Alzheimer’s disease (AD) is a progressive type of dementia which leads to a decline in thinking, memory, behavior and daily social & occupational functioning. It mostly affects people over the age of 65.
What Is Alzheimer’s Disease (AD)?
Also known simply as Alzheimer’s, it is a neurodegenerative condition that causes cognitive decline, and loss of memory due to atrophy or shrinkage of the brain and dying brain cells. It is an irreparable condition that progressively becomes worse and affects the sufferer’s ability to conduct simple daily activities. According to the World Health Organization, about 50 million people suffer from this condition globally with 10 million new patients each year.
Moreover, it also causes around 70% of dementia cases. Dementia is a syndrome that causes cognitive deterioration that affects thinking and daily functioning. According to recent research 1 Kumar A, Sidhu J, Goyal A, et al. Alzheimer Disease. [Updated 2020 Nov 18]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK499922/ , it is “a neurodegenerative disease with insidious onset and progressive impairment of behavioral and cognitive functions including memory, comprehension, language, attention, reasoning, and judgment.” The researchers found that early onset before the age of 65 is rare and is observed only in 10% of cases. “ It is the sixth leading cause of death in the United States,” states the research paper.
AD may cause severe cognitive & behavioral impairment, language difficulties and abnormal or impulsive behavior. As it becomes progressively worse, a person may be unable to recall recent experiences and fail to identify loved ones & family members. In severe cases, the sufferer may require full-time assistance. Although treatment may help, as of now there is no specific cure for this neurological condition. It should be noted that Alzheimer’s and dementia are not the same conditions, even though they are often mistakenly used interchangeably. AD is a form of dementia.
Understanding Alzheimer’s
Alzheimer’s disease is primarily marked by the existence of plaques & tangles 2 Perl D. P. (2010). Neuropathology of Alzheimer’s disease. The Mount Sinai journal of medicine, New York, 77(1), 32–42. https://doi.org/10.1002/msj.20157 in the hippocampus deep within the brain. According to a 2011 study 3 Serrano-Pozo, A., Frosch, M. P., Masliah, E., & Hyman, B. T. (2011). Neuropathological alterations in Alzheimer disease. Cold Spring Harbor perspectives in medicine, 1(1), a006189. https://doi.org/10.1101/cshperspect.a006189 , the neuropathological traits of AD involve “positive lesions such as amyloid plaques and cerebral amyloid angiopathy, neurofibrillary tangles, and glial responses, and negative lesions such as neuronal and synaptic loss.”
It may also result in a loss of connection between the brain and neurons. One 2017 study 4 Kocahan, S., & Doğan, Z. (2017). Mechanisms of Alzheimer’s Disease Pathogenesis and Prevention: The Brain, Neural Pathology, N-methyl-D-aspartate Receptors, Tau Protein and Other Risk Factors. Clinical psychopharmacology and neuroscience : the official scientific journal of the Korean College of Neuropsychopharmacology, 15(1), 1–8. https://doi.org/10.9758/cpn.2017.15.1.1 found that almost 80% of the neurons present in the hippocampus can die due to AD which causes cognitive alterations. This means information is not transmitted properly between various brain regions and from the brain to the organs & muscles.
The syndrome was originally described 5 Schachter, A. S., & Davis, K. L. (2000). Alzheimer’s disease. Dialogues in clinical neuroscience, 2(2), 91–100. https://doi.org/10.31887/DCNS.2000.2.2/asschachter by Dr. Alois Alzheimer in 1906 based on the criteria of senile plaques & neurofibrillary tangles, disorientation, progressive loss of memory and pathological markers. Although believed to be a rare disorder initially, it was eventually found to be an unavoidable outcome of aging. But it is not a normal element of aging. During his initial analysis, Dr. Alzheimer observed certain abnormalities in the brain tissue of a female patient 6 What is Alzheimer’s disease? (2017). National Institute on Aging. https://www.nia.nih.gov/health/what-alzheimers-disease who died from an unrecognizable psychiatric condition.
The patient experienced symptoms like abnormal behavior, language problems and memory loss. However, upon examination of the deceased patient, he found several unusual clumps (amyloid plaques) along with tangled fiber bundles (neurofibrillary tangles) in her brain. As a result of his observation, the condition was named after Dr. Alois Alzheimer and plaques and tangles in the brain became the primary features of the condition. However, it is believed that several other changes in the brain may be associated with AD.
