported that nightmares in women are associated with an anxiety disorder, depressive disorder or both. According to a 2010 study [mfn] Li, S. X., Zhang, B., Li, A. M., & Wing, Y. K. (2010). Prevalence and correlates of frequent nightmares: a community-based 2-phase study. Sleep, 33(6), 774–780. https://doi.org/10.1093/sleep/33.6.774 [/mfn], frequent nightmares are common in the general population.
At least 5.1% of people experience a nightmare at least once per week. Recent research [mfn] Morgenthaler TI, Auerbach S, Casey KR, Kristo D, Maganti R, Ramar K, Zak R, Kartje R. Position Paper for the Treatment of Nightmare Disorder in Adults: An American Academy of Sleep Medicine Position Paper. J Clin Sleep Med. 2018 Jun 15;14(6):1041-1055. doi: 10.5664/jcsm.7178. PMID: 29852917; PMCID: PMC5991964. [/mfn] shows that about 4% of adults are affected by nightmare disorder, “occurring in isolation or as part of other disorders such as posttraumatic stress disorder (PTSD).” The condition is prevalent more in younger adults than older people. Further research reveals that about 50%-85% of adults experience at least one occasional nightmare, while around 2%-8% of general people experience an ongoing problem. The frequency tends to be higher in people with a clinical condition.
The frequency of nightmares is associated with a number of factors, such as:
- Female sex
- Insomnia symptoms
- Sleep-disordered breathing symptoms
- Sleep-related daytime consequences
- Low family income
- Sociodemographic characteristics
- Comorbid sleep and psychiatric disorders
The 2010 study states that repetitive nightmares are also “independently related to the neuroticism personality trait, irrespective of psychiatric diagnosis.” It found that frequent nightmares can increase the risk of developing a psychiatric disorder, like mood disorders, by 5.74 times. The researchers found that people experiencing frequent nightmare episodes were higher on neuroticism in the personality scale. Another study [mfn] Ohayon MM, Morselli PL, Guilleminault C. Prevalence of nightmares and their relationship to psychopathology and daytime functioning in insomnia subjects. Sleep. 1997 May;20(5):340-8. doi: 10.1093/sleep/20.5.340. PMID: 9381055. [/mfn] revealed that about 18.3% of people with insomnia suffer from nightmares. Repeated episodes can often lead to –
- Sleep with many awakenings
- Abnormally long sleep onset
- Daytime memory impairment after poor nocturnal sleep
- Daytime anxiety after poor nocturnal sleep
One 2000 study [mfn] Schredl, M., Blomeyer, D. & Görlinger, M. Nightmares in children: Influencing factors. Somnologie 4, 145–149 (2000). https://doi.org/10.1007/s11818-000-0007-z [/mfn] found that among children between 6 and 11 years of age, 5% to 41% of them experienced at least one nightmare per week. Moreover, the frequency of episodes are higher in girls than in boys. It also found that nightmares can often occur along with night terrors and sleepwalking.
Bad Dreams, Nightmares & Night Terrors
Nightmares are more emotionally intense than bad dreams. Individuals experiencing nightmares tend to experience more fear and anxiety when compared to bad dreams. Moreover, nightmares tend to have more aggressive stories or plots and unhappy endings than the less intense bad dreams. Although both night terrors and nightmares can make a person wake up from deep sleep due to fear, both are different conditions. “Nightmares are different from night terrors,” states the U.S. National Library of Medicine. In night terrors, the sufferer tends to awaken with more severe and intense symptoms, like crying or screaming, after the episode than in nightmare disorder.
Night terrors generally occur in the initial few hours of sleep, while nightmares occur mostly during the later stages. Night terrors are typically experienced as emotions and not as dreams. Unlike nightmares, people experiencing night terrors are unable to recall the details about their terrifying ordeal upon awakening. According to a 2018 study [mfn] Boyden, S. D., Pott, M., & Starks, P. T. (2018). An evolutionary perspective on night terrors. Evolution, medicine, and public health, 2018(1), 100–105. https://doi.org/10.1093/emph/eoy010 [/mfn], as most people do not have “one clear definition of night terrors”, they often tend to confuse them with nightmares. The research authors explain “Notably, night terrors are distinguishable from less severe nightmares by difficulty in waking” the sufferer.
Types Of Nightmare
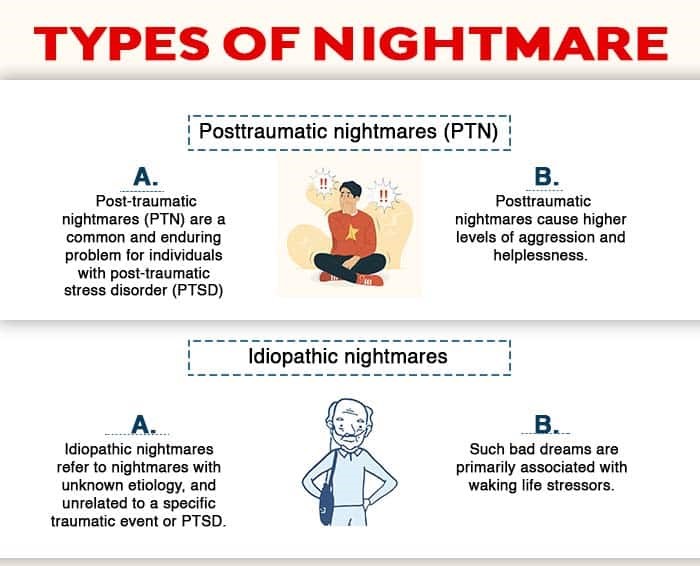
According to experts, nightmares can be categorized into two broad types, namely posttraumatic nightmares and idiopathic nightmares.
