Smoking is a harmful practice that can have numerous adverse effects on people’s physical and psychological health. Though many people smoke for experiencing temporary pleasure and coping with stress, regular smoking gradually becomes a life-threatening addiction.
What Is Smoking?
A 2021 research paper [mfn] Adams TN, Morris J. Smoking. [Updated 2021 Feb 21]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK537066/ [/mfn] defines smoking as the practice of inhaling and exhaling the smoke of certain plant-based burning substances into the bloodstream. It is considered to be one of the most significant global public health issues. Though there are numerous plant materials people use as a substance, such as marijuana [mfn] Lafaye, G., Karila, L., Blecha, L., & Benyamina, A. (2017). Cannabis, cannabinoids, and health. Dialogues in clinical neuroscience, 19(3), 309–316. https://doi.org/10.31887/DCNS.2017.19.3/glafaye [/mfn] , cocaine [mfn] Cocaine Research Report. (2016). Drugabuse.gov | National Institute on Drug Abuse (NIDA). https://www.drugabuse.gov/download/1141/cocaine-research-report.pdf?v=3f3fb3f0903dfa8879388c2a5d086cb9 [/mfn] , hashish, the dried leaves of tobacco plants are the most common ones. It contains a high amount of nicotine that causes extreme addiction.
“Nicotine addiction is a complex disorder, habitual use of tobacco and tobacco products continues to be a significant contributor to health problems worldwide, which in part may be related to the increasing affordability of tobacco and nicotine products,” explained the researchers [mfn] Widysanto A, Combest FE, Dhakal A, et al. Nicotine Addiction. [Updated 2021 May 22]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK499915/ [/mfn] . People smoke tobacco in a variety of ways, including in a cigarette, cigar, or pipe. Nicotine refers to an alkaloid that can negatively affect a person’s physiological and psychological well-being. A 2015 study [mfn] Mishra, A., Chaturvedi, P., Datta, S., Sinukumar, S., Joshi, P., & Garg, A. (2015). Harmful effects of nicotine. Indian journal of medical and paediatric oncology : official journal of Indian Society of Medical & Paediatric Oncology, 36(1), 24–31. https://doi.org/10.4103/0971-5851.151771 [/mfn] claims that it causes several premature diseases and deaths worldwide than any other human habit or behavior does.
Tobacco consumption is associated with various physical as well as psychological diseases and disorders, such as:
- Cancer [mfn] Jacob, L., Freyn, M., Kalder, M., Dinas, K., & Kostev, K. (2018). Impact of tobacco smoking on the risk of developing 25 different cancers in the UK: a retrospective study of 422,010 patients followed for up to 30 years. Oncotarget, 9(25), 17420–17429. https://doi.org/10.18632/oncotarget.24724 [/mfn]
- Cardiovascular diseases and stroke [mfn] Lakier J. B. (1992). Smoking and cardiovascular disease. The American journal of medicine, 93(1A), 8S–12S. https://doi.org/10.1016/0002-9343(92)90620-q [/mfn]
- Diabetes [mfn] Chang S. A. (2012). Smoking and type 2 diabetes mellitus. Diabetes & metabolism journal, 36(6), 399–403. https://doi.org/10.4093/dmj.2012.36.6.399 [/mfn]
- Pneumonia [mfn] Baskaran, V., Murray, R. L., Hunter, A., Lim, W. S., & McKeever, T. M. (2019). Effect of tobacco smoking on the risk of developing community acquired pneumonia: A systematic review and meta-analysis. PloS one, 14(7), e0220204. https://doi.org/10.1371/journal.pone.0220204 [/mfn]
- Obstructive pulmonary diseases [mfn] Centers for Disease Control and Prevention (US); National Center for Chronic Disease Prevention and Health Promotion (US); Office on Smoking and Health (US). How Tobacco Smoke Causes Disease: The Biology and Behavioral Basis for Smoking-Attributable Disease: A Report of the Surgeon General. Atlanta (GA): Centers for Disease Control and Prevention (US); 2010. 7, Pulmonary Diseases. Available from: https://www.ncbi.nlm.nih.gov/books/NBK53021/ [/mfn]
- Miscarriages [mfn] Pineles, B. L., Park, E., & Samet, J. M. (2014). Systematic review and meta-analysis of miscarriage and maternal exposure to tobacco smoke during pregnancy. American journal of epidemiology, 179(7), 807–823. https://doi.org/10.1093/aje/kwt334 [/mfn]
- Anxiety and depression [mfn] Fluharty, M., Taylor, A. E., Grabski, M., & Munafò, M. R. (2017). The Association of Cigarette Smoking With Depression and Anxiety: A Systematic Review. Nicotine & tobacco research : official journal of the Society for Research on Nicotine and Tobacco, 19(1), 3–13. https://doi.org/10.1093/ntr/ntw140 [/mfn]
- Schizophrenia [mfn] Lucatch, A. M., Lowe, D., Clark, R. C., Kozak, K., & George, T. P. (2018). Neurobiological Determinants of Tobacco Smoking in Schizophrenia. Frontiers in psychiatry, 9, 672. https://doi.org/10.3389/fpsyt.2018.00672 [/mfn]
