Night Eating Syndrome is an eating disorder that involves overeating at night accompanied by sleeping problems. It is characterized by insomnia, eating at night after going to bed, and having a loss of appetite the next morning.
What Is Night Eating Syndrome (NES)?
Night eating syndrome is marked by excessive eating at night and having a delayed circadian pattern. Although binge eating disorder may be a comorbid condition, it differs from binge eating by the amount of food consumed at night and loss of control in the food intake. Night Eating Syndrome is classified as “other specified feeding or eating disorder” by the Diagnostic and Statistical Manual of Mental Disorders, fifth edition (DSM 5). This syndrome is often associated with nocturnal hyperphagia, insomnia & morning anorexia which can last for over 3 months.
One study 1 O’Reardon, J. P., Peshek, A., & Allison, K. C. (2005). Night eating syndrome: diagnosis, epidemiology and management. CNS drugs, 19(12), 997–1008. https://doi.org/10.2165/00023210-200519120-00003 explains that it is characterized by a gap or setback in the circadian timing of consumption of food. “Energy intake is reduced in the first half of the day and greatly increased in the second half, causing sleep disruption in the service of food consumption,” adds the study. NES is separate from both binge eating disorder and bulimia nervosa 2 Jain A, Yilanli M. Bulimia Nervosa. [Updated 2021 Aug 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK562178/ as it does not involve the related compensatory behaviors. Moreover, the time of food consumption and the amount of food intake is also largely different in this syndrome.
Night eating syndrome was first recognized by psychiatrist Albert Stunkard, in 1955. He saw it as a behavioral variation of obesity. As a result, this condition is mostly studied in relation to obesity. Research on the relation between NES and eating disorders is very limited. It can be treated with different treatment methods such as cognitive behavioral therapy, light exposure, and medications. People undergoing treatment often tend to develop strict and consistent bed timing in order to develop coping strategies.
Read More About Binge Eating Disorder Here
Understanding Night Eating Syndrome
Humans tend to correspond with appetite and food consumption in the primary hours of wakefulness. This means that meals are generally consumed between early morning and early evening. However, individuals with this condition retain a normal sleep cycle but display a delayed food intake pattern. These people seem to have a disruption in their circadian rhythm, the biological clock that regulates our sleeping and eating patterns based on the natural cycle of darkness and light.
People with this condition are fully aware while they are eating at night but tend to remember it afterward. They also may experience depression or anxiety and this can both be a cause and result of night eating syndrome. A 2012 study 3 Allison, K. C., & Tarves, E. P. (2011). Treatment of night eating syndrome. The Psychiatric clinics of North America, 34(4), 785–796. https://doi.org/10.1016/j.psc.2011.08.002 defined night eating syndrome as “a delay in the circadian rhythm of eating, characterized by appetite suppression during morning hours and appetite increase during evening hours”.
People with this condition tend to eat at night because they believe that it will ultimately help them to sleep at night or fall back asleep. A central feature of this syndrome involves “if I don’t eat, I won’t be able to sleep”. They may also have no appetite in the morning and feel guilt and shame for eating at night. In order to be diagnosed with this condition, the individual must be fully aware of the night eating in order to differentiate it from parasomnia and other sleep-related disorders.
Prevalence Of Night Eating Syndrome
NES affects both men and women. The prevalence rate 4 Rand, C. S., Macgregor, A. M., & Stunkard, A. J. (1997). The night eating syndrome in the general population and among postoperative obesity surgery patients. The International journal of eating disorders, 22(1), 65–69. https://doi.org/10.1002/(sici)1098-108x(199707)22:1<65::aid-eat8>3.0.co;2-0 of this condition is between 1 and 2 percent of the general population and approximately 10 percent of obese individuals. The age of onset 5 Vander Wal J. S. (2012). Night eating syndrome: a critical review of the literature. Clinical psychology review, 32(1), 49–59. https://doi.org/10.1016/j.cpr.2011.11.001 is typically in early adulthood and is often long lasting. A critical review 6 Allison, K. C., Ahima, R. S., O’Reardon, J. P., Dinges, D. F., Sharma, V., Cummings, D. E., Heo, M., Martino, N. S., & Stunkard, A. J. (2005). Neuroendocrine profiles associated with energy intake, sleep, and stress in the night eating syndrome. The Journal of clinical endocrinology and metabolism, 90(11), 6214–6217. https://doi.org/10.1210/jc.2005-1018 also found that people with NES also experience a depressed mood and anxiety disorders. Studies 7 Allison, K. C., Lundgren, J. D., O’Reardon, J. P., Geliebter, A., Gluck, M. E., Vinai, P., Mitchell, J. E., Schenck, C. H., Howell, M. J., Crow, S. J., Engel, S., Latzer, Y., Tzischinsky, O., Mahowald, M. W., & Stunkard, A. J. (2010). Proposed diagnostic criteria for night eating syndrome. The International journal of eating disorders, 43(3), 241–247. https://doi.org/10.1002/eat.20693 show that approximately 7 percent to 25 percent of people with this condition also meet the criteria for binge eating disorder. Research 8 Tu, C. Y., Meg Tseng, M. C., & Chang, C. H. (2019). Night eating syndrome in patients with eating disorders: Is night eating syndrome distinct from bulimia nervosa?. Journal of the Formosan Medical Association = Taiwan yi zhi, 118(6), 1038–1046. https://doi.org/10.1016/j.jfma.2018.10.010 also found that those with bulimia nervosa, 40% of inpatients and 50% of outpatients reported night eating symptoms.