1. Posttraumatic nightmares (PTN)
Nightmares and dreaming disturbances that occur as a stress reaction after an exposure to a traumatic event are considered as posttraumatic nightmares. These are either an almost realistic reproduction of a traumatic event experienced in the past or involve content or emotions symbolically associated with trauma.
PTN is mostly experienced by people with post-traumatic stress disorder (PTSD) “PTN cause significant distress, are associated with large costs, and are an independent risk factor for suicide,” explains a 2018 study [mfn] Waltman SH, Shearer D, Moore BA. Management of Post-Traumatic Nightmares: a Review of Pharmacologic and Nonpharmacologic Treatments Since 2013. Curr Psychiatry Rep. 2018 Oct 11;20(12):108. doi: 10.1007/s11920-018-0971-2. PMID: 30306339. [/mfn]. Posttraumatic nightmares cause higher levels of aggression and helplessness and lead to more nocturnal awakenings and intense arousal than idiopathic nightmares.
Read More About Post-traumatic stress disorder (PTSD) Here
2. Idiopathic nightmares
These types of nightmares do not necessarily replicate events or emotions associated with a traumatic event. Idiopathic nightmares involve well-organized plotlines that tend to be highly imaginative or bizarre. One 2009 study [mfn] Hasler, B., & Germain, A. (2009). Correlates and Treatments of Nightmares in Adults. Sleep medicine clinics, 4(4), 507–517. https://doi.org/10.1016/j.jsmc.2009.07.012 [/mfn] explains “Idiopathic nightmares refer to nightmares with unknown etiology, and unrelated to a specific traumatic event or PTSD.”
According to another 2014 study [mfn] Robert, G., & Zadra, A. (2014). Thematic and content analysis of idiopathic nightmares and bad dreams. Sleep, 37(2), 409–417. https://doi.org/10.5665/sleep.3426 [/mfn], such bad dreams are primarily associated with waking life stressors. However, “the extent to which the content of bad dreams and nightmares reflect the nature of these stressors remains unknown,” explain the researchers. Idiopathic nightmares are believed to be the most common types of disturbed dreaming.
PTSD And Other Comorbid Conditions
Nightmare disorder is associated with various co-occurring disorders, such as –
- Posttraumatic stress disorder (PTSD)
- Borderline personality disorder (BPD)
- Insomnia disorder
- Psychosis
- Mood disorders
- Panic disorders
- Anxiety disorders
- Depression
- Schizophrenia
- Substance abuse
One 2015 study [mfn]Paul, F., Schredl, M., & Alpers, G. W. (2015). Nightmares affect the experience of sleep quality but not sleep architecture: an ambulatory polysomnographic study. Borderline personality disorder and emotion dysregulation, 2, 3. https://doi.org/10.1186/s40479-014-0023-4 [/mfn] explains that “nightmares are a core symptom in posttraumatic stress disorder and about 50% of borderline personality disorder patients suffer from frequent nightmares.” Further research [mfn] Swart ML, van Schagen AM, Lancee J, van den Bout J. Prevalence of nightmare disorder in psychiatric outpatients. Psychother Psychosom. 2013;82(4):267-8. doi: 10.1159/000343590. Epub 2013 Jun 1. PMID: 23735876. [/mfn] reveals that nightmare disorders have been observed in approximately 50-70% of PTSD patients, 49% of BPD patients, around 18.3% of people with insomnia, about 17.5% of depressed people and 16.7% of schizophrenia patients.
This is why the disorder should be diagnosed only when symptoms are severe enough to require independent diagnosis. Moreover, if a person is suffering from PTSD, the nightmare disorder should not be diagnosed additionally, unless it is temporally unrelated to trauma. Research shows that nightmares are the hallmark of PTSD [mfn] Germain A. (2013). Sleep disturbances as the hallmark of PTSD: where are we now?. The American journal of psychiatry, 170(4), 372–382. https://doi.org/10.1176/appi.ajp.2012.12040432 [/mfn]. Experts have found that the condition is closely related to PTSD and both these disorders cause altered activity in the same specific regions in the brain. One 2018 study [mfn] El-Solh A. A. (2018). Management of nightmares in patients with posttraumatic stress disorder: current perspectives. Nature and science of sleep, 10, 409–420. https://doi.org/10.2147/NSS.S166089 [/mfn] reports “PTSD and nightmares are intertwined in such a manner that nightmares strengthen PTSD symptoms, and PTSD in turn causes nightmares.” Chronic nightmares in PTSD can affect physiological and psychological well being and lead to insomnia and disturbed sleep.
