Anorexia Nervosa is a life-threatening eating disorder characterized by self-starvation and an intense fear of gaining weight. This disorder is often diagnosed when a person weighs at least 15% less than their ideal weight. The term “anorexia” means “loss of appetite”.
Anorexia Nervosa And The “Ideal Weight”
Most people with anorexia nervosa restrict their food intake in order to prevent weight gain. They tend to control their calorie intake by vomiting right after eating or using laxatives, diet aids, or herbal products. Excessive exercising is also a known trait of people with anorexia. They eat an extremely low-calorie diet due to their excessive fear of gaining weight.
People with this condition are often hungry but refuse to intake food in order to maintain their “ideal weight”. A 2006 study 1 Hoek HW. Incidence, prevalence and mortality of anorexia nervosa and other eating disorders. Curr Opin Psychiatry. 2006 Jul;19(4):389-94. doi: 10.1097/01.yco.0000228759.95237.78. PMID: 16721169. found this disorder to be the highest mortality of any psychiatric disorder. Studies 2 Morris, J., & Twaddle, S. (2007). Anorexia nervosa. BMJ (Clinical research ed.), 334(7599), 894–898. https://doi.org/10.1136/bmj.39171.616840.BE found that the prevalence rate of this disorder is about 0.3%. A 2014 study 3 Universite de Montreal. (2014, October 8). Childhood eating difficulties could be a sign of underlying psychological issues. ScienceDaily. Retrieved May 28, 2021 from www.sciencedaily.com/releases/2014/10/141008083159.htm confirmed that it is the most common chronic condition among teens. This condition is more common in females than in males.
Read More About Anorexia Nervosa Here
The Primary Goals Of Treatment
The primary goal of treatment is to restore the bodyweight of the individual and adopt healthy eating habits to avoid any severe illness. The core treatment goals of this disorder are as follows:
- Achieving and maintaining a normal, healthy, and stable body weight
- Halting all abnormal eating behaviors such as food intake restriction, binge eating, purging, or compulsive exercise
- Discarding the core overvalued beliefs around body weight
- Treating comorbid conditions both psychiatric and medical
- Planning for relapse prevention
The main form of treatment is a combination of therapy and medications. A 2001 study 4 Löwe B, Zipfel S, Buchholz C, Dupont Y, Reas DL, Herzog W. Long-term outcome of anorexia nervosa in a prospective 21-year follow-up study. Psychol Med. 2001 Jul;31(5):881-90. doi: 10.1017/s003329170100407x. PMID: 11459385. demonstrated a full recovery even after 21 years of chronic severe anorexia nervosa. There are several treatment methods for Anorexia nervosa that are adopted to help ease the symptoms of the condition. They include:
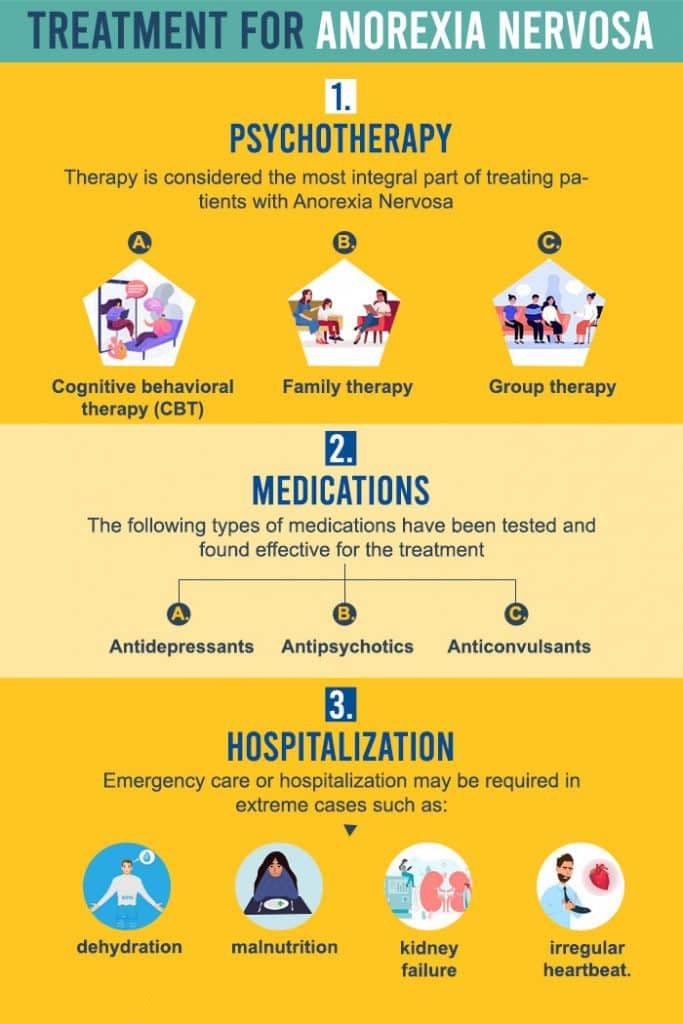
1. Psychotherapy
Therapy is considered the most integral part of treating patients with Anorexia Nervosa. A 2005 study 5 Fairburn CG. Evidence-based treatment of anorexia nervosa. Int J Eat Disord. 2005;37 Suppl:S26-30; discussion S41-2. doi: 10.1002/eat.20112. PMID: 15852315. found significant results in treating patients with eating disorders including anorexia with therapy. The psychotherapy treatment methods that are usually adopted are as follows:
A. Cognitive behavioral therapy (CBT)
CBT may be done in groups or individually. Cognitive behavioral therapy involves the identification of negative thoughts and patterns that govern unhealthy eating behavior. These unhealthy thoughts are then replaced by positive ones to reach the desired goal of eating healthy. The therapist also helps the patient to develop healthy coping strategies to manage the symptoms of the disorder. The goal of this form of therapy is to understand the underlying issues that are triggering unhealthy eating behaviors.
