Table of Contents
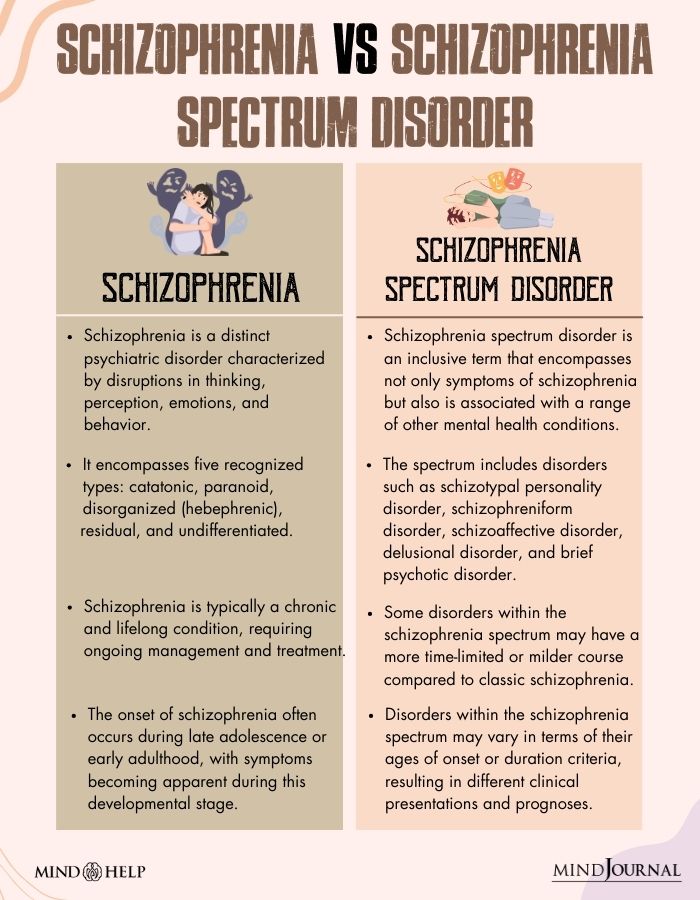
Schizophrenia spectrum disorder (SSD) is a complex and multifaceted psychiatric condition that includes a range of mental health disorders. It is characterized by disruptions in thinking, perception, emotions, and behavior.
What Is Schizophrenia Spectrum Disorder?
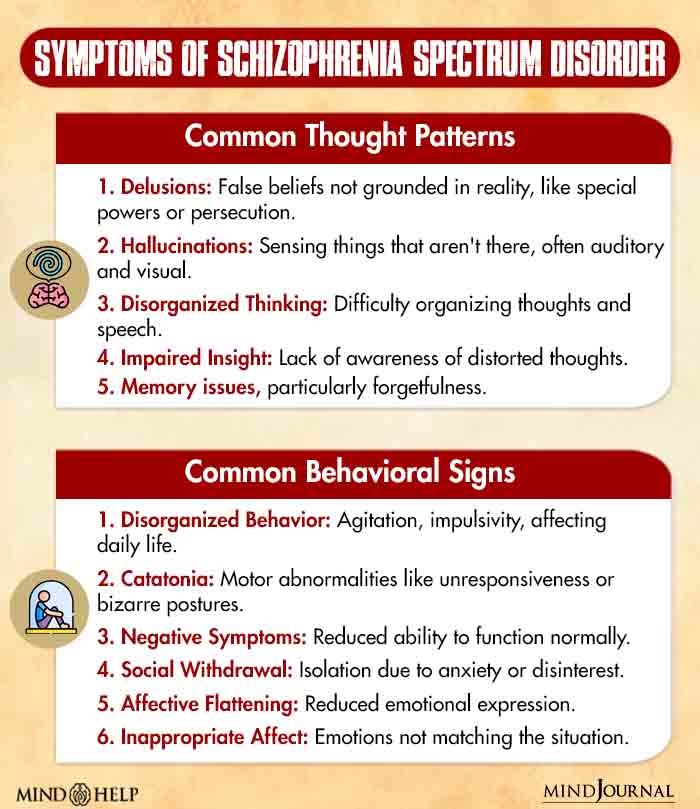
Schizophrenia spectrum disorder (SSD) is a mental health disorder characterized by a range of symptoms, including delusions, hallucinations, etc. Considered both a neuro-developmental disorder and a psychotic disorder 1 Cuthbert, B. N., & Morris, S. E. (2021). Evolving Concepts of the Schizophrenia Spectrum: A Research Domain Criteria Perspective. Frontiers in psychiatry, 12, 641319. https://doi.org/10.3389/fpsyt.2021.641319 , it typically emerges in late adolescence or early adulthood.