Depression [mfn] Beauchemin KM, Hays P. Dreaming away depression: the role of REM sleep and dreaming in affective disorders. J Affect Disord. 1996 Nov 25;41(2):125-33. doi: 10.1016/s0165-0327(96)00080-8. PMID: 8961040. [/mfn] is also associated with nightmares as the patient may have dreams about poor self-image and masochism. Recent research [mfn] Victor I. Spoormaker, Michael Schredl, Jan van den Bout,
Nightmares: from anxiety symptom to sleep disorder, Sleep Medicine Reviews, Volume 10, Issue 1, 2006, Pages 19-31, ISSN 1087-0792, https://doi.org/10.1016/j.smrv.2005.06.001. [/mfn] shows that repeated nightmares and nocturnal awakenings are also associated with psychopathology and neuroticism [mfn] Blagrove M, Farmer L, Williams E. The relationship of nightmare frequency and nightmare distress to well-being. J Sleep Res. 2004 Jun;13(2):129-36. doi: 10.1111/j.1365-2869.2004.00394.x. PMID: 15175092. [/mfn]. People affected by dissociative disorders and schizophrenia may experience nightmares during relapse. Panic disorder patients can suffer from panic attacks during REM sleep. This can be a serious problem for patients with asthma and other breathing disorders. Moreover, a patient may misuse substances like alcohol, drugs and sleeping pills in an attempt to self-medicate and cope with the sleep disturbances, which can worsen the symptoms.
Symptoms Of Nightmare Disorder
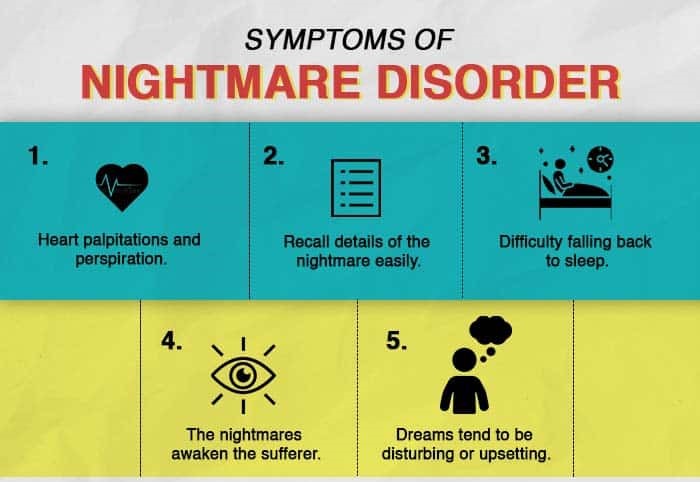
Nightmare episodes are usually brief but may occur multiple times during a night. They can occur frequently or rarely and may cause the person to awaken suddenly. They may have trouble going back to sleep. Moreover, parents or caregivers with children experiencing frequent nightmares can experience significant distress, sleep disturbances and fatigue. Here are some of the common signs and symptoms of nightmare disorder:
- Dreams appear real and vivid. Dreams tend to be disturbing or upsetting and may become increasingly threatening as they progress.
- The “storyline” of the nightmares are typically associated with disturbing themes, like threats to survival or personal safety
- The nightmares awaken the sufferer
- They tend to feel highly alert and experience a range of negative emotions after waking up, such as fear, anxiety, sadness, disgust, anger or and other dysphoric emotions due to the dream
- Heart palpitations and perspiration
- Recall details of the nightmare easily
- Difficulty falling back to sleep due to distress caused by the nightmares
The sufferer may often shout, scream or yell during an episode. The nightmares may cause significant distress and can disrupt or prevent the person from carrying out normal daily tasks. Moreover, stress, anxiety, fear and sleep deprivation due to terrifying dreams can adversely affect their performance at work or school. This can also affect their personal and social relationships as well. It is best to consult a mental health professional if a person experiences these nightmare symptoms. The condition can also cause certain negative consequences, such as –
- Intense fear or anxiety
- Insomnia, sleep avoidance and deprivation
- Daytime sleepiness and fatigue
- Reduced cognitive & emotional functioning
- Embarrassment
- Physical aggression and injury
- Depression
- Relationship or marital problems
However, to be considered as a nightmare, the following criteria should be met:
- Repeated occurrences of well-remembered and dysphoric dreams.
- Occurring during the second half of a sleep episode.
- Difficulty with memory and concentration.
- Intrusive thoughts about the themes and images of the nightmares.
- Feeling sleepy, exhaustion or fatigue during the day.
- Severe impairment or distress, like intense fear or anxiety, during the daytime.
- Behaviour problems, intense anxiety or fear during bedtime.
- Fear of the dark or worried about having another nightmare.
- Clinically significant impairment in daily functioning related to education, career or social situations.
- The symptoms are not caused by other medical or psychiatric conditions or substance abuse.