- Obsessive-compulsive disorder [mfn] Abramovitch, A., Pizzagalli, D. A., Geller, D. A., Reuman, L., & Wilhelm, S. (2015). Cigarette smoking in obsessive-compulsive disorder and unaffected parents of OCD patients. European psychiatry : the journal of the Association of European Psychiatrists, 30(1), 137–144. https://doi.org/10.1016/j.eurpsy.2013.12.003 [/mfn]
- Panic disorder [mfn] Moylan, S., Jacka, F. N., Pasco, J. A., & Berk, M. (2012). Cigarette smoking, nicotine dependence and anxiety disorders: a systematic review of population-based, epidemiological studies. BMC medicine, 10, 123. https://doi.org/10.1186/1741-7015-10-123 [/mfn]
- Attention deficit hyperactivity disorder [mfn] McClernon, F. J., & Kollins, S. H. (2008). ADHD and smoking: from genes to brain to behavior. Annals of the New York Academy of Sciences, 1141, 131–147. https://doi.org/10.1196/annals.1441.016 [/mfn]
- Bipolar disorder [mfn] Thomson, D., Berk, M., Dodd, S., Rapado-Castro, M., Quirk, S. E., Ellegaard, P. K., Berk, L., & Dean, O. M. (2015). Tobacco use in bipolar disorder. Clinical psychopharmacology and neuroscience : the official scientific journal of the Korean College of Neuropsychopharmacology, 13(1), 1–11. https://doi.org/10.9758/cpn.2015.13.1.1 [/mfn]
- Dementia [mfn] Cataldo, J. K., Prochaska, J. J., & Glantz, S. A. (2010). Cigarette smoking is a risk factor for Alzheimer’s Disease: an analysis controlling for tobacco industry affiliation. Journal of Alzheimer’s disease : JAD, 19(2), 465–480. https://doi.org/10.3233/JAD-2010-1240 [/mfn]
- Eating disorder [mfn] Anzengruber, D., Klump, K. L., Thornton, L., Brandt, H., Crawford, S., Fichter, M. M., Halmi, K. A., Johnson, C., Kaplan, A. S., LaVia, M., Mitchell, J., Strober, M., Woodside, D. B., Rotondo, A., Berrettini, W. H., Kaye, W. H., & Bulik, C. M. (2006). Smoking in eating disorders. Eating behaviors, 7(4), 291–299. https://doi.org/10.1016/j.eatbeh.2006.06.005 [/mfn]
The Psychological Mechanism Of Smoking
Several researchers [mfn] Anzengruber, D., Klump, K. L., Thornton, L., Brandt, H., Crawford, S., Fichter, M. M., Halmi, K. A., Johnson, C., Kaplan, A. S., LaVia, M., Mitchell, J., Strober, M., Woodside, D. B., Rotondo, A., Berrettini, W. H., Kaye, W. H., & Bulik, C. M. (2006). Smoking in eating disorders. Eating behaviors, 7(4), 291–299. https://doi.org/10.1016/j.eatbeh.2006.06.005 [/mfn] and psychologists have examined certain psychological mechanisms that can pose risk factors for tobacco use. They have found that low levels of self-esteem and self-confidence, depressive mood, negative thoughts [mfn] Weinstein, S. M., & Mermelstein, R. J. (2013). Dynamic associations of negative mood and smoking across the development of smoking in adolescence. Journal of clinical child and adolescent psychology : the official journal for the Society of Clinical Child and Adolescent Psychology, American Psychological Association, Division 53, 42(5), 629–642. https://doi.org/10.1080/15374416.2013.794698 [/mfn] , and personal well-being are closely interlinked with tobacco addiction. Smoking is considered the most effective and easiest way of delivering nicotine to the brain.
Studies [mfn] Benowitz N. L. (2009). Pharmacology of nicotine: addiction, smoking-induced disease, and therapeutics. Annual review of pharmacology and toxicology, 49, 57–71. https://doi.org/10.1146/annurev.pharmtox.48.113006.094742 [/mfn] explain that nicotine exerts an influence on multiple brain systems that leads to affecting people’s behavior, personality, feeling, and thinking. There are a variety of reasons why people start using tobacco. A 2004 research [mfn] Jarvis M. J. (2004). Why people smoke. BMJ (Clinical research ed.), 328(7434), 277–279. https://doi.org/10.1136/bmj.328.7434.277 [/mfn] found that most of the reasons are related to changing one’s self-image, portraying oneself as more attractive, and displaying one’s physical and emotional strength. Some of the most common reasons for developing this behavior are:
- On a dare to show that one is not afraid
- Influenced by media and advertisements
- To appear more sophisticated and modern
- Influenced by friends, family members, and relatives
- To protest or defy authority
- To release stress and tension
- To lose weight
Many people think that the habit of smoking can help them to ease out their stress and cope with anxiety and depression. In reality, it is a highly addictive behavior that can have life-threatening impacts on someone’s mental health. People who are habituated to smoke are more likely to experience the symptoms of anxiety and depression compared to non-smokers.