Symptoms Of Night Eating Syndrome
If a person is suffering from this condition, they are more likely to consume at least a quarter of their daily calories after dinner. The individual wakes up at least twice a week and experiences at least three of the following symptoms:
- Lack of appetite in the morning
- A strong urgency to eat between dinner and sleep
- Insomnia four or five nights a week
- A belief that eating is necessary to go back to sleep
- A depressed mood that worsens during evening hours
- The daily pattern of food consumption displays increased intake in the night
- The individual is aware or can recall the night eating episodes
- Usually skips breakfast for most days
- Difficulty to fall back asleep or remain asleep without eating
Read More About Binge Insomnia Here
Causes Of Night Eating Syndrome
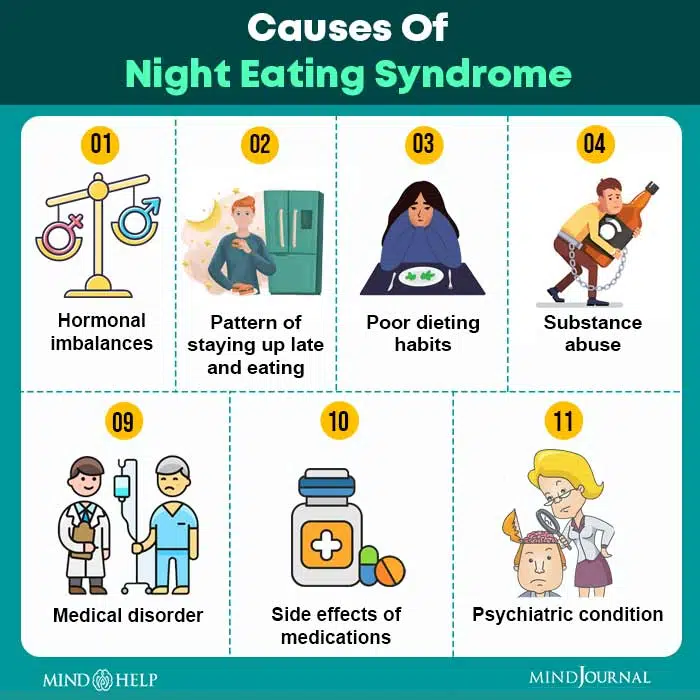
The causes may involve a variety of contributing factors. However, the exact causes of this condition are still unknown. Some of the causes may include:
- Hormonal imbalances that disrupt eating patterns
- A pattern of staying up late and eating late at night
- Poor dieting habits. The body gets used to physical deprivation of food during the day. The drive to eat later in the day is a normal response to restriction. With time, the self-soothing pattern of eating at night may develop into a habit.