Causes Of Nightmare Disorder
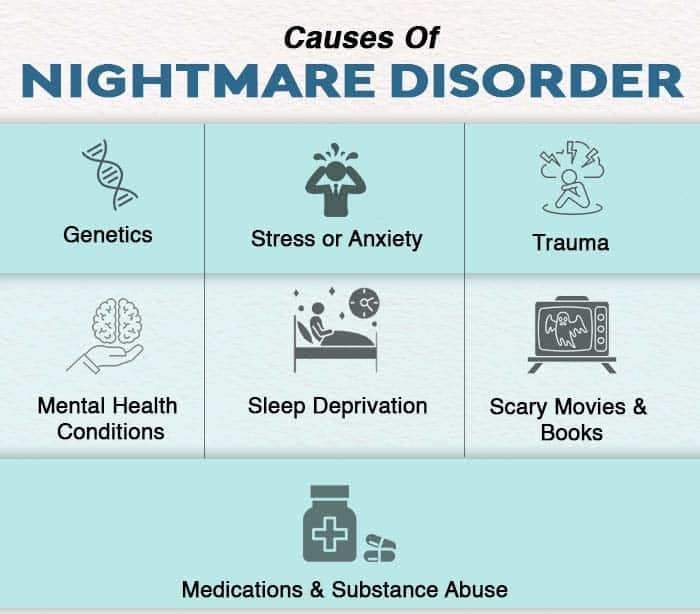
Although the precise cause for the development of this condition has not been identified yet, here are some factors that may influence the development of nightmare disorder:
1. Genetics
The disorder may have a genetic predisposition as it may run in families. Studies [mfn] Hublin C, Kaprio J, Partinen M, Koskenvuo M. Nightmares: familial aggregation and association with psychiatric disorders in a nationwide twin cohort. Am J Med Genet. 1999 Aug 20;88(4):329-36. doi: 10.1002/(sici)1096-8628(19990820)88:4<329::aid-ajmg8>3.0.co;2-e. PMID: 10402498. [/mfn] have found that if a first-degree relative has frequent nightmares, then other family members have higher chance of having this condition.
2. Stress or anxiety
Daily life stressors are also a contributing factor as experiencing anxiety and stress on a regular basis can increase the likelihood of having nightmares. Nightmares may be a coping mechanism to deal with stressful events, according to a study [mfn] Scarpelli S, Bartolacci C, D’Atri A, Gorgoni M, De Gennaro L. Mental Sleep Activity and Disturbing Dreams in the Lifespan. Int J Environ Res Public Health. 2019 Sep 29;16(19):3658. doi: 10.3390/ijerph16193658. PMID: 31569467; PMCID: PMC6801786. [/mfn].
Read More About Generalized Anxiety Disorder Here
3. Trauma
Traumatic experiences, especially the ones experienced during childhood, are one of the major reasons for the onset of this condition. Researchers [mfn] Pagel JF. Nightmares and disorders of dreaming. Am Fam Physician. 2000 Apr 1;61(7):2037-42, 2044. PMID: 10779247. [/mfn] believe that patients with post-traumatic stress disorder (PTSD) experience frequent nightmares after the occurrence of a traumatic event like abuse or an accident.
4. Mental health conditions
Repeated nightmares may often be caused by certain underlying psychiatric disorders, like PTSD, depression, borderline personality disorder, schizophrenia, personality disorders, paranoia etc. Moreover, various other medical conditions such as cancer and heart disease are also associated with this condition as they can disrupt sleep.
5. Medications & substance abuse
Taking certain medications, such as antidepressants, beta-blockers, and medications for Parkinson’s disease or blood pressure can induce nightmares, found studies [mfn] Pagel JF, Helfter P. Drug induced nightmares–an etiology based review. Hum Psychopharmacol. 2003 Jan;18(1):59-67. doi: 10.1002/hup.465. PMID: 12532316. [/mfn]. Moreover, excessive consumption of caffeine, alcohol and recreational drugs can also trigger nightmares. Substance abuse and withdrawal are believed to be a significant factor in the development of nightmare disorder.
6. Sleep deprivation
Insomnia, lack of sleep, sleep disturbances and changes in our sleep schedule can often affect our sleeping and waking routines which can influence the onset of sleep disorders and frequent nightmares.
7. Scary movies & books
Some individuals can experience repeated nightmares after reading or watching scary fiction or real-life scary events, like school shootings, bombings etc. Nightmares can intensify if a person is exposed to such content right before bed.
Read More About The Causes Of Nightmare Disorder Here
Diagnosis Of Nightmare Disorder
Although nightmares are common in children, most adults can also have recurrent nightmares at times. It is crucial that you consult a doctor if these terrifying dreams persist for a long time, affect your sleep patterns, impact your health and impair your daily functioning. The diagnosis process for this condition may involve the following elements:
1. Diagnostic criteria
A doctor will use the diagnostic criteria outlined by the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) to determine whether you have nightmare disorder or not. The DSM-5 diagnostic criteria for nightmare disorder includes the following:
A. Frequent incidences of well-remembered and intensely dysphoric dreams about attempts to escape or avoid various threats to “survival, security, or physical integrity.” These terrifying dreams mostly occur during the latter half of a sleep episode.
B. Upon waking from the nightmares or dysphoric dreams, the sufferer quickly becomes alert and oriented.
C. The nightmares and sleep disturbances result in clinically notable distress and impairment in important areas of daily functioning, such as work, education, relationships or social interaction.
D. The symptoms of nightmare disorder are not caused by the physiological effects of medication, alcohol, drug abuse or other substances.
E. The dysphoric dreams and related symptoms cannot be properly explained by co-existing or comorbid mental or medical disorders.
The doctor may also ask you different questions related to your medical history, family history, use of over-the-counter or prescription medications, supplements, alcohol, drugs and other substances.
