Table of Contents
Disruptive mood dysregulation disorder (DMDD) is a mental disorder observed in children and adolescents. With adequate help and resources, parents may be able to manage and treat it effectively.
What Is Disruptive Mood Dysregulation Disorder?
Disruptive mood dysregulation disorder (DMDD) is a mood disorder that occurs in children. It is characterized by intense irritability, persistent anger, and frequent, extreme temper outbursts.
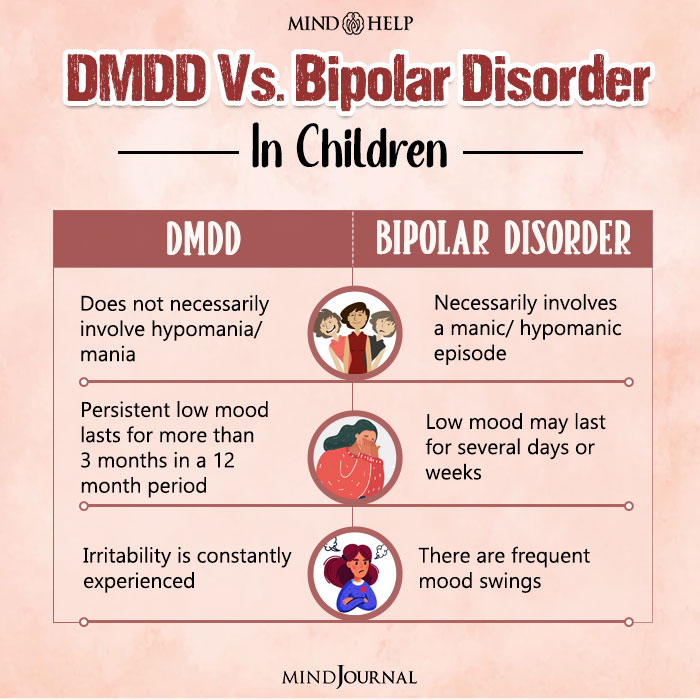
A relatively new diagnosis, DMDD was added to the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) in 2013. According to the DSM-5 1 American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). https://dsm.psychiatryonline.org/doi/book/10.1176/appi.books.9780890425787 , DMDD is a type of depressive disorder that makes it difficult for children to regulate and manage their emotions in an appropriate way.
Most children exhibit temper tantrums from time to time. However, the severe reactions in disruptive mood dysregulation disorder are more than just temper tantrums and are usually age-inappropriate and disproportionate to the current situation.
Children and adolescents suffering from this condition experience extreme impairment which may necessitate medical attention. In fact, these children have significant problems adjusting at home, school, and with peers. They also have high rates of hospitalization, doctor visits, and school suspensions 2 Disruptive Mood Dysregulation Disorder: The Basics. (n.d.). Www.nimh.nih.gov. https://www.nimh.nih.gov/health/publications/disruptive-mood-dysregulation-disorder .
- Read More About ADHD Here
- Read More About Bipolar Disorder Here
How Common Is DMDD?
Research shows that disruptive mood dysregulation disorder affects 2-5% 3 The newest “rage”: disruptive mood dysregulation disorder. (n.d.). Www.mdedge.com. Available from: https://www.mdedge.com/pediatrics/article/106070/mental-health/newest-rage-disruptive-mood-dysregulation-disorder of children with most of them being boys. A 2013 study 4 Copeland, W. E., Angold, A., Costello, E. J., & Egger, H. (2013). Prevalence, comorbidity, and correlates of DSM-5 proposed disruptive mood dysregulation disorder. The American journal of psychiatry, 170(2), 173–179. https://doi.org/10.1176/appi.ajp.2012.12010132 has found that among 3,200 children of 2-17 years of age, about 0.8-3.3% of the children met the DMDD criteria. However, the condition is less prevalent in teenagers. Disruptive mood dysregulation disorder occurs with another disorder about 62-92% of the time.
Case Example
A few weeks after shifting to a new school, 12-year-old Rohit started throwing tantrums at home. He frequently refused to eat what was served to him and would scream at his mother whenever she asked him to do his homework. Assuming that he might be having trouble adjusting to a new environment, his parents hoped he would calm down with time.
However, months passed and there was no change in Rohit’s behavior. His father repeatedly got complaints from his school that he was getting into frequent fights with his classmates, and was mostly rude and moody in class. No amount of scolding or punishment seemed to work on him.
At the end of the year, the school informed his parents that they may have to take stricter measures if such behavior continued. Thus, Rohit’s parents decided to consult a therapist and subsequently learned that their son had been suffering from disruptive mood dysregulation disorder.
Symptoms of DMDD
Children suffering from disruptive mood dysregulation disorder may experience situations and incidents more intensely than other children. They may also lack any self-regulation skills appropriate for their age to control such feelings.