The abnormalities first appear in the hippocampus which play a vital part in developing memories. Other areas of the brain also become affected when neurons or nerve cells start dying. As AD becomes progressively worse, the damage spreads to different areas causing significant atrophy 7 Marino, S., Bonanno, L., Lo Buono, V., Ciurleo, R., Corallo, F., Morabito, R., Chirico, G., Marra, A., & Bramanti, P. (2019). Longitudinal analysis of brain atrophy in Alzheimer’s disease and frontotemporal dementia. The Journal of international medical research, 47(10), 5019–5027. https://doi.org/10.1177/0300060519830830 or shrinking of the brain tissue. According to a 2019 study 8 Coupé, P., Manjón, J. V., Lanuza, E., & Catheline, G. (2019). Lifespan Changes of the Human Brain In Alzheimer’s Disease. Scientific reports, 9(1), 3998. https://doi.org/10.1038/s41598-019-39809-8 , “Brain imaging studies have shown that slow and progressive cerebral atrophy characterized the development of Alzheimer’s Disease.” It adds that neurodegeneration, measured by the degree of cerebral atrophy, “is one of these biomarkers” of AD.
Symptoms Of Alzheimer’s Disease
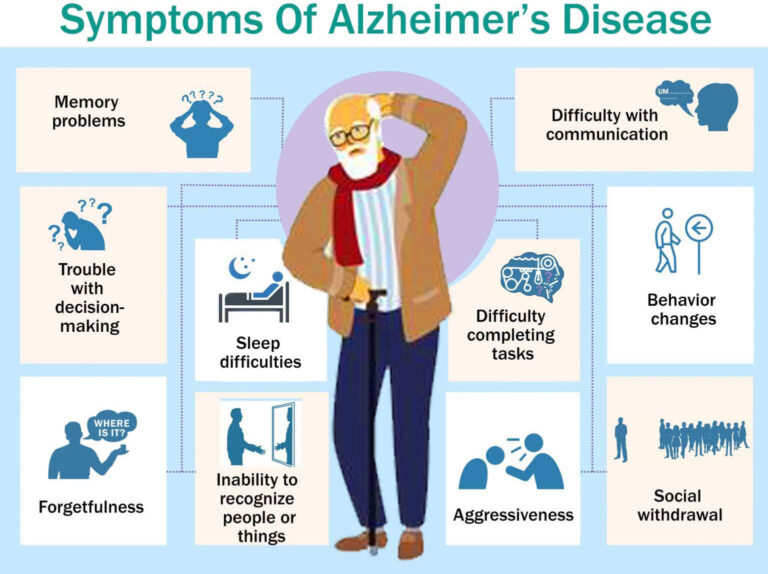
One of the most common signs of AD is loss of memory. Although the symptoms tend to vary for each patient, cognitive decline and problems with thinking & language are observed in most patients during the initial stages. Some sufferers may also experience mild cognitive impairment (MCI 9 Lopez O. L. (2013). Mild cognitive impairment. Continuum (Minneapolis, Minn.), 19(2 Dementia), 411–424. https://doi.org/10.1212/01.CON.0000429175.29601.97 ). Patients also tend to have difficulty completing normal daily tasks and may become unable to care for themselves in severe cases. They may fail to recognize family members, ask questions repeatedly, put things in uncommon places and fail to find them and may even wander away or get physically lost. Here are some other common signs and symptoms of Alzheimer’s disease:
- Memory problems
- Cognitive deficits
- Forgetfulness
- Inability to recognize people or things
- Behavior changes and obsessive compulsive behavior
- Trouble with judgment or reasoning
- Isolation and social withdrawal
- Disorientation about time and/or place
- Trouble with decision-making and problem-solving
- Reduced personal hygiene or need for assisted personal care
- Spatial awareness issues and loss of balance
- Mood swings, confusion and delusions
- Difficulty with communication, speech or writing
- Lack of empathy or apathy
- Loss of motivation or interest
- Irritability, anger or aggressiveness
- Difficulty completing tasks
- Sleep difficulties
- Depression
Read More About Depression Here
Studies 10 Clark, C. N., Nicholas, J. M., Gordon, E., Golden, H. L., Cohen, M. H., Woodward, F. J., Macpherson, K., Slattery, C. F., Mummery, C. J., Schott, J. M., Rohrer, J. D., & Warren, J. D. (2016). Altered sense of humor in dementia. Journal of Alzheimer’s disease : JAD, 49(1), 111–119. https://doi.org/10.3233/JAD-150413 also show that changes in an individual’s sense of humor may also be an early warning sign of AD. As it is a progressive neurodegenerative disorder, the symptoms tend to get more severe over time, when left untreated. Typically, the symptoms tend to develop over months or even years. However, in case these symptoms start manifesting in days or hours, then immediate medical attention may be necessary.