Schizophrenia spectrum disorder includes a range of severity levels and symptoms, which is why it’s described as a ‘spectrum’. While this variability makes classification difficult, individuals across the spectrum often share certain core thoughts, behaviors, and symptoms.
Cinematic Encounters: Schizophrenia Spectrum Disorder
The disorder has indeed been a recurring theme in cinema 2 Cuthbert, B. N., & Morris, S. E. (2021). Evolving Concepts of the Schizophrenia Spectrum: A Research Domain Criteria Perspective. Frontiers in psychiatry, 12, 641319. https://doi.org/10.3389/fpsyt.2021.641319 . These films often feature protagonists who display a fragmented mind ravaged by the typical symptoms of schizophrenia spectrum disorder. For instance, A Beautiful Mind (2001) portrays the real-life story of mathematician John Nash, highlighting his struggles with schizophrenia spectrum disorder and the power of human resilience.
Donnie Darko (2001) explores the blurred line between reality and delusion in the mind of its titular character, showcasing the disorienting effects of the disorder. Shutter Island (2010) further delves into the psychological complexities of a protagonist suffering from schizophrenia spectrum disorder—challenging the audience to question the boundaries of sanity and insanity.
Prevalence of Schizophrenia Spectrum Disorder
Schizophrenia spectrum disorder is a rare disorder that affects approximately 0.3% to 0.7% of the global population 3 Lindhardt, L., Nilsson, L. S., Munk-Jørgensen, P., Mortensen, O. S., Simonsen, E., & Nordgaard, J. (2022). Unrecognized schizophrenia spectrum and other mental disorders in youth disconnected from education and work-life. Frontiers in psychiatry, 13, 1015616. https://doi.org/10.3389/fpsyt.2022.1015616 , with variations in prevalence by region and demographics. The different types of schizophrenia spectrum disorder are often misdiagnosed as the general form of schizophrenia or psychosis.
Types Of Schizophrenia Spectrum Disorder
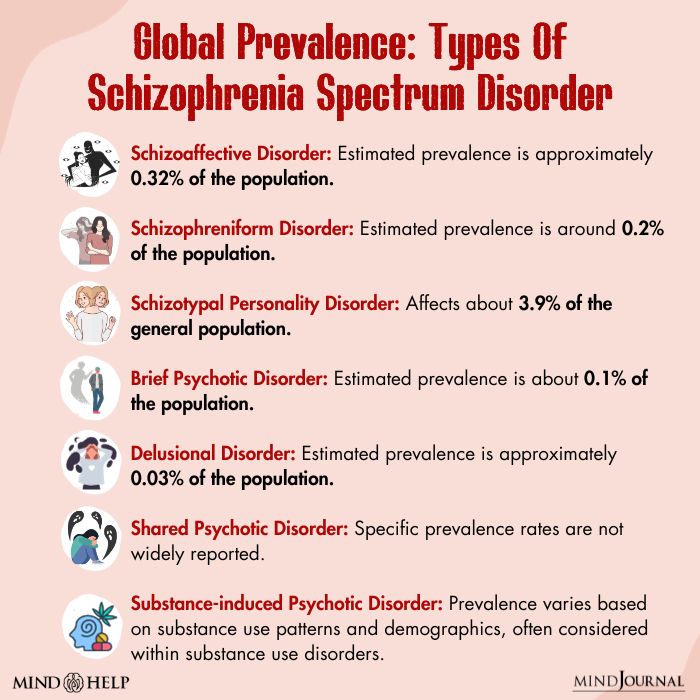
Some of the main 4 Lysaker, P. H., Pattison, M. L., Leonhardt, B. L., Phelps, S., & Vohs, J. L. (2018). Insight in schizophrenia spectrum disorders: relationship with behavior, mood and perceived quality of life, underlying causes and emerging treatments. World psychiatry : official journal of the World Psychiatric Association (WPA), 17(1), 12–23. https://doi.org/10.1002/wps.20508 types of schizophrenia spectrum disorder include:
1. Schizoaffective Disorder
The most common of all types of schizophrenia spectrum disorder, schizoaffective disorder makes individuals experience a combination of symptoms seen in schizophrenia. These include delusions (false beliefs) and hallucinations (perceiving things that are not there)—alongside concurrent mood disturbances, such as episodes of depression (including symptoms of sadness, loss of interest, and low energy) or mania (including symptoms of elevated mood, increased energy, and impulsive behavior).
