Table of Contents
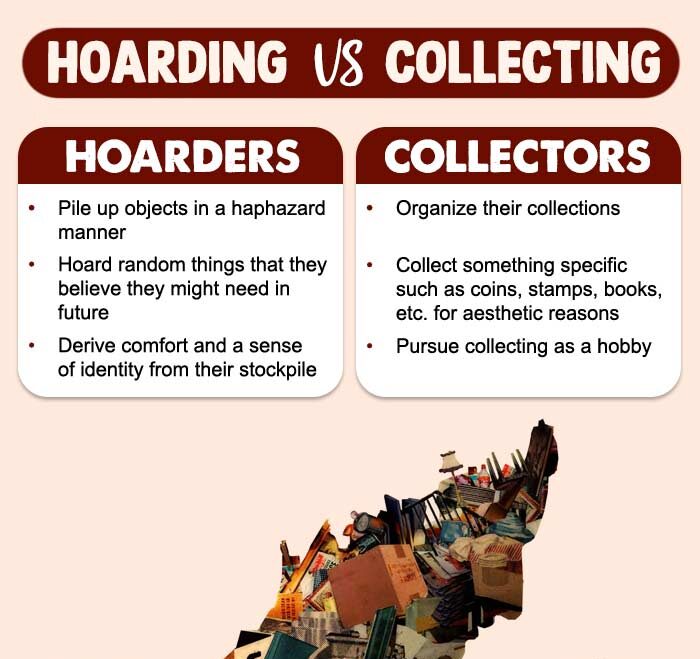
Hoarding Disorder (HD) is a recognized mental health condition characterized by a persistent difficulty discarding or parting with possessions, regardless of their actual value, due to a perceived need to save them. This often leads to excessive accumulation of items, resulting in significant clutter that disrupts living spaces and impairs daily functioning.
What Is Hoarding Disorder?
Hoarding disorder (HD) is a mental disorder 1 Vilaverde, D., Gonçalves, J., & Morgado, P. (2017). Hoarding Disorder: A Case Report. Frontiers in psychiatry, 8, 112. https://doi.org/10.3389/fpsyt.2017.00112 characterized by the urge to save and acquire new items, difficulty discarding current possessions, and excessive household clutter. It is popularly considered a subtype of obsessive-compulsive disorder and is also known as compulsive hoarding disorder. However, experts contend that it should be regarded as a separate disorder with its own unique set of symptoms.
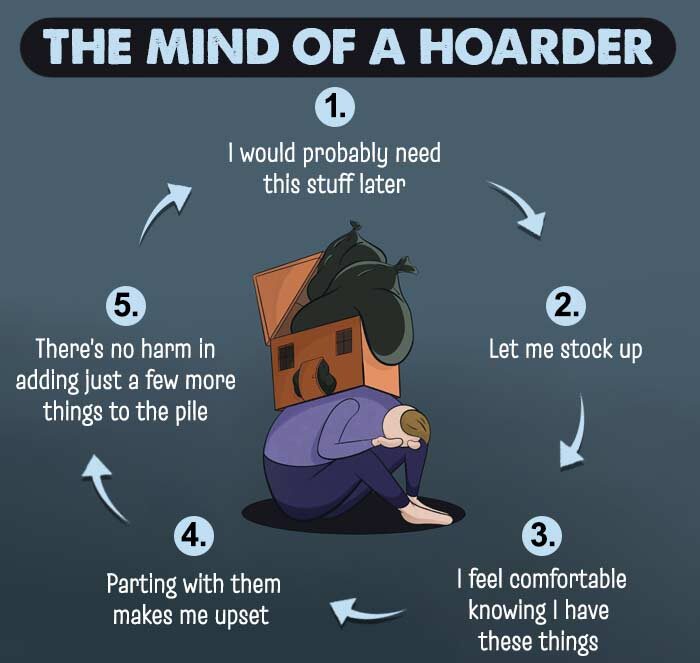
Individuals with Hoarding Disorder often exhibit cognitive distortions related to the perceived value, utility, or emotional significance of possessions, which contribute to persistent and disruptive behaviors. They typically engage in a chronic cycle of acquiring items—regardless of their actual worth or necessity—and experience extreme difficulty discarding them. This pattern leads to significant clutter that encroaches on functional living spaces and may compromise personal hygiene, physical safety, and the well-being of both the individual and those in their immediate environment.