Stages Of Alzheimer’s Disease
AD can appear differently for different individuals . However, everyone tends to experience the same course that progressively worsens from the beginning to the end of the illness. Although there are different models covering the stages of AD, the most popular and common model is the seven stages of Alzheimer’s developed by Barry Reisberg, M.D. 11 Reisberg, B., Ferris, S. H., de Leon, M. J., & Crook, T. (1982). The Global Deterioration Scale for assessment of primary degenerative dementia. The American journal of psychiatry, 139(9), 1136–1139. https://doi.org/10.1176/ajp.139.9.1136 , Professor of Psychiatry at New York University Langone Health. Also known as the Global Deterioration Scale (GDS 12 Krzymińska, E., Rossa, G., & Krzymiński, S. (1993). Skale GDS i FAST w rozpoznawaniu otepienia type Alzheimera [The Global Deterioration Scale (GDS) and Functional Assessment Staging (FAST) in the diagnosis of Alzheimer type dementia]. Psychiatria polska, 27(2), 129–138. ), this model includes the following stages of Alzheimer’s:
Stage 1: Normal behavior with no impairment
There are no noticeable symptoms or problems during this early stage. But an early diagnosis with a positron emission tomography (PET) scan may reveal the brain’s functioning.
Stage 2: Very mild decline or changes
At this stage, minor memory problems may appear, like forgetfulness, which may also be due to the normal aging process. There may also be negligible changes in behavior. However, these subtle signs typically do not affect their normal functioning. It may be too early for doctor’s or loved ones to identify AD.
Stage 3: Mild Decline
Here, mild cognitive 13 Grundman, M. (2004). Mild cognitive impairment can be distinguished from Alzheimer disease and normal aging for clinical trials. Archives of Neurology, 61(1), 59. https://doi.org/10.1001/archneur.61.1.59 and physical impairments may become noticeable, like cognitive problems, decreased attention & memory, difficulty making decisions etc. Symptoms may be noticeable to close loved ones and memory tests can reveal impaired cognition.
Stage 4: Moderate decline
In the fourth stage of Alzheimer’s, the common symptoms of the disorder start to manifest more clearly than the previous stage. Although the symptoms are still mild, the person may experience impairment in the ability to perform daily tasks.
Stage 5: Moderately severe decline
As the symptoms become moderate to severe, the patient may require help and support from caregivers or loved ones in daily activities. They may become confused and have memory problems.
Stage 6: Severe decline
In the sixth stage of Reisberg’s model, an individual suffering from Alzheimer’s may need continuous supervision with basic tasks, like wearing clothes or eating. They may not recognize family members and become confused & delusional.
Stages 7: Very severe decline
In the final stage, patients typically face difficulties in eating and walking. They may lose their ability to communicate and may need constant assistance. People in this stage may be nearing death as it’s a terminal disease.