- Substance abuse
- Medical disorder
- Side effects of medications
- Psychiatric condition
Diagnosis Of Night Eating Syndrome
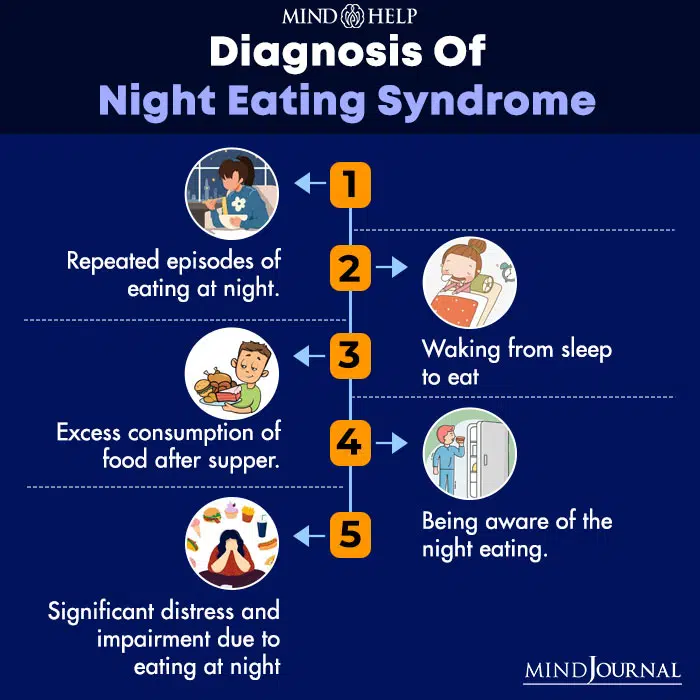
It is important to seek medical attention in case you experience any symptoms of this condition. The doctor will ask several questions regarding your sleeping and eating habits. The doctor may also evaluate your condition with a detailed questionnaire. The diagnosis may also involve a sleep test called polysomnography 9 Rundo, J. V., & Downey, R., 3rd (2019). Polysomnography. Handbook of clinical neurology, 160, 381–392. https://doi.org/10.1016/B978-0-444-64032-1.00025-4 . This test measures brain waves, blood oxygen levels, and heart rates. It usually occurs at a hospital or a sleep center.
The diagnostic criteria 10 O’Reardon, J. P., Peshek, A., & Allison, K. C. (2005). Night eating syndrome : diagnosis, epidemiology and management. CNS drugs, 19(12), 997–1008. https://doi.org/10.2165/00023210-200519120-00003 for night eating syndrome are:
- Repeated episodes of eating at night
- Waking from sleep to eat
- Excess consumption of food after supper
- Being aware of the night eating
- Significant distress and impairment due to eating at night
In order to be diagnosed with this syndrome, the patient must overeat at night for at least three months. Diagnosis of this condition can also be done through assessments via the Night Eating Questionnaire (NEQ), The Night Eating Diagnostic Scale (NEDS), and Night Eating Syndrome History. These questions are self report measures that are used to arrive at a correct diagnosis.
Treatment For Night Eating Syndrome

There are several treatment options that can be adopted to treat patients with this syndrome. This condition is often tied with obesity and it often makes it tough to lose weight. It is worth mentioning that not everyone with NES is obese. Sleep troubles or insomnia also is a contributing factor in gaining weight. Hence, it is important to adopt treatment therapies in your daily routine in order to lead a healthy and happy lifestyle. Some of the treatment options adopted by doctors are as follows:
1. Cognitive Behavioral Therapy (CBT)
Studies 11 Berner, L. A., & Allison, K. C. (2013). Behavioral management of night eating disorders. Psychology research and behavior management, 6, 1–8. https://doi.org/10.2147/PRBM.S31929 found that this therapy is one of the most effective treatment methods for this disorder. Cognitive Behavioral Therapy is used to identify and evaluate the negative thoughts and patterns that govern an individual’s behavior. These negative thoughts and patterns are then altered with positive ones to attain the desired outcome. This treatment includes educating themselves and self-monitoring to understand the disorder. The doctor will also help the patient to develop different coping strategies to help ease the symptoms. Regular routines may also be introduced such as meal planning and structuring regular eating routines. It can also involve a reduction in dieting.
The treatment also involves adding shifting eating patterns to earlier in the day in order to align better with sleep and wake cycles. It is a necessary step to break the cycle of eating at night. It can be done gradually by increasing the morning meal intake until a breakfast routine becomes easy every day.
Read More About Cognitive Behavioral Therapy (CBT) Here
2. Light Exposure Therapy
This therapy is also referred to as heliotherapy. It involves exposure to daylight or some equivalent form of light with the same intensity. During light therapy, the patient sits near a device called a light therapy box. This therapy is used to compensate for the lack of exposure to sunlight. The patient is required to use this therapy during the morning to reset the circadian rhythm. This will gradually enable the patient to break the cycle of eating at night. Experts believe that light therapy 12 Beauchamp, M. T., & Lundgren, J. D. (2016). A Systematic Review of Bright Light Therapy for Eating Disorders. The primary care companion for CNS disorders, 18(5), 10.4088/PCC.16r02008. https://doi.org/10.4088/PCC.16r02008 affects melatonin, a hormone that helps regulate circadian rhythms.