From a psychological standpoint, individuals with this disorder may disproportionately derive their sense of identity and self-worth from material possessions. This attachment often stems from underlying emotional vulnerabilities, such as anxiety, perfectionism, trauma, or a fear of losing important memories, making it difficult for them to let go of even seemingly insignificant items.
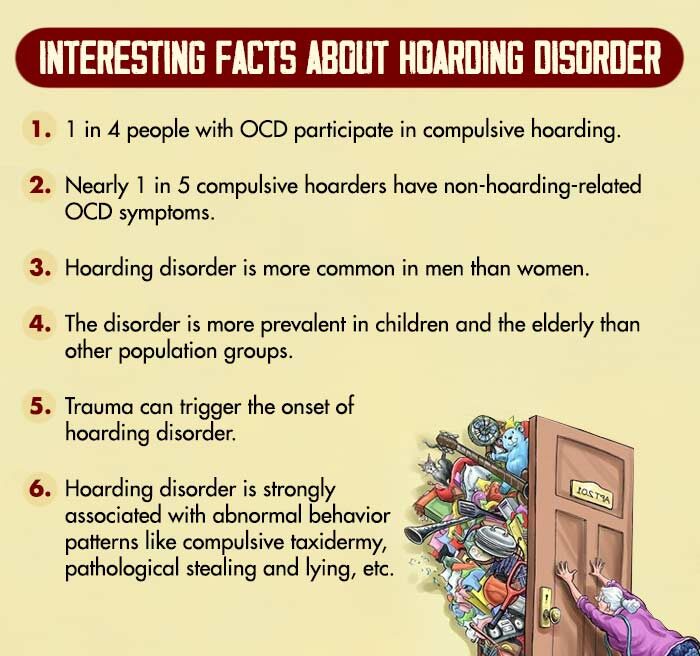
The last two decades have seen a steady rise in the number of hoarding disorder cases. Research affirms that 2–14% 2 Davidson, E. J., Dozier, M. E., Pittman, J. O. E., Mayes, T. L., Blanco, B. H., Gault, J. D., Schwarz, L. J., & Ayers, C. R. (2019). Recent Advances in Research on Hoarding. Current psychiatry reports, 21(9), 91. https://doi.org/10.1007/s11920-019-1078-0 of the global population suffers from symptoms of compulsive hoarding.
The overall prevalence 3 Jaisoorya, T. S., Thamby, A., Manoj, L., Kumar, G. S., Gokul, G. R., Narayanaswamy, J. C., Arumugham, S. S., Thennarassu, K., & Reddy, Y. C. J. (2021). Prevalence of hoarding disorder among primary care patients. Revista brasileira de psiquiatria (Sao Paulo, Brazil : 1999), 43(2), 168–173. https://doi.org/10.1590/1516-4446-2020-0846 of this disorder is higher in men (than women) 4 Vilaverde, D., Gonçalves, J., & Morgado, P. (2017). Hoarding Disorder: A Case Report. Frontiers in psychiatry, 8, 112. https://doi.org/10.3389/fpsyt.2017.00112 , the elderly population, and people with certain psychiatric disorders (like obsessive-compulsive disorder, stress disorders, etc.). However, the personal nature of hoarding and the stigma attached to mental healthcare treatment prevents people from seeking medical attention.
Case Example
Mr. Shetty, a 60-year-old man, demonstrated a longstanding pattern of acquiring and retaining items of little to no practical value. His collection included old newspapers and magazines dating back several years, empty toiletry containers, and worn-out clothing and accessories. Despite the items’ lack of utility, he was reluctant to discard them.
Over time, the extent of his hoarding became increasingly evident. His garage was filled with obsolete car parts from vehicles he no longer owned, boxes of tangled electrical cords, defunct mobile phones, outdated gadgets, and various other non-functional objects. These possessions occupied substantial portions of his living space, restricting functional use and contributing to environmental disarray.
Attempts by his adult children to clear out the clutter were met with intense emotional distress and resistance. In some cases, these interventions triggered a reactive increase in his hoarding behaviors. Mr. Shetty expressed a deep emotional attachment to his belongings, often stating, “These are marks of my existence. They are proof that I have lived a worthy life.” He did not acknowledge his behavior as problematic, demonstrating poor insight into the consequences of his condition.