2. Specifiers
A doctor or mental health professional, such as a psychiatrist or a psychologist, may add certain specifiers to determine the duration & severity of the condition to make an accurate diagnosis.
The specifiers for duration may include:
- Acute: The duration of the period of nightmares is less than or at least 1 month.
- Subacute: The duration of the period of nightmares is more than 1 month, however, should not be less than 6 months.
- Persistent: The duration of the period of nightmares is at least 6 months or more.
Clinicians may rate the severity of the condition by the frequency of occurrence of nightmares, such as –
- Mild: Occurrence of less than 1 episode each week on average.
- Moderate: Occurrence of 1 or more episodes each week, but less than daily.
- Severe: Occurrence of 1 or more episodes daily.
3. Assessment tools
Although there are no particular tests to diagnose nightmares or nightmare disorder, various instruments may be used by healthcare professionals to assess and evaluate nightmare frequency and distress. According to research [mfn] Gieselmann, A., Ait Aoudia, M., Carr, M., Germain, A., Gorzka, R., Holzinger, B., Kleim, B., Krakow, B., Kunze, A. E., Lancee, J., Nadorff, M. R., Nielsen, T., Riemann, D., Sandahl, H., Schlarb, A. A., Schmid, C., Schredl, M., Spoormaker, V. I., Steil, R., van Schagen, A. M., … Pietrowsky, R. (2019). Aetiology and treatment of nightmare disorder: State of the art and future perspectives. Journal of sleep research, 28(4), e12820. https://doi.org/10.1111/jsr.12820 [/mfn], some common assessment tools used by clinicians may include –
- The Nightmare Frequency Questionnaire (NFQ)
- The Mannheim Dream Questionnaire (MADRE)
- The Nightmare Distress Questionnaire (NDQ)
- The Nightmare Effects Survey (NES)
- The Trauma-Related Nightmare Survey (TRNS)
- The Disturbing Dream and Nightmare Severity Index (DDNSI)
- The Nightmare Effects Questionnaire (NEQ)
- The Van Dream Anxiety Scale (VDAS)
- The Nightmare Behavior Questionnaire (NBQ)
Apart from these, a subscale of the SLEEP‐50 may also be used to evaluate nightmare distress in accordance with DSM‐IV criteria for nightmare and the disorder. Moreover, a sleep questionnaire [mfn] Li, S. X., Zhang, B., Li, A. M., & Wing, Y. K. (2010). Prevalence and correlates of frequent nightmares: a community-based 2-phase study. Sleep, 33(6), 774–780. https://doi.org/10.1093/sleep/33.6.774 [/mfn] can also be used to assess factors like nightmares, trouble initiating sleep, trouble maintaining sleep, restless sleep, early morning awakening, morning headache and daytime fatigue. The doctor may also conduct a nocturnal sleep study, also known as polysomnography [mfn] Phelps AJ, Kanaan RAA, Worsnop C, Redston S, Ralph N, Forbes D. An Ambulatory Polysomnography Study of the Post-traumatic Nightmares of Post-traumatic Stress Disorder. Sleep. 2018 Jan 1;41(1). doi: 10.1093/sleep/zsx188. PMID: 29182727. [/mfn]. The patient may be required to spend a night in a sleep laboratory while the doctor monitors different functions of the patient, such as –
- Brain waves
- Breathing
- Eye movements
- Heartbeat
- Blood oxygen levels
- Muscle tension
- Leg movements
Sensors placed on the patient monitor and record their brain waves, eye movements, heart rate and leg movements as they sleep. The patient may also be videotaped to better analyze the behaviour during sleep cycles. One study [mfn] Bloch KE. Polysomnography: a systematic review. Technol Health Care. 1997 Oct;5(4):285-305. PMID: 9429270. [/mfn] explains “Polysomnography refers to the continuous monitoring of multiple neurophysiological and cardiorespiratory variables, usually over the course of a night, to study normal and disturbed sleep.” The doctor may conduct some additional tests to make sure that the symptoms are not caused by other underlying conditions or co-occurring conditions such as anxiety, PTSD etc.
When To See A Doctor?
Although it is normal to have nightmares occasionally, repeated nightmares may be a cause for concern. Chronic dysphoric dreams can indicate the onset of nightmare disorder. You should consult a doctor or a mental health professional if nightmares :
- Occur more than once a week
- Persist over time
- Regularly disrupt your sleep
- Cause anxiety & fear about bedtime or going to sleep
- Affect your mood and behaviour
- Cause difficulty in daily daytime functioning
- Occur when starting a new medication
You may also maintain a daily sleep diary and keep track of your nightmares, feelings and thoughts associated with sleep disruptions. This can help the doctor get a better idea about your condition.