Read More About Schizophrenia Here
2. Schizophreniform Disorder
It exhibits several similarities to the general form of schizophrenia, with the main distinction based on the duration of symptoms. If an individual experiences psychosis, delusions, disordered thinking, and inappropriate behaviors for a period exceeding one month but less than six months, these are likely to be diagnosed with schizophreniform disorder.
3. Schizotypal Personality Disorder
This disorder bears a resemblance to schizophrenia, but the episodes are less frequent, prolonged, and intense. Individuals with this disorder typically have some awareness of the distinction between their distorted ideas, experiences, and actual reality.
4. Brief Psychotic Disorder
It is a mental health condition characterized by hallucinations, delusions, and disorganized speech. In some cases, it may also involve “grossly disorganized or catatonic behavior,” which refers to a state of immobility or unresponsiveness. This condition typically lasts for a duration of one month or less.
5. Delusional Disorder
Delusional disorder is a mental health condition characterized by persistent, fixed, false beliefs (delusions) that last for at least a month. Individuals with this disorder can function relatively normally despite their delusions.
Read More About Delusional Disorder Here
6. Shared Psychotic Disorder
Shared psychotic disorder, also known as Folie à Deux, is a psychological phenomenon where one individual in a close relationship holds a delusion, and the other person adopts the same false and fixed belief. This shared delusion occurs due to the close emotional bond and influence between the two individuals.
Read More About Shared Psychotic Disorder Here
7. Substance-induced Psychotic Disorder
Substance-induced psychotic disorder is characterized by the presence of hallucinations and/or delusions that are directly caused by the effects of a substance or withdrawal from a substance. Symptoms can vary depending on the specific substance involved but may include perceptual disturbances (hallucinations), false beliefs, disorganized thinking, and impaired reality testing.
Causes Of Schizophrenia Spectrum Disorder
The development of the symptoms of schizophrenia spectrum disorder involves complex interactions 5 Rasmussen, A. R., Nordgaard, J., & Parnas, J. (2020). Schizophrenia-spectrum psychopathology in obsessive-compulsive disorder: an empirical study. European archives of psychiatry and clinical neuroscience, 270(8), 993–1002. https://doi.org/10.1007/s00406-019-01022-z between genetic, environmental, and neurobiological factors:
- Genetics
- Imbalances in the brain’s chemical messengers, including dopamine, glutamate, and serotonin levels.
- Structural and functional abnormalities in the brain
- Inborn cognitive difficulties (like attention and memory problems)
- Social and cultural adversity (such as urban living crisis, migration adversity, experiences of social discrimination, gender violence, etc.)
- Adverse family environments (characterized by criticism, hostility, and emotional over-involvement)
- Mental health disorders (like substance addiction 6 Tumenta, T., Oladeji, O., Gill, M., Khan, B. A., Olayinka, O., Ojimba, C., & Olupona, T. (2020). Substance Use Patterns and Schizophrenia Spectrum Disorders: A Retrospective Study of Inpatients at a Community Teaching Hospital. Journal of clinical medicine research, 12(12), 803–808. https://doi.org/10.14740/jocmr4380 , PTSD, depression, bipolar disorders, psychosis, etc.)
