Living with someone with mental illness can be extremely difficult and stressful for caregivers. The demands of providing care and support can lead to emotional, physical, and financial burdens, such as feelings of guilt, social isolation, and burnout. These challenges can take a toll on caregivers’ well-being and their relationships with their loved ones.
What Is It Like Living With Someone With Mental Illness?
Experiencing a mental illness can have a profound impact on various aspects of life, including personal relationships with friends and family members.
Coping with a 1 Nenobais, A., Jatimi, A., & Jufriyanto, M. (2019). Family Burden for the Caregivers of People with Mental Disorders: A Systematic Review. Jurnal Ners, 14(3), 26. https://doi.org/10.20473/jn.v14i3.16971 who is struggling with mental illness can be particularly challenging, as it often requires managing unpredictable mood swings and navigating crises, while also dealing with the overall impact on daily life.
Research indicates that a considerable percentage of caregivers, ranging from 32% to 71% 2 Urizar, G. G., Jr, Ramírez, I., Caicedo, B. I., & Mora, C. (2022). Mental health outcomes and experiences of family caregivers of children with disabilities during the COVID-19 pandemic in Bolivia. Journal of community psychology, 50(6), 2682–2702. https://doi.org/10.1002/jcop.22763 , experience poor mental health outcomes such as stress, anxiety, and depression, particularly those experiencing poor health or using maladaptive coping strategies.
Caregivers may feel overwhelmed and stressed due to the demands of providing care and support, which can result in burnout and physical and emotional exhaustion. They may also experience guilt, and shame about their loved one’s condition and struggle to balance their own needs with the needs of their loved one.
Read More About Caregiving Here
Living With A Family Member With Mental Illness
Several mental illnesses can have many significant impacts on family caregivers 3 Chang, H. Y., Chiou, C. J., & Chen, N. S. (2010). Impact of mental health and caregiver burden on family caregivers’ physical health. Archives of gerontology and geriatrics, 50(3), 267–271. https://doi.org/10.1016/j.archger.2009.04.006 , such as:
1. Living with someone with Schizophrenia
Schizophrenia is a chronic mental illness that can cause hallucinations 4 Lippi G. (2016). Schizophrenia in a member of the family: Burden, expressed emotion and addressing the needs of the whole family. The South African journal of psychiatry : SAJP : the journal of the Society of Psychiatrists of South Africa, 22(1), 922. https://doi.org/10.4102/sajpsychiatry.v22i1.922 , delusions, and disordered thinking. Caregivers of people with schizophrenia may experience social isolation, financial strain from medical costs, and difficulty understanding and coping with the person’s symptoms.
Read More About Schizophrenia Here
2. Living with someone with Bipolar Disorder
Bipolar disorder involves extreme mood swings 5 Jain, A., & Mitra, P. (2022). Bipolar Affective Disorder. PubMed; StatPearls Publishing. Available from: https://www.ncbi.nlm.nih.gov/books/NBK558998/ between high-energy manic episodes and low-energy depressive episodes. Caregivers of people with bipolar disorder may experience high levels of stress from trying to manage the person’s unpredictable behavior and mood swings, as well as difficulty communicating with the person during manic or depressive episodes.
Read More About Bipolar Disorder Here
3. Living with someone with Anxiety Disorder
Anxiety disorders involve excessive worry 6 Chand, S. P., & Marwaha, R. (2022). Anxiety. PubMed; StatPearls Publishing. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470361/ or fear about everyday situations, leading to physical symptoms like rapid heartbeat and sweating. Caregivers of people with anxiety may experience stress and burnout from constantly monitoring and reassuring the person, as well as difficulty understanding and coping with the person’s fears and worries.
Read More About Anxiety Disorder Here
4. Living with someone with Autistic Spectrum Disorder (ASD)
People with ASD may be hypersensitive 7 Mughal, S., Faizy, R. M., & Saadabadi, A. (2020). Autism Spectrum Disorder (Regressive Autism, Child Disintegrative Disorder). PubMed; StatPearls Publishing. Available from: https://www.ncbi.nlm.nih.gov/books/NBK525976/ to certain sensory stimuli, such as noise, touch, or smell and also they may have rigid routines and interests that they are unwilling to deviate from, which can make it challenging to introduce new activities or experiences.