Nightmare Disorder And Suicide
According to a 2015 study [mfn] Paul, F., Schredl, M., & Alpers, G. W. (2015). Nightmares affect the experience of sleep quality but not sleep architecture: an ambulatory polysomnographic study. Borderline personality disorder and emotion dysregulation, 2, 3. https://doi.org/10.1186/s40479-014-0023-4 [/mfn], nightmares cause significant impairment leading to “waking distress, negative mood, non-restorative sleep and tiredness during the day.” Hence, repeated and frequent nightmares can result in suicidal ideation and behaviour. Sleep disturbances and nightmares have been identified as one of the strong predictors of suicidal behaviour among young individuals. “Both insomnia symptoms and nightmares were associated with an increased likelihood of reporting suicidal ideation (independent of depression),” found researchers from a 2018 study [mfn] Russell, K., Rasmussen, S., & Hunter, S. C. (2018). Insomnia and Nightmares as Markers of Risk for Suicidal Ideation in Young People: Investigating the Role of Defeat and Entrapment. Journal of clinical sleep medicine : JCSM : official publication of the American Academy of Sleep Medicine, 14(5), 775–784. https://doi.org/10.5664/jcsm.7104 [/mfn]. Nightmares can often lead to feelings of entrapment and defeat in young people with insomnia and/or nightmares.
However, the relationship between nightmare disorder and suicide is not limited to young sufferers only, as the general population suffering from nightmares are also related to suicide risk. People experiencing frequent nightmares have 105% higher risk of suicide, while people with occasional nightmares have 57% higher chances as compared to people with no nightmares at all.
Suicide risk is also high in individuals who have PTSD and experience nightmares as well. A 2017 study [mfn] Sandman, N., Valli, K., Kronholm, E., Vartiainen, E., Laatikainen, T., & Paunio, T. (2017). Nightmares as predictors of suicide: an extension study including war veterans. Scientific reports, 7, 44756. https://doi.org/10.1038/srep44756 [/mfn] states “The common denominator between the frequency of nightmares and an increased risk for suicide may be a history of trauma.” Authors of a 2016 study [mfn] Nadorff, M. R., Pearson, M. D., & Golding, S. (2016). Explaining the Relation between Nightmares and Suicide. Journal of clinical sleep medicine : JCSM : official publication of the American Academy of Sleep Medicine, 12(3), 289–290. https://doi.org/10.5664/jcsm.5564 [/mfn] explain “Given that nightmares are that disturbing to the nightmare sufferer, it should not be surprising that nightmares have been found to be associated with suicidal thoughts, attempts, and death by suicide.” However, the psychological process through which nightmares lead to suicidal ideation is not yet well understood.
Some common suicide warning signs for patients with nightmare disorder include:
- Talking about death, suicide or self-harm repeatedly
- Feelings of hopelessness and helplessness
- Severe insomnia or changes in sleeping habits or sleep avoidance
- Changes in appetite and weight
- Isolation & social withdrawal
- Occupied with macabre or morbid themes
- Alcohol or substance abuse
- Looking for methods to commit suicide
If you or your loved one is having suicidal thoughts then make sure to talk to a trusted friend or a family member and seek medical help. Call a suicide helpline or consult a doctor, mental health professional immediately.
Treatment Of Nightmare Disorder
Seeking treatment for nightmares is exceptionally important as it can help the sufferer and their family members to live a healthier and better life, especially if repeated nightmares are causing harmful effects and suicidal ideation. Treatment can help a patient identify any underlying psychiatric conditions and treat them along with the nightmares.
As the treatment plan may include both psychotherapy & medications, it is crucial that you consult a doctor or a mental health professional, like a psychiatrist or a psychologist. Depending on the individual’s health, symptoms, causes and other co-occurring disorders, the doctor can devise an effective treatment plan.
Some of the most helpful treatment options available for nightmare disorder includes:
1. Psychotherapy
Psychotherapy, also known as talk therapy, is considered as one of the most beneficial forms of treatment for nightmares as it helps to recognize and reform negative thoughts and behavior patterns. A therapist can encourage the patient to talk about their nightmares and associated feelings that cause discomfort in a safe environment. The following therapy options are mostly recommended for this disorder:
A. Cognitive Behavioral Therapy (CBT)
Experts believe that Cognitive Behavioral Therapy (CBT) is the most helpful and effective therapy technique for this condition. CBT focuses on the thoughts, emotions, moods and behaviors of the patients and helps them cope with distorted thoughts and behavior. This is a goal-oriented approach for coping with negative emotions, dysfunctional thoughts and counterproductive behavior.
According to a 2019 study [mfn] Sheaves B, Holmes EA, Rek S, Taylor KM, Nickless A, Waite F, Germain A, Espie CA, Harrison PJ, Foster R, Freeman D. Cognitive Behavioural Therapy for Nightmares for Patients with Persecutory Delusions (Nites): An Assessor-Blind, Pilot Randomized Controlled Trial. Can J Psychiatry. 2019 Oct;64(10):686-696. doi: 10.1177/0706743719847422. Epub 2019 May 26. PMID: 31129983; PMCID: PMC6783669. [/mfn], “CBT for nightmares is feasible and may be efficacious for treating nightmares and comorbid insomnia for patients,” over a period of 4 weeks. Another 2016 study [mfn] Levrier, K., Marchand, A., Belleville, G., Dominic, B. P., & Guay, S. (2016). Nightmare Frequency, Nightmare Distress and the Efficiency of Trauma-Focused Cognitive Behavioral Therapy for Post-Traumatic Stress Disorder. Archives of trauma research, 5(3), e33051. https://doi.org/10.5812/atr.33051 [/mfn] revealed that CBT tends to have a positive impact on patients with nightmare disorder with about 77% of patients experiencing a reduction in frequent nightmares.