According to the NIMH 5 NIMH» Disruptive Mood Dysregulation Disorder. (2017, January). Www.nimh.nih.gov. Available from: https://www.nimh.nih.gov/health/topics/disruptive-mood-dysregulation-disorder-dmdd/disruptive-mood-dysregulation-disorder , children or adolescents with DMDD usually display the following symptoms:
- Frequent display of tantrums and outbursts that are not age-appropriate and are out of proportion to the situation
- Intense verbal (yelling, screaming) or behavioral (physical aggression) temper outbursts for at least 3 times per week, on average
- Persistent angry or irritable mood between tantrums, most of the time, almost every day
- Irritability and difficulty in functioning in more than one aspect of life, such as school, home, or in a social setting
As children age, their symptoms may also change.
- They may find it difficult to adjust to school
- They may have trouble establishing healthy relationships with their peers or family members.
Read More About Mood Disorders Here
Causes Of DMDD
The exact causes of disruptive mood dysregulation disorder are unknown. However, common contributing factors 6 Weis R (2014). Introduction to abnormal child and adolescent psychology (2nd ed.). CA: SAGE. p. 477. ISBN 9781452225258. may include:
- Negative childhood experiences
- Genetic factors
- Co-occurring mental conditions and,
- Temperament 7 Dougherty, L. R., Smith, V. C., Bufferd, S. J., Carlson, G. A., Stringaris, A., Leibenluft, E., & Klein, D. N. (2014). DSM-5 disruptive mood dysregulation disorder: correlates and predictors in young children. Psychological medicine, 44(11), 2339–2350. https://doi.org/10.1017/S0033291713003115 vulnerabilities (eg: irritability, anxiousness, moodiness, difficult behavior)
Other common risk factors of disruptive mood dysregulation disorder are:
- Poor parental support
- Family conflicts
- Parental hostility
- Substance use
- Disciplinary problems at school
- Pre-existing mental health conditions
Research 8 Copeland, W. E., Angold, A., Costello, E. J., & Egger, H. (2013). Prevalence, comorbidity, and correlates of DSM-5 proposed disruptive mood dysregulation disorder. The American journal of psychiatry, 170(2), 173–179. https://doi.org/10.1176/appi.ajp.2012.12010132 shows that the condition usually develops during early childhood. Moreover, it may also occur with some other mental health conditions, like:
- Oppositional defiant disorder
- Depressive disorders
- Attention deficit hyperactivity disorder
- Anxiety disorders
Read More About Anxiety Here
Diagnosing DMDD
According to the DSM-5, the diagnosis of disruptive mood dysregulation disorder necessitates persistent, severe, frequent, and out-of-proportion temper outbursts. The diagnostic criteria 9 Rao U. (2014). DSM-5: disruptive mood dysregulation disorder. Asian journal of psychiatry, 11, 119–123. https://doi.org/10.1016/j.ajp.2014.03.002 for DMDD are similar to that of severe mood dysregulation (SMD).
The criteria for diagnosing DMDD include the following:
- Recurrent and severe temper outbursts 10 Rao U. (2014). DSM-5: disruptive mood dysregulation disorder. Asian journal of psychiatry, 11, 119–123. https://doi.org/10.1016/j.ajp.2014.03.002 (verbally and/or behaviorally) at least 3 times a week or more. It should be inappropriate in duration and intensity to the situation. The outbursts must also be “inconsistent with the developmental level”.
- Persistently angry or irritable mood between temper outbursts present throughout the day and is observed by others almost every day.
- There can be no symptom-free period for more than 3 consecutive months and all the symptoms mentioned above must be experienced during a period of 12 months or more.
- The behaviors and symptoms must be experienced in multiple settings. It should be present in an extreme degree in at least one setting.
- The first diagnosis should not be made before the child is 6 years old or after 18 years of age. Onset should be before the age of 10.
In order to diagnose disruptive mood dysregulation disorder, a mental health professional usually takes a detailed history of the child from both the parent and the child. Apart from this, they may also conduct psychometric tests and recommend certain medical tests to rule out other factors, like developmental disability or the effects of substance abuse.
Currently, there is a lack of well-validated assessments for disruptive mood dysregulation disorder. However, some use the Kiddie Schedule for Affective Disorders and Schizophrenia for School-Aged Children 11 Baweja, R., Mayes, S. D., Hameed, U., & Waxmonsky, J. G. (2016). Disruptive mood dysregulation disorder: current insights. Neuropsychiatric disease and treatment, 12, 2115–2124. https://doi.org/10.2147/NDT.S100312 .
Read More About Schizophrenia Here
Treatment Of DMDD
As disruptive mood dysregulation disorder is a new diagnosis, not a lot of research has been conducted on its treatment. Thus, professionals generally use treatment methods that have proven helpful for disorders with similar symptoms, such as anxiety and ADHD.