Causes Of Alzheimer’s Disease
The exact causes of this disorder are not yet known. However, it is believed that a combination of different factors such as genetic, environmental & lifestyle factors may play a contributing role. It believed that late onset is associated with changes in the brain while early onset may be related to genetic mutation. Here are some of the common risk factors that may influence the development of Alzheimer’s –
1. Brain structure and protein
The condition may be caused by an abnormal growth and spread of amyloid protein 14 de Paula, V., Guimarães, F. M., Diniz, B. S., & Forlenza, O. V. (2009). Neurobiological pathways to Alzheimer’s disease: Amyloid-beta, TAU protein or both?. Dementia & neuropsychologia, 3(3), 188–194. https://doi.org/10.1590/S1980-57642009DN30300003 and tau protein 15 Medeiros, R., Baglietto-Vargas, D., & LaFerla, F. M. (2010). The role of tau in Alzheimer’s disease and related disorders. CNS Neuroscience & Therapeutics, 17(5), 514-524. https://doi.org/10.1111/j.1755-5949.2010.00177.x in the brain that results in the death of brain cells. According to a 2019 study 16 Tiwari, S., Atluri, V., Kaushik, A., Yndart, A., & Nair, M. (2019). Alzheimer’s disease: pathogenesis, diagnostics, and therapeutics. International journal of nanomedicine, 14, 5541–5554. https://doi.org/10.2147/IJN.S200490 , AD is a “prominent protein-conformational disease (PCD) primarily caused by the aberrant processing and polymerization of normally soluble proteins 17 Tran, L., & Ha-Duong, T. (2015). Exploring the Alzheimer amyloid-β peptide conformational ensemble: A review of molecular dynamics approaches. Peptides, 69, 86–91. https://doi.org/10.1016/j.peptides.2015.04.009 .” It is believed that the build up of amyloid protein leads to the formation of plaques while fibers of tau protein create tangles. These plaques and tangles hinder communication among neurons and prevent them from functioning normally. The death of the nerve cells gradually progresses and spreads to other areas leading to the symptoms of AD.
2. Genetics
Genes 18 Bekris, L. M., Yu, C. E., Bird, T. D., & Tsuang, D. W. (2010). Genetics of Alzheimer disease. Journal of geriatric psychiatry and neurology, 23(4), 213–227. https://doi.org/10.1177/0891988710383571 may also play a crucial role in the development of Alzheimer’s disease. According to a 2019 study 19 Silva, M., Loures, C., Alves, L., de Souza, L. C., Borges, K., & Carvalho, M. (2019). Alzheimer’s disease: risk factors and potentially protective measures. Journal of biomedical science, 26(1), 33. https://doi.org/10.1186/s12929-019-0524-y , “Approximately 70% of the risk of developing AD can be attributed to genetics.” Early-onset AD, which occurs before the age of 60 to 65 years, may be a result of gene mutations or permanent changes in specific genes that can be passed to children from their parents. This is identified as early-onset familial Alzheimer disease (FAD).
“Familial AD (FAD) characterizes families that have more than one member with AD and usually implies multiple affected persons in more than one generation,” explains a recent study 20 Bird, T. D. (1999). Early-Onset Familial Alzheimer Disease – RETIRED CHAPTER, FOR HISTORICAL REFERENCE ONLY. In M. P. Adam (Eds.) et. al., GeneReviews®. University of Washington, Seattle. . So if you have a first-degree relative suffering from the disorder, then it is highly likely you may develop it too. However, it should be noted that although genetics may increase the risk of developing the disease, it does not necessarily cause AD.
3. Age
As the condition typically develops after 65 years of age, aging is believed to be perhaps the most significant risk factor for AD. Although not a normal aspect of aging, growing older does increase the risk. “Advanced age, however, remains the major established risk factor for AD, although environmental variables may also have some role in disease expression,” states a 2000 study 21 Munoz, D. G., & Feldman, H. (2000). Causes of Alzheimer’s disease. CMAJ : Canadian Medical Association journal = journal de l’Association medicale canadienne, 162(1), 65–72. . Research 22 Reitz, C., & Mayeux, R. (2014). Alzheimer disease: epidemiology, diagnostic criteria, risk factors and biomarkers. Biochemical pharmacology, 88(4), 640–651. https://doi.org/10.1016/j.bcp.2013.12.024 also found that the incidence rate for AD tends to greatly increase with age with the highest observable increased risk during “the 7th and 8th decades of life.”