Read More About Genetics Here
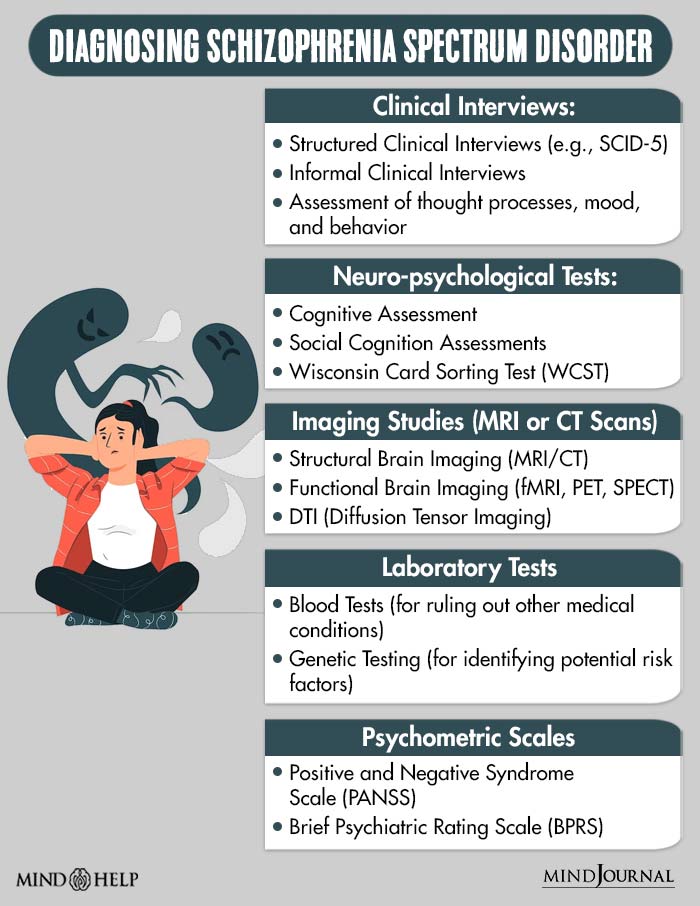
Diagnosis Of Schizophrenia Spectrum Disorder
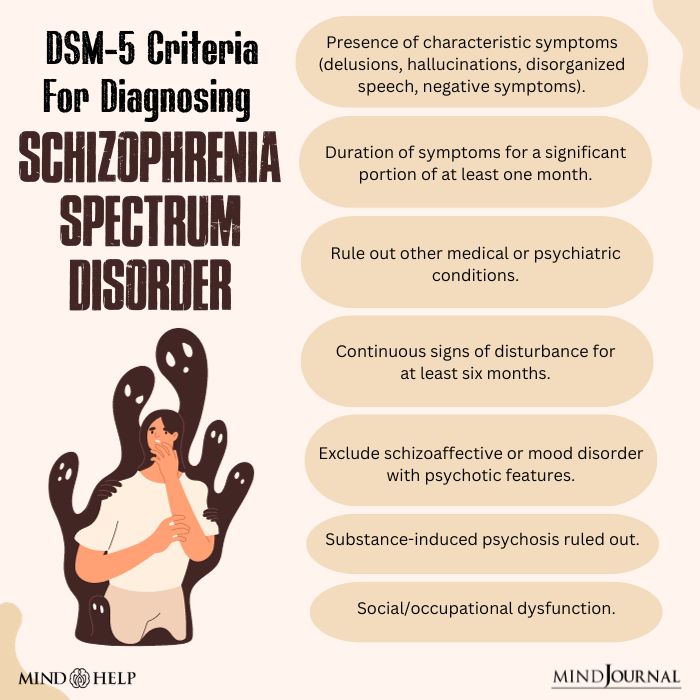
Diagnosing the various types of schizophrenia spectrum disorder (SSD) involves a structured process based on the DSM-5 criteria 7 Moura, B. M., van Rooijen, G., Schirmbeck, F., Wigman, H., Madeira, L., Harten, P. V., van Os, J., Bakker, P. R., Marcelis, M., & Genetic Risk and Outcome of Psychosis (GROUP) investigators (2021). A Network of Psychopathological, Cognitive, and Motor Symptoms in Schizophrenia Spectrum Disorders. Schizophrenia bulletin, 47(4), 915–926. https://doi.org/10.1093/schbul/sbab002 .
Mental health professionals, such as psychiatrists or psychologists, typically begin with a thorough clinical interview to evaluate the patient’s mental health history, the duration and intensity of symptoms, and any functional impairments. They also work to rule out other medical or psychiatric conditions that could present with similar symptoms. To support the diagnosis and guide treatment planning for schizophrenia spectrum disorders, additional tools like neuropsychological assessments, brain imaging (MRI or CT scans), and laboratory tests may be used.