3. Progressive Muscle Relaxation (PMR)
Progressive muscle relaxation is a therapeutic treatment designed to achieve muscular relaxation through the tension and release of various muscle groups. It is a deep relaxation technique that is used to control stress, anxiety, and relieve insomnia. PMR is based on a simple practice of tensing or tightening one muscle group at a time followed by a relaxation phase with a release of tension. There is some evidence 13 Vander Wal, J. S., Maraldo, T. M., Vercellone, A. C., & Gagne, D. A. (2015). Education, progressive muscle relaxation therapy, and exercise for the treatment of night eating syndrome. A pilot study. Appetite, 89, 136–144. https://doi.org/10.1016/j.appet.2015.01.024 that using PMR techniques can help ease the symptoms.
4. Medications
There is little evidence that supports the use of psychiatric medications for treating eating disorders. However, some medications tend to work in cases of patients with NES. Medications that are usually prescribed include selective serotonin reuptake inhibitors (SSRIs) including paroxetine (Paxil), fluvoxamine (Luvox), and sertraline (Zoloft).
Read More About Meditation Here
Prevention Of Night Eating Syndrome
Here are a few preventive steps that can help someone to cope with this condition:
1. Monitor Your Eating Patterns
In order to change your night eating patterns, it is crucial to monitor your daily eating habits. This includes what you eat, when you eat, what you are thinking about while eating, what are you feeling, and the level of hunger before, during, and after the episode. By monitoring your patterns you will be able to make the conscious decision to stop eating. This will also allow you to understand why you have developed this habit.
2. Don’t Skip Meals
People with this condition skip breakfast and hardly have a proper meal during the day. Hence, it is essential not to skip meals during the day. One of the reasons why you may be consuming food after dinner is that you probably are starving during the day. You have to keep a balance on the daily calorie intake that is spread evenly throughout the day. This will help you to adopt a regular healthy eating pattern. So in order to stop eating in the middle of the night, you need to follow an eating schedule so that your body can retrain itself in accordance with the new schedule.
3. Don’t Eat In The Bedroom
If you want to stop eating in the middle of the night it is important to completely stop eating in the bedroom. It is more likely that all the eating episodes are occurring in the bedroom. This makes the bedroom a conditioned stimulus. This means that whenever you enter the bedroom your hunger signals in the brain get triggered and you feel compelled to eat.
So once you condition your brain about not eating in the bedroom, the hunger signals will no longer get triggered when you go to bed at night. As a result, this will improve your quality of sleep and break your unhealthy eating patterns.
4. Adopt Relaxation Techniques
You need to remember that the urgency to eat at night will come and go. So you need to control the urgency and not give in. You can do this by adopting relaxation techniques. This can include mindful meditation 14 Katterman, S. N., Kleinman, B. M., Hood, M. M., Nackers, L. M., & Corsica, J. A. (2014). Mindfulness meditation as an intervention for binge eating, emotional eating, and weight loss: a systematic review. Eating behaviors, 15(2), 197–204. https://doi.org/10.1016/j.eatbeh.2014.01.005 and progressive muscle relaxation. These relaxation techniques can prevent you from acting on your urge immediately. By placing your attention on the relaxation techniques, you will realize that the intensity of the urge decreases substantially.
5. Exercise Regularly
Exercising 15 Cook, B. J., Wonderlich, S. A., Mitchell, J. E., Thompson, R., Sherman, R., & McCallum, K. (2016). Exercise in Eating Disorders Treatment: Systematic Review and Proposal of Guidelines. Medicine and science in sports and exercise, 48(7), 1408–1414. https://doi.org/10.1249/MSS.0000000000000912 regularly can actually help you to manage your urges because of the positive effects it has on sleep. Regular exercise works wonders on sleeping patterns, thus improving the quality of sleep. A reason why people eat so much is that they can’t initiate or sustain sleep. Exercising regularly can help to manage the symptoms of this condition.
Recovering From Night Eating Syndrome
It is important to seek medical attention if you are experiencing any symptoms of this syndrome. The patient may feel guilty or ashamed to seek treatment and that is why it is important for family members or spouses to encourage them. With therapy and medication, it is possible to recover and develop healthy sleeping and eating patterns.
Night Eating Syndrome At A Glance
- Night eating syndrome is an eating disorder involving overeating at night and disruptions in sleep.
- It is closely associated with delayed circadian patterns, loss of control over food intake, eating disorders, obesity, insomnia, anorexia, mental disorders, etc.
- Its symptoms involve loss of appetite, skipping regular meals, experiencing eating urgencies before bedtime, insomnia, and depressive moods.
- The causes of night eating syndrome is attributed to hormonal imbalances, disrupted circadian clocks, poor eating and sleeping patterns, physical comorbidities, psychiatric disorders, etc.
- Night eating syndromes can be diagnosed with psychotherapies, medication, exercising and meditation, following a healthy schedule, implementing self-help strategies, etc.