Read More About Aging And Mental Health Here
4. Environmental factors
Various environmental factors 23 Wainaina, M. N., Chen, Z., & Zhong, C. (2014). Environmental factors in the development and progression of late-onset Alzheimer’s disease. Neuroscience bulletin, 30(2), 253–270. https://doi.org/10.1007/s12264-013-1425-9 like brain injury, childhood experiences, lifestyle, social engagement, malnutrition or exposure to toxic chemicals & infectious agents 24 Armstrong R. A. (2013). What causes alzheimer’s disease?. Folia neuropathologica, 51(3), 169–188. https://doi.org/10.5114/fn.2013.37702 , can also influence onset of Alzheimer’s. The condition may also be associated with other disorders such as obesity, diabetes, high blood pressure, immune system dysfunction, stroke and heart disease. One 2016 study 25 Killin, L. O., Starr, J. M., Shiue, I. J., & Russ, T. C. (2016). Environmental risk factors for dementia: a systematic review. BMC geriatrics, 16(1), 175. https://doi.org/10.1186/s12877-016-0342-y found “moderate evidence for air pollution exposures being related to dementia risk, particularly nitrogen oxides, particulate matter, and ozone.”
Apart from these, other risk factors for AD may include:
- Mild cognitive impairment
- Head trauma
- Gender
- Down syndrome
- Sedentary lifestyle
- Cardiovascular disease
- Unhealthy sleep patterns
- Excessive alcohol use
- Untreated or chronic depression
- Education
- Poor diet
- Hearing loss
- Social isolation or loneliness
Diagnosis Of Alzheimer’s Disease
To be diagnosed with Alzheimer’s, the patient must experience behavioral changes, cognitive decline and memory loss. As there are no specific tests for the condition, a doctor may inquire about the patient’s symptoms, medical history, family history, medications, lifestyle and use of alcohol or substances to rule out other underlying medical conditions. The doctor can also conduct certain physical and lab tests such as blood pressure, heart rate and blood or urine tests.
Moreover, the following mental, neurological, physical & imaging tests may also be required to be conducted for a proper diagnosis:
- Neurological function and neuropsychological tests
- Mental status testing, such as memory and cognitive tests
- Genetic testing
- Positron emission tomography (PET) scan
- Magnetic resonance imaging (MRI)
- Computed tomography (CT) scan
- Assessment tools to evaluate cognitive function
- Tests to determine emotional stability, personality and behavior changes
Once someone has been clinically diagnosed with Alzheimer’s disease, it is important that they seek medical attention. Early diagnosis and treatment can help to manage and alleviate the symptoms.
Treatment Of Alzheimer’s Disease
Currently there is no specific cure for Alzheimer’s disease as the death of brain cells is irreversible. However, certain treatment approaches can help to alleviate the symptoms and help to improve the patient’s quality of life. Moreover, treatment can also help to maintain cognitive function and better manage issues like memory loss. Typically treatment addresses the following aspects:
- Enabling the patient to maintain brain and cognitive health
- Delaying or relieving common symptoms
- Regulating behavioral symptoms
Here are some of the most recommended treatment approaches for AD:
1. Medications
Although there are no specific medications for AD, certain medications may be prescribed by a doctor for the short-term relief of specific symptoms. Some of the medicines may include:
A. Acetylcholinesterase (AChE) inhibitors
Also known as cholinesterase inhibitors 26 McGleenon, B. M., Dynan, K. B., & Passmore, A. P. (1999). Acetylcholinesterase inhibitors in Alzheimer’s disease. British journal of clinical pharmacology, 48(4), 471–480. https://doi.org/10.1046/j.1365-2125.1999.00026.x , these medications help to boost acetylcholine levels which facilitates the communication between nerve cells. These can help to improve cognitive symptoms like confusion and memory loss. According to a 2011 study 27 Mehta, M., Adem, A., & Sabbagh, M. (2012). New acetylcholinesterase inhibitors for Alzheimer’s disease. International journal of Alzheimer’s disease, 2012, 728983. https://doi.org/10.1155/2012/728983 , “Acetylcholinesterase (AChE) has proven to be the most viable therapeutic target for symptomatic improvement in Alzheimer’s disease (AD).” Three cholinesterase inhibitors, namely donepezil 28 Howard, R., McShane, R., Lindesay, J., Ritchie, C., Baldwin, A., Barber, R., Burns, A., Dening, T., Findlay, D., Holmes, C., Hughes, A., Jacoby, R., Jones, R., Jones, R., McKeith, I., Macharouthu, A., O’Brien, J., Passmore, P., Sheehan, B., Juszczak, E., … Phillips, P. (2012). Donepezil and memantine for moderate-to-severe Alzheimer’s disease. The New England journal of medicine, 366(10), 893–903. https://doi.org/10.1056/NEJMoa1106668 , rivastigmine, and galantamine have been approved 29 Matsunaga, S., Kishi, T., Nomura, I., Sakuma, K., Okuya, M., Ikuta, T., & Iwata, N. (2018). The efficacy and safety of memantine for the treatment of Alzheimer’s disease. Expert opinion on drug safety, 17(10), 1053–1061. https://doi.org/10.1080/14740338.2018.1524870 by the U.S. Food and Drug Administration (FDA) for AD treatment.