A 2017 research paper [mfn] West R. (2017). Tobacco smoking: Health impact, prevalence, correlates and interventions. Psychology & health, 32(8), 1018–1036. https://doi.org/10.1080/08870446.2017.1325890 [/mfn] says that the worldwide prevalence of tobacco smoking is around 1 billion, where males smoke at higher rates than females, with 30% and 7% prevalence respectively. Studies [mfn] Jha P, MacLennan M, Chaloupka FJ, et al. Global Hazards of Tobacco and the Benefits of Smoking Cessation and Tobacco Taxes. In: Gelband H, Jha P, Sankaranarayanan R, et al., editors. Cancer: Disease Control Priorities, Third Edition (Volume 3). Washington (DC): The International Bank for Reconstruction and Development / The World Bank; 2015 Nov 1. Chapter 10. Available from: https://www.ncbi.nlm.nih.gov/books/NBK343639/ doi: 10.1596/978-1-4648-0349-9_ch10 [/mfn] have estimated that tobacco use kills approximately 5 million people annually worldwide, accounting for over 20% of all deaths of adult men and 5% of deaths of adult women.
Understanding Smoking Addiction
The smoke of burning tobacco contains thousands of harmful chemicals. Research [mfn] Institute of Medicine (US) Committee on Preventing Nicotine Addiction in Children and Youths; Lynch BS, Bonnie RJ, editors. Growing up Tobacco Free: Preventing Nicotine Addiction in Children and Youths. Washington (DC): National Academies Press (US); 1994. 2, THE NATURE OF NICOTINE ADDICTION. Available from: https://www.ncbi.nlm.nih.gov/books/NBK236759/ [/mfn] says that the significant one ‘nicotine’ develops a dangerous addiction in people. Single nicotine inhalation becomes a permanent addiction by going through the following process that includes:
- The smoke gets rapidly absorbed through the lungs into the bloodstream that carries it directly to the heart. A 2010 study [mfn] Benowitz, N. L., Hukkanen, J., & Jacob, P., 3rd (2009). Nicotine chemistry, metabolism, kinetics and biomarkers. Handbook of experimental pharmacology, (192), 29–60. https://doi.org/10.1007/978-3-540-69248-5_2 [/mfn] suggests, when a person inhales the smoke, it reaches the brain within about 10-20 seconds.
- As the nicotine enters the heart directly, it does not get a chance to dissipate. A high concentration of nicotine remains in the lungs and the bloodstream until it reaches the brain.
- According to 2013 research [mfn] Tweed, J. O., Hsia, S. H., Lutfy, K., & Friedman, T. C. (2012). The endocrine effects of nicotine and cigarette smoke. Trends in endocrinology and metabolism: TEM, 23(7), 334–342. https://doi.org/10.1016/j.tem.2012.03.006 [/mfn] , nicotine stimulates the adrenal glands to release the adrenaline hormone in the brain which is solely responsible for developing pleasure and energy.
- A 1997 study [mfn] Haass, M., & Kübler, W. (1997). Nicotine and sympathetic neurotransmission. Cardiovascular drugs and therapy, 10(6), 657–665. https://doi.org/10.1007/BF00053022 [/mfn] explains that nicotine affects the central nervous system and increases one’s blood pressure, breathing, and heart rate. But the feeling of pleasure and energy is temporary.
- Studies [mfn] Bruijnzeel A. W. (2012). Tobacco addiction and the dysregulation of brain stress systems. Neuroscience and biobehavioral reviews, 36(5), 1418–1441. https://doi.org/10.1016/j.neubiorev.2012.02.015 [/mfn] have found, once the nicotine reaches people’s brains, it helps to improve their mood as well as decrease their anger and stress. The nicotine relaxes one’s muscles and reduces appetite.
- Nicotine also activates the dopamine signal [mfn] Benowitz N. L. (2009). Pharmacology of nicotine: addiction, smoking-induced disease, and therapeutics. Annual review of pharmacology and toxicology, 49, 57–71. https://doi.org/10.1146/annurev.pharmtox.48.113006.094742 [/mfn] that leads to a kind of relaxing sensation in the brain. The dopamine release instantly produces a sense of pleasure and happiness in people.
Our body and brain become easily habituated with regular nicotine inhalation. When it becomes an addiction, it leads to certain significant changes in the brain. The human body builds up a high tolerance to nicotine and makes a person need nicotine in higher amounts. The whole process of nicotine reaching people’s brains becomes an up and down cycle that happens over and over and ultimately leads to smoking addiction.
How Smoking Affects The Brain
When a person smokes, nicotine starts to act like the neurotransmitters that are already present in the human brain. A 2011 research [mfn] D’Souza, M. S., & Markou, A. (2011). Neuronal mechanisms underlying development of nicotine dependence: implications for novel smoking-cessation treatments. Addiction science & clinical practice, 6(1), 4–16. [/mfn] explains that the brain decreases the acetylcholine receptors to compensate for the increased signal activity caused by nicotine. This leads to developing nicotine tolerance in the brain. When a person starts to smoke regularly, the nicotine begins to reduce one’s ability to feel pleasure.