Fortunately, most of these treatment options work effectively for disruptive mood dysregulation disorder in children. It is recommended that parents and healthcare providers work together to come up with the best treatment option 12 Disruptive Mood Dysregulation Disorder. (n.d.). National Institute of Mental Health (NIMH). https://www.nimh.nih.gov/health/topics/disruptive-mood-dysregulation-disorder-dmdd/disruptive-mood-dysregulation-disorder .
Psychological treatments and/or medication may be used for the treatment of disruptive mood dysregulation disorder, depending on the severity of symptoms, and individual preferences. While psychotherapy is considered as the first line of treatment for this condition, medication may be prescribed to speed up the recovery process.
Psychological treatments
Various types of psychological treatments 13 Kircanski, K., Clayton, M. E., Leibenluft, E., & Brotman, M. A. (2018). Psychosocial Treatment of Irritability in Youth. Current treatment options in psychiatry, 5(1), 129–140. https://doi.org/10.1007/s40501-018-0141-5 may be utilized for treating a child suffering from disruptive mood dysregulation disorder, such as:
- Psychotherapy
- Parent training
- Computer-based training
Let us take a closer look at each of these options:
A. Psychotherapy
The most common type of psychotherapy used for treating disruptive mood dysregulation disorder in children and teens is cognitive-behavioral therapy (CBT 14 Tudor, M. E., Ibrahim, K., Bertschinger, E., Piasecka, J., & Sukhodolsky, D. G. (2016). Cognitive-Behavioral Therapy for a 9-Year-Old Girl With Disruptive Mood Dysregulation Disorder. Clinical case studies, 15(6), 459–475. https://doi.org/10.1177/1534650116669431 ). It enables children to learn how to cope with difficult thoughts and emotions that may result in feelings of anxiety or depression. CBT is also helpful in teaching various coping skills for effectively regulating mood, managing anger, and improving tolerance for frustration.
Read More About Cognitive Behavioral Therapy (CBT) Here
Dialectical behavior therapy for children (DBT-C) can also be used in the treatment of DMDD. It teaches children how to avoid prolonged, extreme outbursts and regulate moods & emotions by being more mindful. DBT-C has been proven to increase adaptive coping skills in children and significantly reduce their depressive symptoms 15Perepletchikova, F., Axelrod, S. R., Kaufman, J., Rounsaville, B. J., Douglas-Palumberi, H., & Miller, A. L. (2011). Adapting Dialectical Behaviour Therapy for Children: Towards a New Research Agenda for Paediatric Suicidal and Non-Suicidal Self-Injurious Behaviours. Child and adolescent mental health, 16(2), 116–121. https://doi.org/10.1111/j.1475-3588.2010.00583.x .
B. Parent training
This involves teaching parents certain strategies for effectively responding to temper outbursts and strengthening the parent-child relationship. Moreover, it also teaches them how to reduce irritable behavior and aggression, avoid supporting unpleasant behavior, reward positive behavior and calm the child.
Parent training can help caregivers spend more quality time with the child and manage their behavior better 16 Baweja, R., Mayes, S. D., Hameed, U., & Waxmonsky, J. G. (2016). Disruptive mood dysregulation disorder: current insights. Neuropsychiatric disease and treatment, 12, 2115–2124. https://doi.org/10.2147/NDT.S100312 .
C. Computer-based training
Currently, new treatment methods are being researched to understand how mobile and computer-based platforms may improve certain symptoms of disruptive mood dysregulation disorder in children. It is theorized that irritable children and adolescents with DMDD are more likely to misperceive 17 Imaging Studies Help Pinpoint Child Bipolar Circuitry. (n.d.). National Institute of Mental Health (NIMH). Retrieved August 30, 2022, from https://www.nimh.nih.gov/archive/news/2010/imaging-studies-help-pinpoint-child-bipolar-circuitry ambiguous facial expressions, which computer-based training can help with.
Medications
Presently, there is no specific medication for the treatment of disruptive mood dysregulation disorder in children or adolescents that has been approved by the U.S. Food and Drug Administration (FDA 18 Research, C. for D. E. and. (2019). FDA Drug Safety Communication: Safety Review Update of Medications used to treat Attention-Deficit/Hyperactivity Disorder (ADHD) in children and young adults. FDA. Available from: https://www.fda.gov/drugs/drug-safety-and-availability/fda-drug-safety-communication-safety-review-update-medications-used-treat-attention ). However, doctors may prescribe medicines 19 NIMH» Disruptive Mood Dysregulation Disorder. (2017, January). Www.nimh.nih.gov. Available from: https://www.nimh.nih.gov/health/topics/disruptive-mood-dysregulation-disorder-dmdd/disruptive-mood-dysregulation-disorder that have proven to be useful for other similar disorders, such as:
A. Stimulants
Stimulants are generally used for the treatment of ADHD. Research shows that stimulant medications can substantially help in reducing irritability in children. However, it should not be prescribed to individuals with severe heart problems.