A significant psychosocial trigger appears to have been the loss of his father approximately 25 years ago. Following this bereavement, Mr. Shetty began displaying compulsive behaviors centered around material possessions. He appeared preoccupied with the idea that retaining objects would preserve his legacy and affirm the meaning of his life.
Case Analysis
Mr. Shetty’s presentation is consistent with the diagnostic criteria for Hoarding Disorder, as defined by the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5). Core features observed include a persistent difficulty discarding possessions, regardless of actual value, and a resultant accumulation that compromises usable living space. His behavior has caused significant distress to family members and impaired his overall quality of life.
The absence of insight is notable, as Mr. Shetty does not recognize the dysfunctional nature of his behavior. Instead, he rationalizes his hoarding as a meaningful pursuit linked to self-worth and identity preservation. This emotional overattachment to objects, compounded by a history of unresolved grief, suggests that his hoarding may serve as a maladaptive coping mechanism for underlying emotional vulnerability and fear of loss.
Mr. Shetty’s case highlights the chronic and progressive nature of Hoarding Disorder, as well as the importance of early identification, psychoeducation, and therapeutic intervention—potentially incorporating Cognitive Behavioral Therapy (CBT) tailored for hoarding, motivational interviewing, and family support to address insight deficits and promote functional change.
Symptoms Of Hoarding Disorder
The main hoarding disorder symptoms 5 Administration, S. A. and M. H. S. (2016, June 1). Table 3.29, DSM-5 Hoarding Disorder. Www.ncbi.nlm.nih.gov. Available from: https://www.ncbi.nlm.nih.gov/books/NBK519704/table/ch3.t29/ are:
- Persistent Difficulty Discarding Possessions: An ongoing inability to discard or part with possessions, regardless of their actual value, due to a perceived need to save them or distress associated with letting them go.
- Marked Distress or Impairment: Attempts to discard possessions are accompanied by significant emotional distress, anxiety, or indecision, which often reinforces hoarding behavior.
- Accumulation Leading to Congestion of Living Spaces: Possessions accumulate to such an extent that active living areas become cluttered and unusable for their intended purpose, resulting in functional impairment and compromised quality of life.
Additionally, it is often observed that the individual’s living spaces are rendered largely unusable due to the extent of clutter, and any attempts at clearing or organizing the area typically occur only through the intervention of others.
Types of Hoarding Disorder
As per research 6 Frost, R. O., Patronek, G., & Rosenfield, E. (2011). Comparison of object and animal hoarding. Depression and anxiety, 28(10), 885–891. https://doi.org/10.1002/da.20826 , hoarding disorders can be categorized into the following types:
1. Trash hoarding disorder
Trash hoarding refers to a subtype of hoarding behavior characterized by the accumulation of items that are clearly non-functional, broken beyond repair, or have no apparent value or utility.
Commonly hoarded materials in such cases include outdated or defunct electronics, old newspapers and magazines, empty plastic or glass containers, tin cans, and various discarded packaging materials.
Despite their obvious lack of usefulness, individuals with this hoarding pattern experience significant difficulty discarding these items, often due to distorted beliefs about their potential future use or emotional attachment.
2. Food hoarding disorder
Food hoarding is a subtype of hoarding behavior in which individuals accumulate excessive quantities of edible items, often far beyond their immediate needs.
This behavior is typically driven by fears of scarcity, potential emergencies, or natural disasters. Over time, the collected food—often expired or improperly stored—can contribute to significant clutter in living areas, creating unsanitary conditions and posing health and safety risks.
Despite spoilage or contamination, individuals with this hoarding pattern may experience intense anxiety or distress at the thought of discarding food items.
3. Compulsive shopping and hoarding disorder
Individuals exhibiting this subtype of hoarding disorder often engage in indiscriminate shopping behaviors, frequently purchasing items they do not need and exceeding their financial limitations.
This pattern is commonly associated with compulsive buying disorder (CBD), a condition characterized by an irresistible urge to shop, often as a means of alleviating emotional distress.
When compulsive buying co-occurs with hoarding disorder, it can lead to excessive accumulation of items and significant financial strain, making the combined presentation a particularly complex and severe psychiatric concern.
The dual diagnosis often reflects underlying emotional dysregulation, poor impulse control, and distorted beliefs about possessions, requiring integrated clinical intervention.