It causes the smoker to need more nicotine inhalation to sustain the pleasure. It also activates the reward system [mfn] De Biasi, M., & Dani, J. A. (2011). Reward, addiction, withdrawal to nicotine. Annual review of neuroscience, 34, 105–130. https://doi.org/10.1146/annurev-neuro-061010-113734 [/mfn] of the human brain and increases the levels of dopamine, a chemical messenger that influences rewarding behaviors [mfn] Bromberg-Martin, E. S., Matsumoto, M., & Hikosaka, O. (2010). Dopamine in motivational control: rewarding, aversive, and alerting. Neuron, 68(5), 815–834. https://doi.org/10.1016/j.neuron.2010.11.022 [/mfn] . Research says that certain other chemicals in tobacco products, including acetaldehyde, increases the effects of nicotine in the brain.
It requires more research to detect the effects of smoking on a person’s cognitive abilities. But smoking damages certain areas by causing thinning in some crucial areas. According to a 2015 study [mfn] Karama, S., Ducharme, S., Corley, J., Chouinard-Decorte, F., Starr, J. M., Wardlaw, J. M., Bastin, M. E., & Deary, I. J. (2015). Cigarette smoking and thinning of the brain’s cortex. Molecular Psychiatry, 20(6), 778-785. https://doi.org/10.1038/mp.2014.187 [/mfn] , smokers tend to have a thinner cerebral cortex than others as nicotine destroys the brain’s grey matter. “Smoking is significantly associated with gray matter volume loss in the prefrontal cortex, the anterior cingulate cortex, the insula, and the olfactory gyrus.”, explained by a 2014 research paper [mfn] Fritz, H. C., Wittfeld, K., Schmidt, C. O., Domin, M., Grabe, H. J., Hegenscheid, K., Hosten, N., & Lotze, M. (2014). Current smoking and reduced gray matter volume-a voxel-based morphometry study. Neuropsychopharmacology : official publication of the American College of Neuropsychopharmacology, 39(11), 2594–2600. https://doi.org/10.1038/npp.2014.112 [/mfn] . The cerebral cortex [mfn] Jawabri KH, Sharma S. Physiology, Cerebral Cortex Functions. [Updated 2021 May 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK538496/ [/mfn] is considered extremely crucial for thinking abilities, memory, perception, and learning.
Smoking And Mental Health
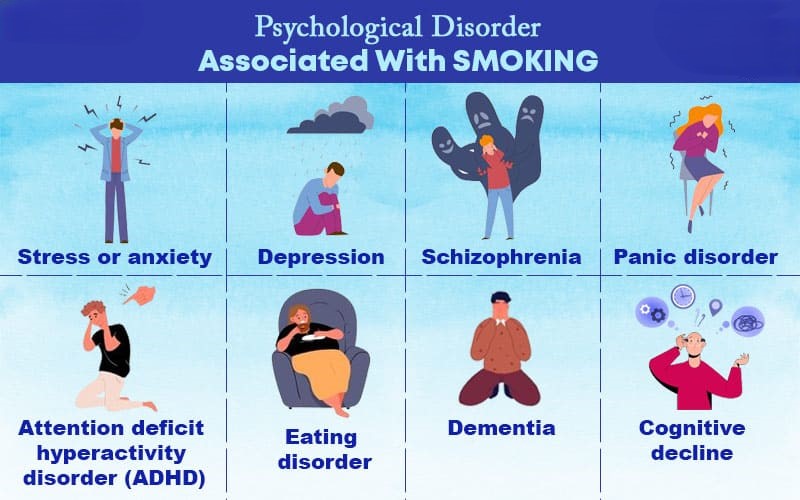
There is a common perception that smoking helps people to cope with stress and anxiety. But the truth is nicotine addiction can have numerous adverse effects on a person’s physical and psychological health. A 2013 study [mfn] Minichino, A., Bersani, F. S., Calò, W. K., Spagnoli, F., Francesconi, M., Vicinanza, R., Delle Chiaie, R., & Biondi, M. (2013). Smoking behaviour and mental health disorders–mutual influences and implications for therapy. International journal of environmental research and public health, 10(10), 4790–4811. https://doi.org/10.3390/ijerph10104790 [/mfn] states that smokers are more likely to suffer from various psychological disorders than non-smokers. Nicotine inhalation provides a boost in confidence and a great sense of achievement at first.