5. Living with someone with a Personality Disorder
Caregivers of people with personality disorders may experience difficulty 8 Fariba, K., Gupta, V., & Kass, E. (2020). Personality Disorder. PubMed; StatPearls Publishing. Available from: https://www.ncbi.nlm.nih.gov/books/NBK556058/ managing the person’s unpredictable or impulsive behavior, as well as difficulty understanding and coping with the person’s emotional volatility and intense relationships.
Read More About Personality Disorders Here
What Causes Stress For Someone Living With Mental Illness?
Here are some possible causes of burnout or stress for caregivers or someone living with a person suffering from mental illness:
- Constantly managing the needs 9 Schulz, R., & Sherwood, P. R. (2008). Physical and mental health effects of family caregiving. The American journal of nursing, 108(9 Suppl), 23–27. https://doi.org/10.1097/01.NAJ.0000336406.45248.4c of a person with mental illness, can be demanding and draining
- Lack of self-care or personal time, leading to exhaustion and burnout 10 Broxson, J., & Feliciano, L. (2020). Understanding the Impacts of Caregiver Stress. Professional case management, 25(4), 213–219. https://doi.org/10.1097/NCM.0000000000000414
- Financial strain from medical bills, treatment costs 11 Chadda R. K. (2014). Caring for the family caregivers of persons with mental illness. Indian journal of psychiatry, 56(3), 221–227. https://doi.org/10.4103/0019-5545.140616 , or caregiving expenses
- Struggling to balance caregiving responsibilities 12 Alyafei, A. H., Alqunaibet, T., Mansour, H., Ali, A., & Billings, J. (2021). The experiences of family caregivers of people with severe mental illness in the Middle East: A systematic review and meta-synthesis of qualitative data. PloS one, 16(7), e0254351. https://doi.org/10.1371/journal.pone.0254351 with other obligations, such as work or family responsibilities
- Worrying about the person with mental illness and their future 13 Moss, K. O., Kurzawa, C., Daly, B., & Prince-Paul, M. (2019). Identifying and Addressing Family Caregiver Anxiety. Journal of hospice and palliative nursing : JHPN : the official journal of the Hospice and Palliative Nurses Association, 21(1), 14–20. https://doi.org/10.1097/NJH.0000000000000489
- Dealing with stigma or judgment 14 Rössler W. (2016). The stigma of mental disorders: A millennia-long history of social exclusion and prejudices. EMBO reports, 17(9), 1250–1253. https://doi.org/10.15252/embr.201643041 from others about the person’s mental illness
How Mental Illness Affects Relationships
Mental health symptoms or long-term illness can affect relationships in the following ways:
1. Communication Difficulties
Symptoms of mental illness, such as depression or anxiety, can make it difficult to communicate effectively with a partner. People with mental illness may withdraw from social interactions 15 Palmer, A. D., Newsom, J. T., & Rook, K. S. (2016). How does difficulty communicating affect the social relationships of older adults? An exploration using data from a national survey. Journal of communication disorders, 62, 131–146. https://doi.org/10.1016/j.jcomdis.2016.06.002 or struggle to express their thoughts and feelings, leading to misunderstandings or conflicts in the relationship.
2. Changes in Behavior
Mental illness or long-term illness can cause changes in behavior 16 Aung, M. H., Matthews, M., & Choudhury, T. (2017). Sensing behavioral symptoms of mental health and delivering personalized interventions using mobile technologies. Depression and anxiety, 34(7), 603–609. https://doi.org/10.1002/da.22646 , such as irritability, withdrawal, or mood swings, which can affect a relationship badly in many ways.
3. Changes in Intimacy
Mental illness or long-term illness can affect sexual desire 17 Bonfils, K. A., Firmin, R. L., Salyers, M. P., & Wright, E. R. (2015). Sexuality and intimacy among people living with serious mental illnesses: Factors contributing to sexual activity. Psychiatric rehabilitation journal, 38(3), 249–255. https://doi.org/10.1037/prj0000117 , physical ability, or emotional connection, which can impact intimacy in a relationship.