4. Animal hoarding disorder
Animal hoarding is a severe and distinct subtype of hoarding disorder, characterized by the compulsive accumulation of animals—most commonly cats or dogs—beyond the individual’s capacity to provide adequate care.
Individuals with this condition often continue to acquire animals despite overcrowded living conditions, inadequate sanitation, and limited resources. They may refuse to surrender animals that are ill, suffering, or even deceased, due to distorted beliefs about their ability to care for them or deep emotional attachment.
Interventions by animal welfare authorities or law enforcement are frequently met with intense emotional distress and resistance, underscoring the complex psychological and emotional dynamics underlying this form of hoarding.
5. Sentimental hoarding disorder
Sentimental hoarding is a subtype of hoarding behavior marked by an intense emotional attachment to personal belongings associated with past experiences or significant life events. Individuals with this tendency often struggle to discard items that serve as reminders of loved ones, milestones, or meaningful places and adventures.
These objects—such as old letters, photographs, souvenirs, or clothing—are perceived as tangible connections to memories or relationships. The idea of parting with such items may evoke feelings of loss, guilt, or identity disruption, making decluttering efforts particularly distressing and emotionally charged.
Causes Of Hoarding Disorder
Research 7 Dozier, M. E., & Ayers, C. R. (2017). The Etiology of Hoarding Disorder: A Review. Psychopathology, 50(5), 291–296. https://doi.org/10.1159/000479235 attributes the development of hoarding to a combination of genetic factors, a reinforcement of beliefs surrounding reasons to save objects or vulnerability towards avoidant behaviors.
The common causes of hoarding disorder include:
1. Genetics
Twin studies suggest that up to 50% of the variance in hoarding behaviors may be genetically linked. It was also found that older adults with HD reportedly have an average of 2 biological relatives with symptoms or signs of hoarding disorder.
Read More About Genetics Here
2. Neurocognition
Premature cognitive aging and executive dysfunction, among other cognitive domains are linked to the risk of hoarding disorder.
3. Personality traits
People with certain personality traits related to perfectionism, indecision, and procrastination are more vulnerable to compulsive hoarding. Research also associates this disorder with several personality traits, namely:
- Paranoid
- Schizotypal
- Avoidant
- Obsessive-compulsive, etc.
Read More About Paranoid Here
4. Trauma
People with a history of trauma or those who have endured a stressful life event (positive or negative) are prone to hoarding disorder.
5. Cultural beliefs
Hoarding disorder can also result from certain beliefs about material possessions that are transmitted across generations in certain cultures.
Mental Health Effects of Hoarding
People with Hoarding Disorder often experience a range of associated problems stemming from their condition. They are at a higher risk of developing comorbid psychiatric conditions such as major depressive disorder, anxiety disorders (including generalized anxiety and social anxiety), obsessive-compulsive disorder (OCD), and attention-deficit/hyperactivity disorder (ADHD). In addition to psychological distress, hoarding behavior can lead to significant functional impairment, including social isolation, strained family relationships, financial difficulties, and health hazards due to unsanitary living conditions or increased risk of fire and injury. The cumulative effect of these challenges can profoundly affect the individual’s overall quality of life and daily functioning.
Common Psychiatric Comorbidities Associated with Hoarding Disorder:
- Major Depressive Disorder (Severe Depression): Persistent feelings of sadness, hopelessness, and low energy are frequently observed in individuals with hoarding disorder. Depression may both contribute to and worsen hoarding behavior by reducing motivation and increasing emotional dependence on possessions.
- Obsessive-Compulsive Disorder (OCD): While hoarding was once classified as a subtype of OCD, it is now recognized as a distinct disorder. However, a significant number of individuals with hoarding disorder may exhibit overlapping obsessive-compulsive symptoms, such as intrusive thoughts and compulsive rituals.
- Schizophrenia and Other Psychotic Disorders: In some cases, hoarding behavior may co-occur with psychotic conditions, especially when delusional beliefs are present (e.g., believing that certain items have supernatural significance or must be preserved for safety). Insight is typically poor in such cases.
- Anxiety Disorders: Generalized anxiety disorder, social anxiety disorder, and panic disorder are commonly observed in individuals with hoarding disorder. Anxiety often drives acquisition and intensifies the fear of discarding items, reinforcing the hoarding cycle.