But it gradually reduces the feeling of pleasure once it becomes an addiction. Studies [mfn] Benowitz N. L. (2009). Pharmacology of nicotine: addiction, smoking-induced disease, and therapeutics. Annual review of pharmacology and toxicology, 49, 57–71. https://doi.org/10.1146/annurev.pharmtox.48.113006.094742 [/mfn] have found that nicotine interferes with the functioning of neurotransmitters and exerts several neuroendocrine effects that lead to developing several psychological complications. Nicotine addiction is associated with various significant psychological disorders, including:
1. Stress or anxiety
Many people smoke to ease their feelings of stress. As nicotine offers instant relaxation, people smoke in the belief that it will reduce their anxiety. Once a person finishes smoking, the nicotine level begins to fall in their body. A 2017 research [mfn] Benowitz, N. L., & Burbank, A. D. (2016). Cardiovascular toxicity of nicotine: Implications for electronic cigarette use. Trends in cardiovascular medicine, 26(6), 515–523. https://doi.org/10.1016/j.tcm.2016.03.001 [/mfn] claims that the nicotine level makes their hearts beat faster and increases their blood pressure. One might experience anxiety [mfn] Picciotto, M. R., Brunzell, D. H., & Caldarone, B. J. (2002). Effect of nicotine and nicotinic receptors on anxiety and depression. Neuroreport, 13(9), 1097–1106. https://doi.org/10.1097/00001756-200207020-00006 [/mfn] and intolerable craving for nicotine. It also decreases one’s capability to deal with stress.
Read More About Anxiety Here
2. Depression
Research [mfn] Fluharty, M., Taylor, A. E., Grabski, M., & Munafò, M. R. (2017). The Association of Cigarette Smoking With Depression and Anxiety: A Systematic Review. Nicotine & tobacco research : official journal of the Society for Research on Nicotine and Tobacco, 19(1), 3–13. https://doi.org/10.1093/ntr/ntw140 [/mfn] says that a person with depression tends to get addicted to smoking more than any other person. Many people get addicted to nicotine without showing any symptoms of depression. A 2007 research paper [mfn] Lembke, A., Johnson, K., & DeBattista, C. (2007). Depression and smoking cessation: does the evidence support psychiatric practice?. Neuropsychiatric disease and treatment, 3(4), 487–493. [/mfn] claims that people with depression often struggle a lot and experience severe withdrawal symptoms while quitting smoking. Depression and nicotine addiction are closely associated as smoking often leads to depression, which in turn often encourages one to start smoking. Nicotine stimulates dopamine release that develops a sense of happiness. As depressive people lack positive feelings, they use nicotine to temporarily increase their dopamine supply.
Read More About Major Depressive Disorder ( Depression ) Here
3. Schizophrenia
According to a 2018 study [mfn] Lucatch, A. M., Lowe, D., Clark, R. C., Kozak, K., & George, T. P. (2018). Neurobiological Determinants of Tobacco Smoking in Schizophrenia. Frontiers in psychiatry, 9, 672. https://doi.org/10.3389/fpsyt.2018.00672 [/mfn] , schizophrenia patients are more likely to get addicted to nicotine. As nicotine develops a temporary pleasurable feeling, research [mfn] Quigley, H., & MacCabe, J. H. (2019). The relationship between nicotine and psychosis. Therapeutic advances in psychopharmacology, 9, 2045125319859969. https://doi.org/10.1177/2045125319859969 [/mfn] says that it may seem to reduce some of the symptoms of schizophrenia or the side effects of medicines used for the treatment. A 2013 research [mfn] Fotuhi, O., Fong, G. T., Zanna, M. P., Borland, R., Yong, H. H., & Cummings, K. M. (2013). Patterns of cognitive dissonance-reducing beliefs among smokers: a longitudinal analysis from the International Tobacco Control (ITC) Four Country Survey. Tobacco control, 22(1), 52–58. https://doi.org/10.1136/tobaccocontrol-2011-050139 [/mfn] explains that tobacco may improve concentration and decrease the unpleasant hyperstimulation experienced by schizophrenia patients. But studies [mfn] Kendler, K. S., Lönn, S. L., Sundquist, J., & Sundquist, K. (2015). Smoking and schizophrenia in population cohorts of Swedish women and men: a prospective co-relative control study. The American journal of psychiatry, 172(11), 1092–1100. https://doi.org/10.1176/appi.ajp.2015.15010126 [/mfn] have shown that nicotine may increase the risk of schizophrenia.
Read More About Schizophrenia Here
4. Panic disorder
A 2018 research paper [mfn] Farris, S. G., Brown, L. A., Goodwin, R. D., & Zvolensky, M. J. (2017). Panic attack history and smoking topography. Drug and alcohol dependence, 171, 84–90. https://doi.org/10.1016/j.drugalcdep.2016.11.023 [/mfn] suggests that regular smoking is considered to be a risk factor for the first occurrence of panic attacks and disorders. Nicotine addiction can increase the lifetime risk of panic disorder by three times. Studies [mfn] Lakier J. B. (1992). Smoking and cardiovascular disease. The American journal of medicine, 93(1A), 8S–12S. https://doi.org/10.1016/0002-9343(92)90620-q [/mfn] have found that it is also a contributing factor to increase the risk of cardiovascular disease in panic disorder patients.