B. Antidepressants
This type of medication can help to treat mood problems and irritability in children with disruptive mood dysregulation disorder. Antidepressants, like citalopram, can be effective for this condition but it may lead to suicidal thoughts in children. Hence, it is crucial that parents closely monitor the child taking such medications.
Read More About Antidepressants Here
C. Atypical antipsychotic
Medications such as aripiprazole and risperidone may be prescribed to children with intense irritability, severe temper outbursts, and aggression.
However, they may have some serious side effects, like weight gain, hormone changes, movement disorders, sedation, and suicidal tendencies. This is why these medications are only used when other treatment options have proved ineffective.
Parents are advised to contact their healthcare provider immediately in case their child experiences any side effects. The medication should not be stopped without consultation as doing so might result in the condition worsening.
Tips For Parents
Parents and caregivers of children with disruptive mood dysregulation disorder may often feel stressed, anxious, and overwhelmed. It is thus important to know how to handle children with this condition and function better.
Here are some effective coping strategies for parents of children with DMDD:
- Learn about the condition (eg: risk factors, prognosis, treatment options, etc.) to be better equipped to deal with it.
- Identify the triggers for your child’s temper outbursts, and observe the settings in which they occur, so you can anticipate and try to control such situations.
- Talk to others (eg: counselors, teachers or other parents) to understand why your child may be behaving in this way and share your own feelings.
- Make sure your child is safe. Keep sharp objects and potentially dangerous items away from children who may get aggressive and supervise them as much as possible.
- Teach your child valuable coping skills, like deep breathing, reciting affirmations, or singing songs for when they become frustrated or angry.
- Motivate them to behave positively, by rewarding appropriate behaviors with praise, attention and certain privileges. Try to ignore their misbehavior, as it may often be an attempt to garner attention.
- Practice self-care. In order to be able to take care of your child, you should also take care of your own mental and physical health by eating nutritious food, sleeping well, exercising, etc.
- Seek professional help whenever required.
Takeaway
Disruptive mood dysregulation disorder is a challenging disorder that can be hard to identify and diagnose. Moreover, it can lead to serious problems in different aspects of a child’s life.
If left untreated, it may also result in anxiety and depression in their adulthood affecting their ability to function in daily life. In case you suspect that your child may be suffering from DMDD, try to seek help immediately.
At A Glance
- Disruptive mood dysregulation disorder is a mood disorder which makes it difficult for children to regulate and manage their emotions in an appropriate way.
- The condition usually develops before the age of 10.
- One of the most common risk factors for the onset of DMDD is the temperament of a child.
- Psychological treatments are considered as the first-line of treatment for this condition.
- Medication may also be prescribed to speed up the recovery.
- Certain practices, such as identifying triggers and practicing self care can help parents in coping with disruptive mood dysregulation disorder better.
Frequently Asked Questions (FAQs)
1. Is disruptive mood dysregulation disorder the same as conduct disorder?
No. While DMDD shares several symptoms with conduct disorder, the former is predominantly based on mood disturbances whereas the latter primarily involves defiant and vindictive behavior 20 Mayes, S. D., Waxmonsky, J. D., Calhoun, S. L., & Bixler, E. O. (2016). Disruptive Mood Dysregulation Disorder Symptoms and Association with Oppositional Defiant and Other Disorders in a General Population Child Sample. Journal of child and adolescent psychopharmacology, 26(2), 101–106. https://doi.org/10.1089/cap.2015.0074 .
2. Is DMDD an intellectual disability?
No, disruptive mood dysregulation disorder is not an intellectual disability. In fact, children with DMDD can have normal levels of intelligence.
3. How does DMDD affect the brain?
Children with DMDD seem to have problems with selective attention and visual attention and processing, indicating problems in the parietal regions of the brain 21 Brænden, A., Zeiner, P., Coldevin, M., Stubberud, J. and Melinder, A., 2022. Underlying mechanisms of disruptive mood dysregulation disorder in children: A systematic review by means of research domain criteria. JCPP Advances, 2(1). Available from: https://acamh.onlinelibrary.wiley.com/doi/full/10.1002/jcv2.12060
4. Is DMDD permanent?
No. DMDD is a disorder that generally occurs in childhood. It can be effectively managed with psychological and medical interventions.
5. Does DMDD run in families?
There is no conclusive evidence regarding the inheritability of DMDD.
6. Can Major Depressive Disorder and DMDD coexist?
DMDD is a subtype of depression that occurs in children, and if left untreated may develop into major depressive disorder in adulthood.