Read More About DSM 5 Here
Schizophrenia Spectrum Disorder Treatment
Schizophrenia spectrum disorder treatment often involves a combination of therapies and medications 8 Chien, W. T., Leung, S. F., Yeung, F. K., & Wong, W. K. (2013). Current approaches to treatments for schizophrenia spectrum disorders, part II: psychosocial interventions and patient-focused perspectives in psychiatric care. Neuropsychiatric disease and treatment, 9, 1463–1481. https://doi.org/10.2147/NDT.S49263 tailored to the individual’s symptoms and needs:
1. Psychosocial Therapies
Therapeutic approaches 9 Chien, W. T., Leung, S. F., Yeung, F. K., & Wong, W. K. (2013). Current approaches to treatments for schizophrenia spectrum disorders, part II: psychosocial interventions and patient-focused perspectives in psychiatric care. Neuropsychiatric disease and treatment, 9, 1463–1481. https://doi.org/10.2147/NDT.S49263 in schizophrenia spectrum disorder treatment primarily include cognitive behavioral therapy (CBT), which aids individuals in managing distressing symptoms, enhancing coping skills, and challenging delusional beliefs. Additionally, involving family members in family therapy can foster understanding, communication, and vital support networks.
Individual therapy offers a secure environment for discussing personal experiences and emotions, while social skills training focuses on improving interpersonal and social functioning, ultimately contributing to a comprehensive treatment plan for individuals with SSD.
2. Medication
Antipsychotic medications 10 Huang, M. W., Gibson, R. C., Jayaram, M. B., & Caroff, S. N. (2022). Antipsychotics for schizophrenia spectrum disorders with catatonic symptoms. The Cochrane database of systematic reviews, 7(7), CD013100. https://doi.org/10.1002/14651858.CD013100.pub2 (First and Second Generation) are the cornerstone of schizophrenia spectrum disorder treatment and can help alleviate positive symptoms such as hallucinations and delusions. Moreover, long-acting injectable antipsychotics 11 Sommer, I. E., Slotema, C. W., Daskalakis, Z. J., Derks, E. M., Blom, J. D., & van der Gaag, M. (2012). The treatment of hallucinations in schizophrenia spectrum disorders. Schizophrenia bulletin, 38(4), 704–714. https://doi.org/10.1093/schbul/sbs034 are administered monthly or less frequently and can enhance medication adherence.
Lastly, adjunctive medications 12 Nitta, M., Kishimoto, T., Müller, N., Weiser, M., Davidson, M., Kane, J. M., & Correll, C. U. (2013). Adjunctive use of nonsteroidal anti-inflammatory drugs for schizophrenia: a meta-analytic investigation of randomized controlled trials. Schizophrenia bulletin, 39(6), 1230–1241. https://doi.org/10.1093/schbul/sbt070 like mood stabilizers, antidepressants, or anti-anxiety medications may be prescribed to address specific symptoms or comorbid conditions.
3. Hospitalization
In severe cases of SSD or during acute episodes, hospitalization may be necessary to stabilize the individual and ensure his/her safety.
Non-medical Aid For People With Schizophrenia Spectrum Disorder
Supportive measures 13 Stevović, L. I., Repišti, S., Radojičić, T., Sartorius, N., Tomori, S., Kulenović, A. D., Popova, A., Kuzman, M. R., Vlachos, I. I., Statovci, S., Bandati, A., Novotni, A., Bajraktarov, S., Panfil, A. L., Maric, N., Delić, M., & Jovanović, N. (2022). Non-pharmacological interventions for schizophrenia-analysis of treatment guidelines and implementation in 12 Southeast European countries. Schizophrenia (Heidelberg, Germany), 8(1), 10. https://doi.org/10.1038/s41537-022-00226-y for individuals with different types of schizophrenia spectrum disorder (SSD) can benefit their physical and mental well-being in the long run. These include vocational rehabilitation for employment assistance, supported housing for stable living arrangements, and case management to aid with daily tasks and care coordination.
Additionally, encouraging self-help and education through participation in support groups can enhance coping, while providing legal and financial support is crucial for overall well-being. Some individuals may also benefit from complementary therapies 14 Bighelli, I., Wallis, S., Reitmeir, C., Schwermann, F., Salahuddin, N. H., & Leucht, S. (2023). Effects of psychological treatments on functioning in people with Schizophrenia: a systematic review and meta-analysis of randomized controlled trials. European archives of psychiatry and clinical neuroscience, 273(4), 779–810. https://doi.org/10.1007/s00406-022-01526-1 like mindfulness, art therapy, or exercise 15 Böge, K., Karadza, A., Fuchs, L. M., Ehlen, F., Ta, T. M. T., Thomas, N., Bajbouj, M., & Hahn, E. (2020). Mindfulness-Based Interventions for In-Patients With Schizophrenia Spectrum Disorders-A Qualitative Approach. Frontiers in psychiatry, 11, 600. https://doi.org/10.3389/fpsyt.2020.00600 as adjunctive treatments.