Read More About Panic Disorder Here
5. Attention deficit hyperactivity disorder (ADHD)
A 2009 research [mfn] McClernon, F. J., & Kollins, S. H. (2008). ADHD and smoking: from genes to brain to behavior. Annals of the New York Academy of Sciences, 1141, 131–147. https://doi.org/10.1196/annals.1441.016 [/mfn] explains that tobacco consumption in attention deficit hyperactivity disorder patients results from an attempt at self-medication. ADHD patients tend to use nicotine to relieve the symptoms of the disorder. Studies [mfn] Wickström R. (2007). Effects of nicotine during pregnancy: human and experimental evidence. Current neuropharmacology, 5(3), 213–222. https://doi.org/10.2174/157015907781695955 [/mfn] show that women are more likely to get addicted to nicotine early and late in their pregnancy period.
6. Dementia
According to a 2014 study [mfn] Zhou, S., Zhou, R., Zhong, T., Li, R., Tan, J., & Zhou, H. (2014). Association of smoking and alcohol drinking with dementia risk among elderly men in China. Current Alzheimer research, 11(9), 899–907. https://doi.org/10.2174/1567205011666141001123356 [/mfn] , smoking is one of the significant risk factors for dementia. Inhaling the smoke of tobacco is associated with increased oxidative stress [mfn] Kamceva, G., Arsova-Sarafinovska, Z., Ruskovska, T., Zdravkovska, M., Kamceva-Panova, L., & Stikova, E. (2016). Cigarette Smoking and Oxidative Stress in Patients with Coronary Artery Disease. Open access Macedonian journal of medical sciences, 4(4), 636–640. https://doi.org/10.3889/oamjms.2016.117 [/mfn] . Oxidative stress refers to the imbalance between toxic molecules and antioxidants. This imbalance damages the cells in the human body. Research [mfn] Luca, M., Luca, A., & Calandra, C. (2015). The Role of Oxidative Damage in the Pathogenesis and Progression of Alzheimer’s Disease and Vascular Dementia. Oxidative medicine and cellular longevity, 2015, 504678. https://doi.org/10.1155/2015/504678 [/mfn] says that this imbalance is closely related to the onset of dementia. Nicotine inhalation increases the other risk factors of dementia, such as high blood pressure and stroke [mfn] Shah, R. S., & Cole, J. W. (2010). Smoking and stroke: the more you smoke the more you stroke. Expert review of cardiovascular therapy, 8(7), 917–932. https://doi.org/10.1586/erc.10.56 [/mfn] .
Read More About Dementia Here
7. Cognitive decline
People may experience cognitive decline as they get older. A 2012 study [mfn] Sabia, S., Elbaz, A., Dugravot, A., Head, J., Shipley, M., Hagger-Johnson, G., Kivimaki, M., & Singh-Manoux, A. (2012). Impact of smoking on cognitive decline in early old age: the Whitehall II cohort study. Archives of general psychiatry, 69(6), 627–635. https://doi.org/10.1001/archgenpsychiatry.2011.2016 [/mfn] claims that smokers are more likely to experience the symptoms of cognitive decline much earlier than others. Smokers may experience:
- Hallucination [mfn] Quigley, H., & MacCabe, J. H. (2019). The relationship between nicotine and psychosis. Therapeutic advances in psychopharmacology, 9, 2045125319859969. https://doi.org/10.1177/2045125319859969 [/mfn]
- Anxiety and depression [mfn] Leventhal, A. M., & Zvolensky, M. J. (2015). Anxiety, depression, and cigarette smoking: a transdiagnostic vulnerability framework to understanding emotion-smoking comorbidity. Psychological bulletin, 141(1), 176–212. https://doi.org/10.1037/bul0000003 [/mfn]
- Personality changes [mfn] Littlefield, A. K., & Sher, K. J. (2012). Smoking desistance and personality change in emerging and young adulthood. Nicotine & tobacco research : official journal of the Society for Research on Nicotine and Tobacco, 14(3), 338–342. https://doi.org/10.1093/ntr/ntr219 [/mfn]
- Losing motivation [mfn] Blank, M. D., Ferris, K. A., Metzger, A., Gentzler, A., Duncan, C., Jarrett, T., & Dino, G. (2017). Physical Activity and Quit Motivation Moderators of Adolescent Smoking Reduction. American journal of health behavior, 41(4), 419–427. https://doi.org/10.5993/AJHB.41.4.6 [/mfn]
- Confusion regarding visual-spatial tasks [mfn] Fernandes, T., Almeida, N. L., & Santos, N. (2017). Effects of smoking and smoking abstinence on spatial vision in chronic heavy smokers. Scientific reports, 7(1), 1690. https://doi.org/10.1038/s41598-017-01877-z [/mfn]
Read More About Cognitive decline Here
8. Eating disorders
A 2005 study [mfn] Jessen, A., Buemann, B., Toubro, S., Skovgaard, I. M., & Astrup, A. (2005). The appetite-suppressant effect of nicotine is enhanced by caffeine. Diabetes, obesity & metabolism, 7(4), 327–333. https://doi.org/10.1111/j.1463-1326.2004.00389.x [/mfn] says that smoking can decrease appetite and increases satiety. Many people with eating disorders try to suppress their appetite by smoking cigarettes. Research mentions that women with an eating disorder tend to appear to be at increased risk for smoking and higher nicotine dependence, especially those who binge eat and display impulsive behavior.