One 2008 research [mfn] Lancee, J., Spoormaker, V. I., Krakow, B., & van den Bout, J. (2008). A systematic review of cognitive-behavioral treatment for nightmares: toward a well-established treatment. Journal of clinical sleep medicine : JCSM : official publication of the American Academy of Sleep Medicine, 4(5), 475–480. [/mfn] additionally found that nightmare-focused CBT tends to be more effective than other forms of treatment, especially for reducing nightmares and improving sleep quality. The study states “While indirect CBT such as recording and relaxation are effective in reducing nightmares (but not associated complaints), nightmare-focused CBT demonstrated better results on all outcomes, most notably the techniques of exposure and IRT.”
B. Other therapies
Different types of therapy techniques can help the patient to deal with the distressing events related to their nightmares. A 2018 study [mfn] Morgenthaler, T. I., Auerbach, S., Casey, K. R., Kristo, D., Maganti, R., Ramar, K., Zak, R., & Kartje, R. (2018). Position Paper for the Treatment of Nightmare Disorder in Adults: An American Academy of Sleep Medicine Position Paper. Journal of clinical sleep medicine : JCSM : official publication of the American Academy of Sleep Medicine, 14(6), 1041–1055. https://doi.org/10.5664/jcsm.7178 [/mfn] suggests these following forms of therapies for the treatment of nightmare disorder:
- Cognitive behavioural therapy
- Exposure, relaxation, and rescripting therapy
- Hypnosis
- Lucid dreaming therapy
- Progressive deep muscle relaxation
- Sleep dynamic therapy
- Self-exposure therapy
- Systematic desensitization
2. Medications
Medication may also be prescribed for nightmare disorder, but it is mostly not recommended as therapy is considered as the first-line of treatment. However, when symptoms seem severe, medications may be prescribed, especially when therapy is not helpful. Medications are particularly used for treating PTSD-related nightmares. But as certain medications can cause side-effects in some patients, it is important that you consult a doctor before taking any medicine. Mostly, antidepressants, anti-anxiety medication or antipsychotic drugs are recommended as these impact the nervous system.
According to research, the alpha-blocker prazosin is considered as the most effective drug for treating nightmares and nightmare disorder. A recent 2020 study [mfn] Zhang Y, Ren R, Sanford LD, Yang L, Ni Y, Zhou J, Zhang J, Wing YK, Shi J, Lu L, Tang X. The effects of prazosin on sleep disturbances in post-traumatic stress disorder: a systematic review and meta-analysis. Sleep Med. 2020 Mar;67:225-231. doi: 10.1016/j.sleep.2019.06.010. Epub 2019 Jun 22. PMID: 31972510; PMCID: PMC6986268. [/mfn] which considered effects of prazosin on nightmares and sleep quality found that “the use of prazosin was associated with an improvement of nightmare symptoms.” Apart from this, there are several other medications [mfn] Aurora, R. N., Zak, R. S., Auerbach, S. H., Casey, K. R., Chowdhuri, S., Karippot, A., Maganti, R. K., Ramar, K., Kristo, D. A., Bista, S. R., Lamm, C. I., Morgenthaler, T. I., Standards of Practice Committee, & American Academy of Sleep Medicine (2010). Best practice guide for the treatment of nightmare disorder in adults. Journal of clinical sleep medicine : JCSM : official publication of the American Academy of Sleep Medicine, 6(4), 389–401. [/mfn] which may be prescribed for the treatment of nightmare disorder by a doctor, such as:
- Nitrazepam
- Triazolam
- Trazodone
- Nefazodone
- Clonidine
- Atypical antipsychotics (Olanzapine, Risperidone, Aripiprazole)
- Topiramate
- Gabapentin
- Tricyclic Antidepressants
However, research reveals that certain medications, like clonazepam and venlafaxine, should not be recommended for this condition as these may make the symptoms worse.
3. Hypnotherapy
Researchers [mfn] Kingsbury SJ. Brief hypnotic treatment of repetitive nightmares. Am J Clin Hypn. 1993 Jan;35(3):161-9. doi: 10.1080/00029157.1993.10403000. PMID: 8434562. [/mfn] consider hypnotherapy as one of the most effective ways to cure nightmares in patients who do not respond to psychotherapy or medications. Hypnosis [mfn] Ng BY, Lee TS. Hypnotherapy for sleep disorders. Ann Acad Med Singap. 2008 Aug;37(8):683-8. PMID: 18797562. [/mfn] is a trance-like mental state which makes the patient open to positive suggestions and enables them to concentrate on specific thoughts & emotions. This can help them experience deep relaxation and overcome anxiety related to nightmares. Studies have found that 71% of patients respond positively to hypnosis.