B. Memantine
These are used mostly by patients who cannot tolerate cholinesterase inhibitors. Memantine 30 Folch, J., Busquets, O., Ettcheto, M., Sánchez-López, E., Castro-Torres, R. D., Verdaguer, E., Garcia, M. L., Olloquequi, J., Casadesús, G., Beas-Zarate, C., Pelegri, C., Vilaplana, J., Auladell, C., & Camins, A. (2018). Memantine for the Treatment of Dementia: A Review on its Current and Future Applications. Journal of Alzheimer’s disease : JAD, 62(3), 1223–1240. https://doi.org/10.3233/JAD-170672 helps to block and manage glutamate levels, a chemical compound in the brain.
One 2006 study 31 Robinson, D. M., & Keating, G. M. (2006). Memantine: a review of its use in Alzheimer’s disease. Drugs, 66(11), 1515–1534. https://doi.org/10.2165/00003495-200666110-00015 found that this medicine is “an effective pharmacotherapeutic agent, and currently the only approved option, for the treatment of moderate to severe Alzheimer’s disease.”
C. Huperzine A (HupA)
According to a 2018 study 32 Weller, J., & Budson, A. (2018). Current understanding of Alzheimer’s disease diagnosis and treatment. F1000Research, 7, F1000 Faculty Rev-1161. https://doi.org/10.12688/f1000research.14506.1 , the nutraceutical huperzine A is considered as an effective disease-modifying alternative drug for Alzheimer’s. “For patients who choose alternative therapy, the nutraceutical huperzine A 33 Xing, S. H., Zhu, C. X., Zhang, R., & An, L. (2014). Huperzine a in the treatment of Alzheimer’s disease and vascular dementia: a meta-analysis. Evidence-based complementary and alternative medicine : eCAM, 2014, 363985. https://doi.org/10.1155/2014/363985 has shown benefit in both memory function and activities of daily living,” adds the study. However, it is not approved by the FDA in the U.S. but government-approved in some other countries. Research 34 Qian, Z. M., & Ke, Y. (2014). Huperzine A: Is it an Effective Disease-Modifying Drug for Alzheimer’s Disease?. Frontiers in aging neuroscience, 6, 216. https://doi.org/10.3389/fnagi.2014.00216 shows that HupA is a highly effective medication and can be regarded as a “disease-modifying drug for AD.”
Apart from the above mentioned medications, a doctor may also prescribe other drugs like antidepressants, antipsychotics or anti-anxiety medications to reduce specific symptoms, such as depression, aggression, hallucinations etc.
2. Therapy
Some forms of therapy and activities may also be helpful for people suffering from Alzheimer’s disease. Here are some of the most recommended therapy approaches for this disorder:
A. Cognitive stimulation therapy (CST)
CST 35 Kim, K., Han, J. W., So, Y., Seo, J., Kim, Y. J., Park, J. H., Lee, S. B., Lee, J. J., Jeong, H. G., Kim, T. H., & Kim, K. W. (2017). Cognitive Stimulation as a Therapeutic Modality for Dementia: A Meta-Analysis. Psychiatry investigation, 14(5), 626–639. https://doi.org/10.4306/pi.2017.14.5.626 can help people with dementia with themed activities that are conducted in groups throughout a number of weeks under the supervision of a trained healthcare professional like a therapist or a nurse. The sessions focus on various topics that help to improve the memories and cognitive functioning of the patients. One 2019 study 36 Chen, J., Duan, Y., Li, H., Lu, L., Liu, J., & Tang, C. (2019). Different durations of cognitive stimulation therapy for Alzheimer’s disease: a systematic review and meta-analysis. Clinical interventions in aging, 14, 1243–1254. https://doi.org/10.2147/CIA.S210062 found that “the combination of CST and drug treatment for AD is effective in AD, regardless of whether short-term CST, maintenance CST, or long-term CST is used.” However, the study observed that “long-term CST appears to be more effective.”