4. Role Changes
Living with someone who has mental health issues may require one partner to take on a caregiving role 18 Mokoena, A. G., Poggenpoel, M., Myburgh, C., & Temane, A. (2019). Lived experiences of couples in a relationship where one partner is diagnosed with a mental illness. Curationis, 42(1), e1–e7. https://doi.org/10.4102/curationis.v42i1.2015 , which can change the relationship dynamic and create new challenges.
5. Impact on Social Life
Mental illness or long-term illness can limit social activities 19 Mushtaq, R., Shoib, S., Shah, T., & Mushtaq, S. (2014). Relationship between loneliness, psychiatric disorders and physical health ? A review on the psychological aspects of loneliness. Journal of clinical and diagnostic research : JCDR, 8(9), WE01–WE4. https://doi.org/10.7860/JCDR/2014/10077.4828 or cause isolation, which can affect the couple’s social life and support system.
Tips For Helping A Loved One Cope With Mental Illness
The following are some tips that may be useful for living well 20 Muralidharan, A., Brown, C. H., E Peer, J., A Klingaman, E., M Hack, S., Li, L., Walsh, M. B., & Goldberg, R. W. (2019). Living Well: An Intervention to Improve Medical Illness Self-Management Among Individuals With Serious Mental Illness. Psychiatric services (Washington, D.C.), 70(1), 19–25. https://doi.org/10.1176/appi.ps.201800162 with a loved one with mental illness:
- Educate yourself about the person’s mental illness and its symptoms, so you can better understand 21 Mannarini, S., Rossi, A., & Munari, C. (2020). How do education and experience with mental illness interact with causal beliefs, eligible treatments and stigmatising attitudes towards schizophrenia? A comparison between mental health professionals, psychology students, relatives and patients. BMC psychiatry, 20(1), 167. https://doi.org/10.1186/s12888-020-02580-6 their behavior and ways to respond to it.
- Encourage the person to seek treatment 22 Thomas, S., Jenkins, R., Burch, T., Calamos Nasir, L., Fisher, B., Giotaki, G., Gnani, S., Hertel, L., Marks, M., Mathers, N., Millington-Sanders, C., Morris, D., Ruprah-Shah, B., Stange, K., Thomas, P., White, R., & Wright, F. (2016). Promoting Mental Health and Preventing Mental Illness in General Practice. London journal of primary care, 8(1), 3–9. https://doi.org/10.1080/17571472.2015.1135659 for their mental illness and support them in their recovery journey.
- Communicate openly and honestly 23 Milton, A. C., Mullan, B., MacCann, C., & Hunt, C. (2018). An evaluation of communication barriers and facilitators at the time of a mental health diagnosis: a survey of health professional practices. Epidemiology and psychiatric sciences, 27(4), 357–368. https://doi.org/10.1017/S2045796016001153 with the person about your feelings and concerns, and listen actively to their perspective.
- Set boundaries to protect your own mental health and well-being, and also practice self-care 24 Karimirad, M. R., Seyedfatemi, N., Mirsepassi, Z., Noughani, F., & Cheraghi, M. A. (2022). Barriers to Self-Care Planning for Family Caregivers of Patients with Severe Mental Illness. Journal of patient experience, 9, 23743735221092630. https://doi.org/10.1177/23743735221092630 on a regular basis.
- Seek support 25 Sun, X., Ge, J., Meng, H., Chen, Z., & Liu, D. (2019). The Influence of Social Support and Care Burden on Depression among Caregivers of Patients with Severe Mental Illness in Rural Areas of Sichuan, China. International journal of environmental research and public health, 16(11), 1961. https://doi.org/10.3390/ijerph16111961 from friends, families, or mental health professionals, such as therapists or support groups.