Read more: Treatment For Nightmare Disorder
Self-Help Strategies For Nightmare Disorder
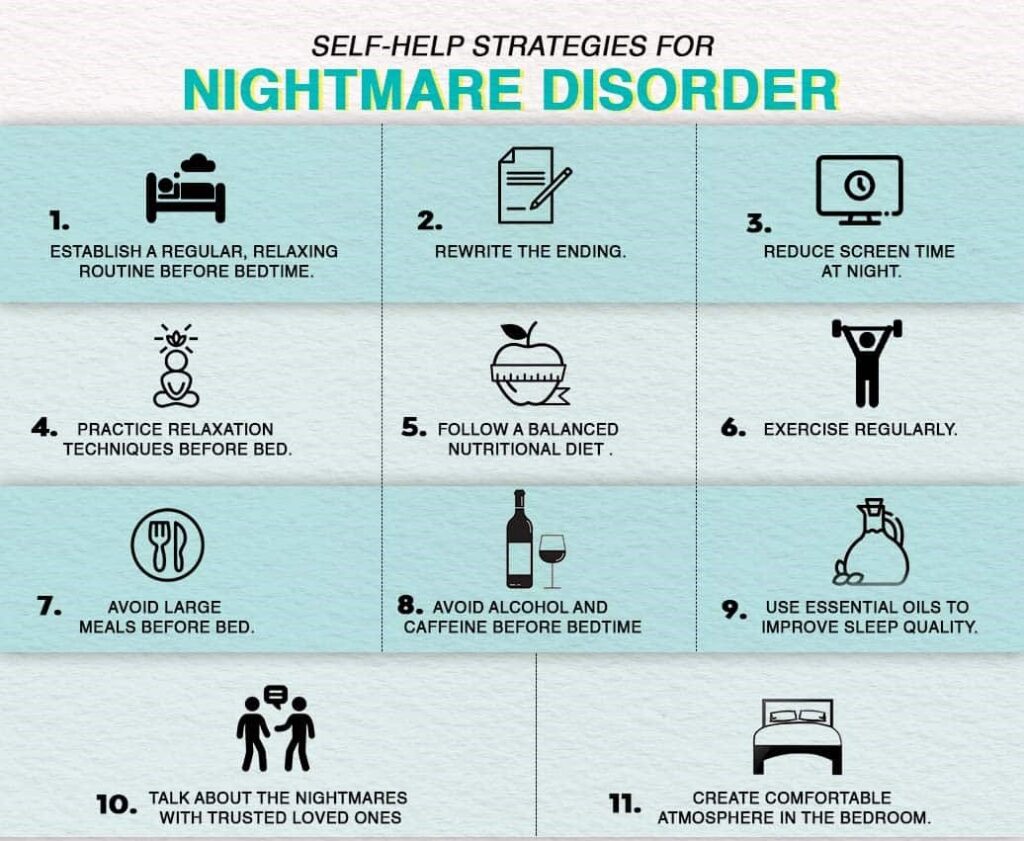
In addition to psychotherapy and medications, certain coping strategies can also help someone reduce nightmares and overcome the disorder in the long run. Here are some self-help strategies for nightmares disorder:
- Practice good sleep hygiene and follow a daily bedtime routine. Establish calming and relaxing routines and habits around bedtime.
- Create a calming and comfortable atmosphere in the bedroom.
- Avoid large meals, work, exercise & technology before bed.
- Practice relaxation techniques like deep breathing, meditation, yoga, relaxation exercises and other calming activities like reading or taking a warm bath before bed.
- Rewrite the ending of the nightmare and think about a happier ending. You may also write a journal about it.
- Talk about the stress, anxiety and fear associated with the nightmares with trusted loved ones or see a doctor or mental health professional.
- Avoid stimulants like alcohol and caffeine before bedtime as these may worsen nightmares.
- Avoid using a smartphone, laptop or tablet before bed and reduce screen time at night.
- Exercise regularly and stay physically active throughout the week.
- Use herbs like valerian, passion flowers and hops to relax your mind & body and improve sleep quality. Essential oils of roman chamomile, vetiver and lavender can also be helpful.
- Follow a balanced nutritional diet including tomatoes, mustard seeds, cherries, chillies, goji berries, sprouted seeds, fenugreek, lupin, rice and corn.
Prognosis For Nightmare Disorder
According to research [mfn] Moturi S, Avis K. Assessment and treatment of common pediatric sleep disorders. Psychiatry (Edgmont). 2010 Jun;7(6):24-37. PMID: 20622943; PMCID: PMC2898839. [/mfn], the prognosis for this condition appears to be very good. With psychological interventions and pharmacologic treatments, the symptoms can resolve over time, both for children and adults. However, if the symptoms persist then comorbid conditions should be considered, such as PTSD, anxiety disorders etc.
If you are suffering from chronic nightmares leading to sleep disturbances, then make sure to consult a doctor and mental health professional and seek treatment immediately for nightmare disorder or any underlying conditions. With appropriate treatment and coping strategies, complete recovery is possible.
Nightmares And Nightmare Disorder At A Glance
- Nightmare disorder is a psychiatric condition marked by repeated, extremely vivid and distressing nightmares.
- People suffering from this psychological condition experience terrifying nightmares with severe frequency and disruptions in sleep & wakefulness.
- The condition is often caused by stress, anxiety, depression, trauma, medications or substance abuse and other psychiatric disorders.
- Although nightmares usually begin by age 10, these disturbing psychological experiences may occur at any age.
- At least 5.1% of people experience a nightmare.
- Chronic dysphoric dreams can indicate the onset of nightmare disorder.
- Sleep disturbances and nightmares have been identified as one of the strong predictors of suicidal behavior among young individuals.
- Under the supervision of a medical professional, treatment involving psychotherapy & medications can prove helpful.




Leave a Reply