This also includes addressing the traumatic experiences that cause them to resort to such extreme eating behaviours. A 2008 study 6 Bowers WA, Ansher LS. The effectiveness of cognitive behavioral therapy on changing eating disorder symptoms and psychopathology of 32 anorexia nervosa patients at hospital discharge and one year follow-up. Ann Clin Psychiatry. 2008 Apr-Jun;20(2):79-86. doi: 10.1080/10401230802017068. PMID: 18568579. reported cognitive behavioural therapy as an effective form of treatment for Anorexia Nervosa and other forms of eating disorders.
Read More About Cognitive behavioral therapy Here
B. Family therapy
Family therapy is often used to improve communication and resolve conflicts among family members. Family therapy can be helpful for the treatment of Anorexia nervosa since family members can help keep track of their eating habits and lifestyle. A study 7 Eisler I, Dare C, Hodes M, Russell G, Dodge E, Le Grange D. Family therapy for adolescent anorexia nervosa: the results of a controlled comparison of two family interventions. J Child Psychol Psychiatry. 2000 Sep;41(6):727-36. PMID: 11039685. showed significant improvements in the behavior of the patient when therapy with family members was involved. Family members can also benefit from this therapy since the therapist also develops coping strategies on how to deal with the individual experiencing this condition. This therapy also helps to bring a family closer together by addressing their unresolved conflicts.
C. Group therapy
Group therapy usually involves several individuals coming together as a group to address similar issues and helping each other develop coping strategies to manage the symptoms. A psychiatrist or a therapist may also be involved in group therapy sessions. Group therapy also helps to develop socialization techniques. However, a report 8 Morris, J., & Twaddle, S. (2007). Anorexia nervosa. BMJ (Clinical research ed.), 334(7599), 894–898. https://doi.org/10.1136/bmj.39171.616840.BE suggested little evidence that group therapy being beneficial to patients with anorexia.
Read More About Group Therapy Here
2. Medications
The following types of medications have been tested and found effective for the treatment of eating disorders:
- Antidepressants
- Antipsychotics
- Anticonvulsants
- Prokinetic agents
- Opiate antagonists
- Appetite suppressants
- Tetrahydrocannabinol
- Cyproheptadine
- Zinc
- Ondansetron
Evidence 9 Vaswani M, Kalra H. Selective serotonin re-uptake inhibitors in anorexia nervosa. Expert Opin Investig Drugs. 2004 Apr;13(4):349-57. doi: 10.1517/13543784.13.4.349. PMID: 15102585. suggests that fluoxetine may be beneficial in relapse prevention after restoring weight. A 2004 study 10 Powers PS, Santana C. Available pharmacological treatments for anorexia nervosa. Expert Opin Pharmacother. 2004 Nov;5(11):2287-92. doi: 10.1517/14656566.5.11.2287. PMID: 15500375. also found Cyproheptadine has shown significant benefits in relapse prevention. Antidepressants may be prescribed to treat comorbid conditions such as depression or anxiety. However, it is important to understand that medications cannot diminish the intense desire to lose weight.
3. Hospitalization
Emergency care or hospitalization may be required in extreme cases such as dehydration, malnutrition, kidney failure, or an irregular heartbeat. Some people are hospitalized due to the severity of their weight loss practices. Binging and vomiting in low weight can greatly increase mortality when compared to restrictive starvation diets.
A 2005 study 11 Birmingham CL, Su J, Hlynsky JA, Goldner EM, Gao M. The mortality rate from anorexia nervosa. Int J Eat Disord. 2005 Sep;38(2):143-6. doi: 10.1002/eat.20164. PMID: 16134111. reported the annual mortality for Anorexia Nervosa was 5.10 deaths per 1000 person-years, out of which 1.3 resulted from suicide. If the patient doesn’t receive the proper care they are at high risk of irreversible damage that involves acute illness, immune function, cardiovascular function, fertility, or bone density. Reports 12 De Filippo E, Signorini A, Bracale R, Pasanisi F, Contaldo F. Hospital admission and mortality rates in anorexia nervosa: experience from an integrated medical-psychiatric outpatient treatment. Eat Weight Disord. 2000 Dec;5(4):211-6. doi: 10.1007/BF03354448. PMID: 11216129. found an increased incidence of hospitalization rates for people with anorexia nervosa.
The Road To Recovery
Anorexia nervosa is often found to be a lifelong challenge for some people. However, it is possible to recover from this condition by adopting therapy and medication. The treatment of anorexia nervosa is found to be successful in most cases. But relapses are also common among patients. The patient must follow a nutritious diet that ensures the necessary daily calorie, vitamin, and protein intake. A dietician may also prove helpful in developing a wholesome diet.