Read More About Eating disorders Here
Smoking And Personality
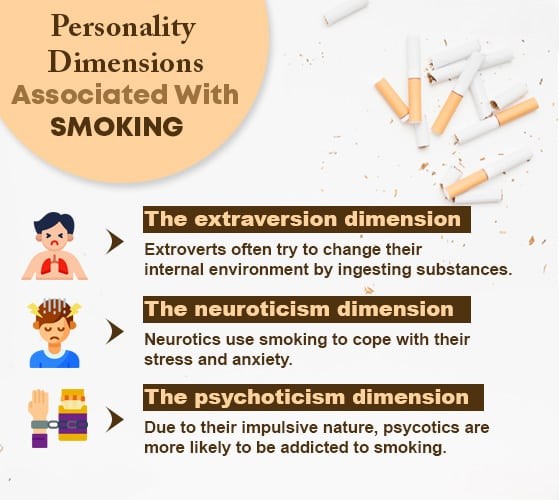
Several significant studies [mfn]Terracciano, A., & Costa, P. T., Jr (2004). Smoking and the Five-Factor Model of personality. Addiction (Abingdon, England), 99(4), 472–481. https://doi.org/10.1111/j.1360-0443.2004.00687.x [/mfn] have examined the connection between smoking and people’s different personality characteristics. These studies have shown the three most common dimensions of characters or personalities that are associated with the psychological aspect of smoking, such as:
1. The extraversion dimension
Certain personality characteristics of extroverts are closely interlinked with nicotine addiction. Extrovert and introvert personalities differ according to the level of necessary stimulation for personal well-being. A recent 2020 study [mfn] Pashapour, H., Musavi, S., Dadashzadeh, H., & Mohammadpoorasl, A. (2020). Relationship between Extraversion and Tobacco Smoking Among High School Students. International journal of preventive medicine, 11, 134. https://doi.org/10.4103/ijpvm.IJPVM_177_19 [/mfn] suggests that extroverts often try to change their external environment by increasing their activity and internal environment by ingesting substances. The extraversion dimension consists of certain factors, such as:
- Positive emotions
- Assertiveness
- Sociability
- Activity level
- Vivacity
2. The neuroticism dimension
A 2002 research [mfn] Goodwin, R., & Hamilton, S. P. (2002). Cigarette smoking and panic: the role of neuroticism. The American journal of psychiatry, 159(7), 1208–1213. https://doi.org/10.1176/appi.ajp.159.7.1208 [/mfn] says that certain personality traits of neuroticism make an individual sensitive to nicotine properties. Such people often use smoke to cope with their stress and anxiety. Research [mfn] Lahey B. B. (2009). Public health significance of neuroticism. The American psychologist, 64(4), 241–256. https://doi.org/10.1037/a0015309 [/mfn] shows that the neuroticism dimension is associated with some psychological disorders, including depression and anxiety. These personalities portray high frequency and intensity of negative affect. This dimension contains some significant factors, including:
- Anxiety
- Psychological vulnerability
- Depression
- Anger
- Hostility
- Negative thoughts
- Jealousy
3. The psychoticism dimension
According to a 1984 research paper [mfn] Parkes K. R. (1984). Smoking and the Eysenck personality dimensions: an interactive model. Psychological medicine, 14(4), 825–834. https://doi.org/10.1017/s0033291700019796 [/mfn] , the association between psychoticism and tobacco intake is the most consistent dimension. The psychoticism dimension of personalities includes the following factors:
- Cynicism
- Impulsivity
- Antisocial actions and behaviors
- Reduced conformity
- Coldness
- Reduced inhibition
- Attraction toward exciting sensations
- Low conscientiousness
Initiating Factors Of Smoking
The factors that trigger the habit of smoking among regular and adult smokers are quite different from those factors that are associated with smoking initiation. A 2011 study [mfn] Peltzer K. (2011). Early smoking initiation and associated factors among in-school male and female adolescents in seven African countries. African health sciences, 11(3), 320–328. [/mfn] mentions that higher nicotine addiction among various population ranges is triggered or influenced by different psychological, social, economic, and cultural factors, including:
- Peer influence (which is the most common predictor)
- Parental or sibling smoking
- Low socioeconomic status
- Poor housing and permanent unemployment
- Substance exposure during childhood
- Access to tobacco products
- Certain beliefs about nicotine’s advantages
- Financial pressure and stress
- Prior history of anxiety and depression
- Influenced by intensive marketing of tobacco products
- Prior experiments with tobacco products
- Lower likelihood of working indoors
- Lack of parental involvement
- Low academic achievement
- lack of cigarette refusal skills
- Low self-esteem
- No knowledge of the harmful effects of tobacco
Smoking Withdrawal
When people suddenly stop smoking and no tobacco is entering their body, they experience certain mild to severe unpleasant physical and psychological symptoms. These symptoms are called nicotine withdrawal symptoms [mfn] Benowitz N. L. (2010). Nicotine addiction. The New England journal of medicine, 362(24), 2295–2303. https://doi.org/10.1056/NEJMra0809890 [/mfn] . The severity of the symptoms largely depends on how much and how long the person has smoked.