Coping With Schizophrenia Spectrum Disorder
Consider the following measures 16 Holubova, M., Prasko, J., Hruby, R., Latalova, K., Kamaradova, D., Marackova, M., Slepecky, M., & Gubova, T. (2016). Coping strategies and self-stigma in patients with schizophrenia-spectrum disorders. Patient preference and adherence, 10, 1151–1158. https://doi.org/10.2147/PPA.S106437 for coping with the symptoms of schizophrenia spectrum disorder:
- Treatment adherence: Consistently attend therapy sessions and take prescribed medications. Stick to your schizophrenia spectrum disorder treatment plan.
- Psychoeducation: Learn about the disorder to help you cope more effectively.
- Track symptoms: Monitor shifts in mood and any occurrences of hallucinations.
- Seek professional help: Consider reaching out to a mental health professional for extra support.
- Crisis plan: Develop a plan for managing crisis situations.
- Set realistic goals: Break tasks into manageable steps.
- Healthy lifestyle: Maintain regular sleep, exercise, and a balanced diet.
- Avoid substance use: Refrain from alcohol or illicit drug use.
- Stress management: Use relaxation and stress-reduction strategies like meditation, yoga, etc.
- Social support: Build a strong support network with friends and family.
Read More About Stress Management Here
Takeaway
Addressing the symptoms of schizophrenia spectrum disorder alone is challenging because of the inherent complexity of the condition. Individuals with SSD often struggle to recognize the full extent of their symptoms, and the disorder can manifest in diverse and distressing ways. Coping with the disorder, even with comprehensive schizophrenia spectrum disorder treatment, can be an arduous journey marked by periods of relapse and fluctuating symptom severity. This is where social and professional support become critically important.
Social support networks, including family, friends, and support groups, offer understanding, encouragement, and a sense of belonging, which can alleviate the isolation and stigma that often accompany SSD. Professional help from mental health experts can help understand better “what is schizophrenia spectrum disorder” and ensure the implementation of evidence-based treatments, ongoing monitoring, and adjustments to treatment plans. This can contribute to the affected individual’s recovery and long-term stability.
At A Glance
- Schizophrenia spectrum disorder (SSD) is a complex mental health disorder characterized by a range of psychiatric symptoms.
- It is considered a neuro-developmental and psychotic disorder and is challenging to categorize due to its diverse symptoms.
- Hallucinations and delusions constitute the most common symptoms of schizophrenia spectrum disorder.
- Various types of schizophrenia spectrum disorder include schizoaffective disorder, schizophreniform disorder, schizotypal personality disorder, brief psychotic disorder, delusional disorder, shared psychotic disorder, and substance-induced psychotic disorder.
- The causes of SSD involve genetic, environmental, and neurobiological factors.
- Schizophrenia spectrum disorder treatment typically combines psychosocial therapies, medication, and non-medical support, with antipsychotic medications playing a central role.
Frequently Asked Questions
1. Which schizophrenia spectrum disorder is the most prevalent?
Schizophrenia, without specifying a particular subtype, is the most prevalent schizophrenia spectrum disorder.
2. How does schizophrenia spectrum disorder progress?
Schizophrenia spectrum disorders typically progress with the emergence of symptoms in late adolescence or early adulthood, followed by potential periods of exacerbation and remission.
3. What is the difference between schizophrenia spectrum disorder and paranoid schizophrenia?
Paranoid schizophrenia is a specific subtype of schizophrenia spectrum disorder characterized by prominent delusions of persecution and grandiosity. In contrast, schizophrenia spectrum disorder encompasses a range of psychotic disorders with various symptoms and presentations.
4. What is schizophrenia spectrum disorder support group?
A schizophrenia spectrum disorder support group is a meeting where individuals impacted by these disorders gather to share experiences and offer mutual support, often with professional facilitation.