- Attention-Deficit/Hyperactivity Disorder (ADHD): Impulsivity, poor organizational skills, and difficulty with sustained attention may contribute to disorganized accumulation and a reduced ability to manage clutter effectively.
Individuals with Hoarding Disorder are also more likely to experience social isolation and to live alone, often as a consequence of strained interpersonal relationships. Their hoarding behaviors can lead to significant conflicts with family members, caregivers, or neighbors, primarily due to concerns over safety, hygiene, and shared living space. Over time, this interpersonal distress may contribute to avoidance of social interaction, further reinforcing isolation and reducing opportunities for support or intervention.
Read More About Schizophrenia Here
Diagnosis Of Hoarding Disorder
Hoarding disorder (HD) is classified as a mental disorder in the obsessive-compulsive spectrum 8 Mataix-Cols, D., Frost, R. O., Pertusa, A., Clark, L. A., Saxena, S., Leckman, J. F., Stein, D. J., Matsunaga, H., & Wilhelm, S. (2010). Hoarding disorder: a new diagnosis for DSM-V?. Depression and anxiety, 27(6), 556–572. https://doi.org/10.1002/da.20693 in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5). It has been widely recognized as an independent condition that mandates help.
Mental health professionals (MHPs) typically begin by conducting a comprehensive clinical interview to obtain a detailed history of the individual’s symptoms, behaviors, and psychosocial context. This process helps establish an accurate diagnosis and rule out other psychiatric or medical conditions that may present with similar features. In addition, MHPs may administer standardized psychological assessments—such as the Saving Inventory-Revised (SI-R) or the Hoarding Rating Scale—to evaluate the severity of symptoms, level of insight, and functional impairment. These evaluations are critical in guiding the development of a tailored treatment plan.
Treatment For Hoarding Disorder
Hoarding disorder treatment 9 Mathews C. A. (2014). Hoarding disorder: more than just a problem of too much stuff. The Journal of clinical psychiatry, 75(8), 893–894. https://doi.org/10.4088/JCP.14ac09325 usually entails:
1. Medication
Several medications 10 Nakao, T., & Kanba, S. (2019). Pathophysiology and treatment of hoarding disorder. Psychiatry and clinical neurosciences, 73(7), 370–375. https://doi.org/10.1111/pcn.12853 are administered for dealing with hoarding disorder. These include:
- Selective serotonin reuptake inhibitors (SSRIs)
- Serotonin-norepinephrine reuptake inhibitors (SNRIs)
- Stimulants, etc.
Read More About Antidepressants Here
2. Psychotherapy
Cognitive-Behavioral Therapy (CBT) is currently the most evidence-based and widely utilized treatment approach for Hoarding Disorder. It focuses on identifying and restructuring cognitive distortions related to the perceived need to save items and the distress associated with discarding them. In conjunction with CBT, motivational interviewing is often employed to enhance the individual’s readiness for change, especially when insight is limited. Harm reduction strategies may also be integrated, aiming to minimize immediate safety risks while gradually addressing hoarding behaviors.
A core component of CBT for hoarding involves exposure-based interventions, in which individuals are supported in systematically sorting, organizing, and discarding items—either during therapy sessions or through structured assignments at home. This behavioral work is often accompanied by skills training in decision-making, organization, and emotional regulation, helping to reduce avoidance and foster long-term functional improvement.
Read More About CBT Here
How To Overcome Hoarding Disorder
The first and most crucial step in overcoming Hoarding Disorder is developing awareness of the problem and cultivating a willingness to change. Acknowledging the emotional and functional impact of hoarding and being open to receiving professional help are foundational to the recovery process.
While professional treatment is often necessary, individuals may also benefit from the following self-help strategies to support their progress:
- Set regular reminders to declutter: Schedule short, manageable sessions every few days to sort through and organize your belongings. Consistency, rather than intensity, often leads to lasting progress.
- Accept help and support: Reach out to trusted friends, family members, or caregivers who can assist you in organizing your space. Allowing others to help can ease the emotional burden and provide perspective.
- Communicate openly and build community: Share your experiences with those close to you and consider joining a support group for individuals coping with hoarding disorder. Knowing you’re not alone can be a powerful motivator.
- Start small and stay focused: Begin by discarding items you haven’t used in the last two to three years. Avoid overwhelming yourself by setting achievable, clearly defined goals.