Research [mfn] Institute of Medicine (US) Committee on Preventing Nicotine Addiction in Children and Youths; Lynch BS, Bonnie RJ, editors. Growing up Tobacco Free: Preventing Nicotine Addiction in Children and Youths. Washington (DC): National Academies Press (US); 1994. 2, THE NATURE OF NICOTINE ADDICTION. Available from: https://www.ncbi.nlm.nih.gov/books/NBK236759/ [/mfn] says that these withdrawal symptoms can be observed in a person within 24-48 hours after he/she last smoked. The symptoms are considered a sign of psychological and physical dependence on nicotine. A 2015 research [mfn] McLaughlin, I., Dani, J. A., & De Biasi, M. (2015). Nicotine withdrawal. Current topics in behavioral neurosciences, 24, 99–123. https://doi.org/10.1007/978-3-319-13482-6_4 [/mfn] has mentioned some of the most common physical and psychological withdrawal symptoms of nicotine, such as:

- Intense craving for nicotine
- Weight gain
- Anxiety and depression
- Changes in appetite
- Headaches and dizziness
- Problems in concentrating
- Sleeping disorders
- Stress and restlessness
- Fatigue
- Constipation
- Mental fog
- Irritability
- Sweating
- Sore throat and coughing
- Abdominal cramping
- nausea and vomiting
- Tingling in the hands and feet
How To Quit Smoking

Despite knowing about all the health risks of nicotine, people start smoking and eventually get addicted to it. It is considered to be a psychological habit and physical addiction. Smoking might offer temporary pleasure and satisfaction, but it has numerous harmful effects on people’s physical and mental well-being. Though quitting smoking can have certain mild as well as severe side effects, a person needs to stop consuming nicotine as it can be life-threatening. Here are some of the effective ways by which one can quit smoking:
- One needs to find and understand their personal reason to stop consuming nicotine. Choosing a reason that is strong enough often helps one to reduce the urge.
- Identify the trigger situations and try to avoid them completely.
- Understand that the withdrawal will not happen overnight. Your body will need enough time to deal with the withdrawal.
- Consult with a health care professional and consider nicotine replacement therapy [mfn] Wadgave, U., & Nagesh, L. (2016). Nicotine Replacement Therapy: An Overview. International journal of health sciences, 10(3), 425–435. [/mfn] . This therapy will help you in coping with withdrawal symptoms.
- Whenever feeling a craving, give yourself at least 10 minutes first and try to distract yourself for that period of time.
- Inform your loved ones that you are planning to quit smoking. Your family and friends can make the withdrawal easy for you by providing care and support.
- Give yourself a break. Spend time with your loved ones. Do something that makes you happy. Listen to some music or cook your favorite food.
- If you feel a craving for nicotine, chew sugarless gum or munch carrots or nuts to satisfy your craving.
- Get yourself habituated with regular physical activity. You can also try yoga or meditation [mfn] Khanna, S., & Greeson, J. M. (2013). A narrative review of yoga and mindfulness as complementary therapies for addiction. Complementary therapies in medicine, 21(3), 244–252. https://doi.org/10.1016/j.ctim.2013.01.008 [/mfn] or any kind of mindfulness practice.
- Eat healthy food and drink plenty of water. Add some fresh vegetables and fruits to your daily diet.
- Don’t be disappointed and try until you succeed in overcoming your cravings.
- If you find it extremely difficult to quit smoking, consider seeking medical help and treatment.
Takeaway
Smoking is the harmful practice of inhaling the smoke of burning tobacco. It might offer a sense of relaxation and pleasure to the body at first but gradually prevents an individual from feeling the same level of pleasure. This condition leads to the person craving more nicotine. Nicotine addiction can have extreme effects on an individual’s physical and psychological health.
Regular nicotine inhalation causes several significant psychotic disorders. People often start smoking due to various reasons, such as peer pressure, tobacco marketing influence, parental or sibling smoking, childhood exposure, and many more. Smoking can cause life-threatening diseases, people should stop nicotine consumption and seek medical help if needed.
Smoking At A Glance
- Smoking is a harmful act where people burn various plant materials and inhale the smoke that reaches the brain within 10-20 seconds.
- Dried tobacco leaves are mostly used for smoking and nicotine is the most harmful substance in tobacco that causes addiction.
- Studies revealed that around 1 billion people regularly consume tobacco and it kills almost 1 million people every year worldwide.
- Nicotine addiction is associated with several life-threatening physical and physiological disorders, such as cancer, heart attack, respiratory diseases, depression, obsessive-compulsive disorder, panic attacks, schizophrenia, dementia, and many more.
- Smoking is also closely interconnected with three personality dimensions that include extraversion, neuroticism, and psychoticism.
- People may experience several mild to severe physical and psychological symptoms after they quit smoking.







Leave a Reply