- Practice empathy and compassion 26 Román-Sánchez, D., Paramio-Cuevas, J. C., Paloma-Castro, O., Palazón-Fernández, J. L., Lepiani-Díaz, I., de la Fuente Rodríguez, J. M., & López-Millán, M. R. (2022). Empathy, Burnout, and Attitudes towards Mental Illness among Spanish Mental Health Nurses. International journal of environmental research and public health, 19(2), 692. https://doi.org/10.3390/ijerph19020692 towards the person, recognizing that mental illness can be a difficult and painful experience.
- Don’t take the person’s behavior personally, and avoid blaming or shaming 27 Leshner A. I. (2019). Stop blaming mental illness. Science (New York, N.Y.), 365(6454), 623. https://doi.org/10.1126/science.aaz0997 them for their symptoms.
- Focus on the person’s strengths and positive qualities, and celebrate their accomplishments and progress 28 Prevo, L., Kremers, S., & Jansen, M. (2020). Small Successes Make Big Wins: A Retrospective Case Study towards Community Engagement of Low-SES Families. International journal of environmental research and public health, 17(2), 612. https://doi.org/10.3390/ijerph17020612 .
- Remember that recovery from 29 Buila, S. M., & Swanke, J. R. (2010). Patient-centered mental health care: encouraging caregiver participation. Care management journals : Journal of case management ; The journal of long term home health care, 11(3), 146–150. https://doi.org/10.1891/1521-0987.11.3.146 mental illness is a process that takes time, and be patient and supportive throughout the journey.
Takeaway
Living well and caring for someone with a mental illness requires patience, understanding, and a willingness to adapt and support each other. It is essential to recognize that mental illness is a medical condition and needs to be treated with care and compassion. However, with proper treatment and support, people with mental illnesses can lead fulfilling and productive lives.
At A Glance
- Living with a family member with mental illness can have a significant impact on both the member and the family caregiver.
- Caring for a loved one with a mental illness can cause emotional, and physical strain, leading to guilt, and burnout.
- The presence of mental health issues in a loved one can be stressful due to the judgment of others and financial strain.
- Mental health symptoms can affect relationships including communication difficulties, behavioral changes, and social isolation.
- Caregivers of individuals with mental illness should provide emotional support, educate themselves, and seek professional help.
Frequently Asked Questions (FAQs)
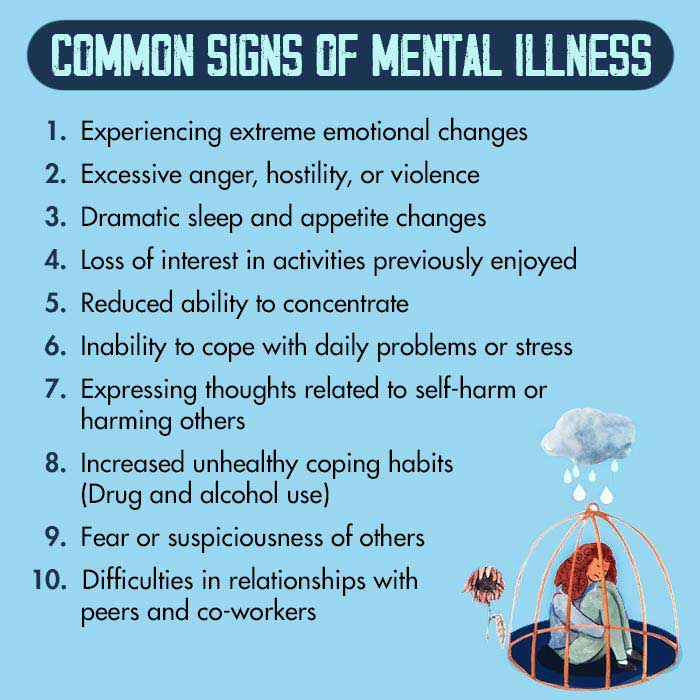
1. What are some common symptoms of mental illness?
Common symptoms of mental illness can vary depending on the specific diagnosis, but can include changes in mood, behavior, and thought patterns, such as in cases with depression, anxiety, irritability, paranoia, hallucinations, and delusions.
2. How to live with someone who has a mental illness?
Living with someone who has mental illness involves creating a supportive environment, encouraging treatment and therapy, seeking for support and help, setting boundaries, and practicing self-care.