- Challenge your beliefs about possessions: Make a list of items you believe are indispensable. Then, write down the perceived consequences of discarding them. Ask yourself: Would my daily life truly be affected without this? This exercise can help identify irrational thoughts linked to hoarding.
- Seek professional help when needed: If managing the condition alone becomes overwhelming, do not hesitate to consult a mental health professional. Evidence-based treatments like Cognitive Behavioral Therapy (CBT) are available and effective.
- Reconnect with your personal values: Remind yourself that your self-worth is not determined by the number or type of possessions you own. Focus on goals, relationships, and experiences that bring lasting meaning to your life.
Takeaway
Hoarding Disorder is now recognized as a serious and debilitating mental health condition that can significantly impair an individual’s physical health, daily functioning, occupational performance, and interpersonal relationships. Left untreated, it may lead to hazardous living conditions, social isolation, and severe emotional distress. Therefore, early identification and appropriate, evidence-based intervention are crucial to preventing long-term consequences and improving overall quality of life.
At A Glance
- Hoarding Disorder (HD) is a recognized mental health condition characterized by a persistent and compulsive urge to acquire and accumulate possessions, often regardless of their actual value. Individuals with this disorder also experience significant difficulty discarding items, leading to excessive clutter that disrupts living spaces and daily functioning.
- If left untreated, hoarding disorder can severely impact a person’s personal well-being, professional performance, and social relationships, often resulting in emotional distress, health hazards, and social isolation.
- However, with timely intervention, hoarding disorder can be effectively managed through a combination of psychotherapy—particularly Cognitive Behavioral Therapy (CBT)—pharmacotherapy, and structured self-help strategies aimed at improving organization, decision-making, and emotional regulation.
Frequently Asked Questions (FAQs)
1. What is the difference between hoarding disorder and obsessive-compulsive disorder?
A person suffering from obsessive-compulsive disorder (OCD) experiences frequent and persistent thoughts, urges, or images about some object or situation. Hoarding disorder, on the other hand, is the compulsive acquisition of items and the difficulty in letting go of them. Although hoarding disorder is historically considered a subtype of OCD, it is a separate clinical condition.
2. Who are some fictional characters with hoarding disorder?
Ariel from Disney’s “Little Mermaid” and the protagonists in films like Unstrung Heroes (1995), Girl with Black Balloons (2010), and Clutter (2013) are some fictional characters with hoarding disorder.
3. What do obsessive-compulsive disorder, body dysmorphic disorder, and hoarding disorder have in common?
Obsessive-compulsive disorder, body dysmorphic disorder, and hoarding disorder—all three mental health disorders are characterized by repetitive and uncontrollable thoughts and urges to engage in a particular behavior or situation.
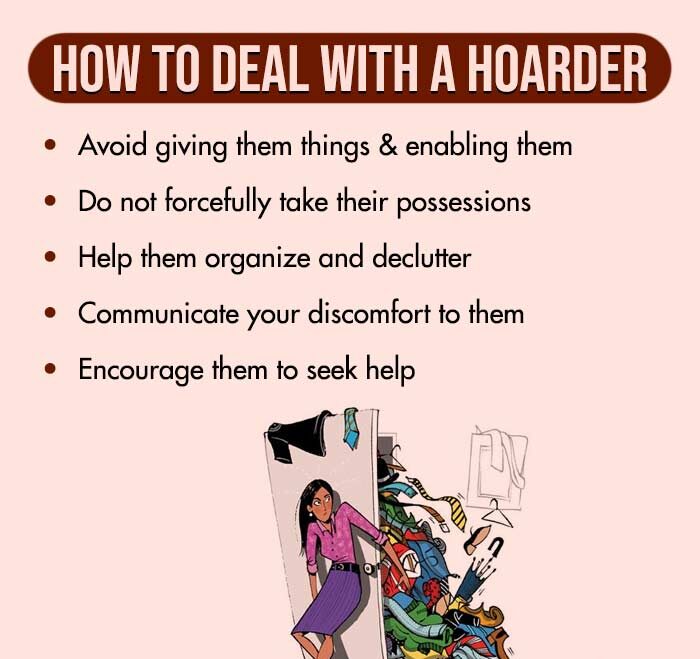
4. How can we help someone with a hoarding disorder?
Empathize and use respectful language to communicate your concerns. Don’t focus on a total clean-up; instead, try to be supportive. Help them navigate through decluttering and therapy with kindness and understanding.