B. Cognitive rehabilitation therapy
This involves a number of evidence-based interventions that aim to improve the cognitive abilities and functioning of individuals who are cognitively impaired or have experienced brain injuries. Cognitive rehabilitation 37 Choi, J., & Twamley, E. W. (2013). Cognitive rehabilitation therapies for Alzheimer’s disease: a review of methods to improve treatment engagement and self-efficacy. Neuropsychology review, 23(1), 48–62. https://doi.org/10.1007/s11065-013-9227-4 can help to balance cognitive deficits and facilitate normal functioning. This form of therapy involves coordinating with trained therapists and caregivers to reach personal goals. It focuses on using brain regions that are still functional to improve areas that are not functioning. One 2017 study 38 Brueggen, K., Kasper, E., Ochmann, S., Pfaff, H., Webel, S., Schneider, W., & Teipel, S. (2017). Cognitive Rehabilitation in Alzheimer’s Disease: A Controlled Intervention Trial. Journal of Alzheimer’s disease : JAD, 57(4), 1315–1324. https://doi.org/10.3233/JAD-160771 found that this therapy can help to improve “communication skills and coping mechanisms” in patients. Another 2015 study 39 Hwang, J. H., Cha, H. G., & Cho, H. S. (2015). The effects of cognitive rehabilitation on Alzheimer’s dementia patients’ cognitive assessment reference diagnosis system performance based on level of cognitive functioning. Journal of physical therapy science, 27(9), 2875–2877. https://doi.org/10.1589/jpts.27.2875 revealed that cognitive rehabilitation can lead to “significantly greater memory improvements.”
Moreover, reminiscing about events from the past, such as looking at old photos, can also be helpful.
Prevention
Along with medications and therapy, certain coping strategies can also help a person deal with Alzheimer’s symptoms. Here are some preventive measures to protect someone from cognitive decline:
- Socialize and talk to your friends and family frequently
- Stay physically active
- Avoid substances, alcohol and smoking
- Have a nutritious plant-based diet and consume adequate antioxidants
- Practice cognitive training exercises
Changing your lifestyle can help significantly in preventing this condition.
Tips For Caregivers
If you care for a loved one with Alzheimer’s disease, then it can certainly be a challenging yet rewarding job. As being a caregiver requires that you have a lot of patience and pay your full attention to your loved one, one of the most important tips for you is to practice self-care. With increased stress and responsibilities, caregivers often tend to ignore their own needs. However, only by caring for yourself, you can care better for your loved one with AD. Here are some other helpful tips:
- Focus on physical and mental comfort of the patient
- Avoid arguing or being confrontational with the patient
- Acknowledge their requests and respond positively
- Build a warm and peaceful environment at home
- Understand that there is a specific reason behind each behavior
- Offer a security object
- Redirect their attention
- Encourage them to rest between energizing and stimulating experiences
- Look for various options, solutions and opportunities to help them
- Never take things personally
Focus On Improving Quality Of Life
As Alzheimer’s is an irreversible and complex neurodegenerative disease, there is no specific cure. However, with effective treatment, coping techniques and prevention, you can enable the patient to enjoy a better quality of life. If you or a loved is suffering from AD, make sure to consult a doctor immediately as early diagnosis and treatment can help greatly.
Alzheimer’s Disease At A Glance
- Alzheimer’s disease is a neurodegenerative condition that causes cognitive decline, and loss of memory due to atrophy or shrinkage of the brain and dying brain cells.
- One of the most common signs of Alzheimer’s disease is loss of memory.
- It is believed that a combination of different factors such as genetic, environmental & lifestyle factors may play a contributing role.
- To be diagnosed with Alzheimer’s, the patient must experience behavioral changes, cognitive decline and memory loss
- There are certain treatment approaches that can help to alleviate the symptoms and help to improve the patient’s quality of life.