Sleeplessness is the inability to fall asleep or being unable to enjoy good quality and quantity of sleep. It can be easily treated via a number of therapies, medication, and self-help strategies.
What Is Sleeplessness?
Sleeplessness is a condition in which a person experiences disturbed sleep-wake conditions. It is also known as insomnia 1 Levenson, J. C., Kay, D. B., & Buysse, D. J. (2015). The pathophysiology of insomnia. Chest, 147(4), 1179–1192. https://doi.org/10.1378/chest.14-1617 .
A person with sleeplessness usually reports difficult and disrupted sleep patterns. He/she has difficulty falling asleep or staying asleep and is usually plagued by conditions like daytime sleepiness, irritability, depressive moods, low energy, and sleep-related anxiety. This further leads to chronic motor disabilities, cognitive dysfunction, and severe mental and physical health issues, if left untreated.
Sleeplessness is a growing public health concern, both in children and adults. In some cases, sleeplessness is acute and short-term, lasting a few days or weeks. In other cases, sleeplessness is long-drawn, evolving into complex sleep disorders that last for months or years.
Studies 2 Bhaskar, S., Hemavathy, D., & Prasad, S. (2016). Prevalence of chronic insomnia in adult patients and its correlation with medical comorbidities. Journal of family medicine and primary care, 5(4), 780–784. https://doi.org/10.4103/2249-4863.201153 over the years have shown that sleeplessness has a worldwide prevalence, affecting 10%–30% of the population, some even as high as 50%–60%. It is common in older adults, females, and people with medical and mental ill health.
Symptoms
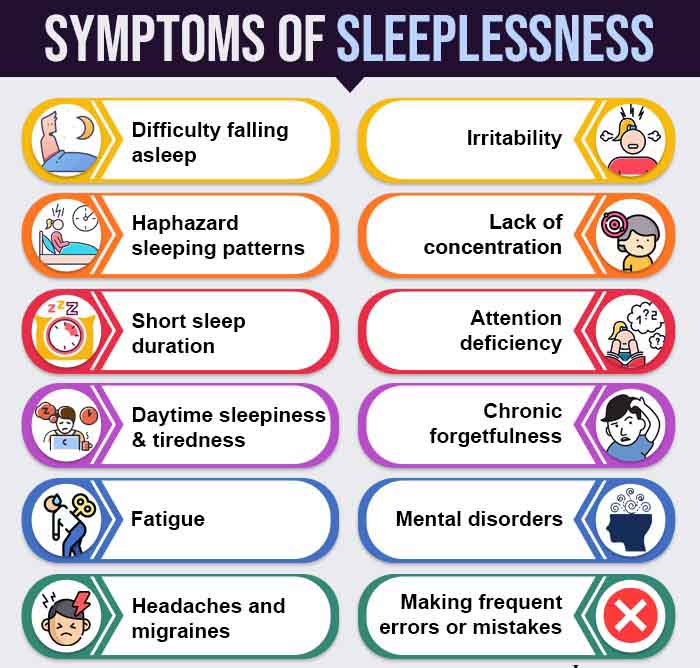
Merely losing sleep once in a while does not necessarily mean that you are suffering from a condition of sleeplessness or insomnia. These are some of the common symptoms to look out for in case of sleeplessness:
- Difficulty falling asleep
- Haphazard sleeping patterns
- Short sleep duration
- Daytime sleepiness
- Daytime tiredness
- Fatigue, exhaustion, and dizziness
- Experiencing headaches and migraines
- Experiencing irritability, lack of concentration, attention deficiency, forgetfulness, etc.
- Making frequent errors or mistakes
The Diagnostic and Statistical Manual of Mental Disorders (DSM) 3 American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). https://doi.org/10.1176/appi.books.9780890425596 suggests making a clinical diagnosis only if you are experiencing sleep difficulty for at least three nights a week for a period of three months or more.
Causes
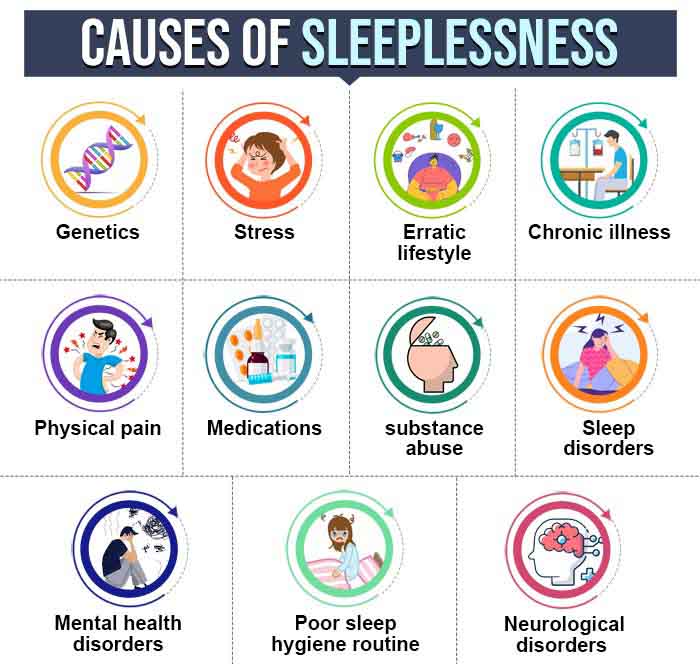
If you are wondering what causes sleeplessness, research has the following answers:
1. Genetics
Recent research 4 Gehrman, P. R., Keenan, B. T., Byrne, E. M., & Pack, A. I. (2015). Genetics of Sleep Disorders. The Psychiatric clinics of North America, 38(4), 667–681. https://doi.org/10.1016/j.psc.2015.07.004 reveals that sleep disorders can be partly due to genetic variability.
For instance, a 2015 study 5 Bidaki, R., Zarei, M., Khorram Toosi, A., & Hakim Shooshtari, M. (2012). A review on genetics of sleep disorders. Iranian journal of psychiatry and behavioral sciences, 6(1), 12–19. showed that a single gene mutation can cause sleep disorders like fatal familial insomnia, chronic primary insomnia, etc.
Read More About Genetics Here
2. Stress
Stress induces certain changes in our bodies’ physiological, hormonal and neuronal mechanisms that mediate sleep disruptions 6 Han, K. S., Kim, L., & Shim, I. (2012). Stress and sleep disorder. Experimental neurobiology, 21(4), 141–150. https://doi.org/10.5607/en.2012.21.4.141 .
Read More About Stress Here
3. Erratic lifestyle
Sedentary behavior 7 Yang, Y., Shin, J. C., Li, D., & An, R. (2017). Sedentary Behavior and Sleep Problems: a Systematic Review and Meta-Analysis. International journal of behavioral medicine, 24(4), 481–492. https://doi.org/10.1007/s12529-016-9609-0 and unhealthy lifestyles 8 Kanerva, N., Pietiläinen, O., Lallukka, T., Rahkonen, O., & Lahti, J. (2018). Unhealthy lifestyle and sleep problems as risk factors for increased direct employers’ cost of short-term sickness absence. Scandinavian journal of work, environment & health, 44(2), 192–201. https://doi.org/10.5271/sjweh.3695 (like those involving smoking, alcoholism, recreational drug use, etc.) cause derailment of body systems and lead to sleeping problems.
4. Poor sleep hygiene routine
A poor sleep hygiene routine fosters insufficient 9 Molla, A., & Wondie, T. (2021). Magnitude of Poor Sleep Hygiene Practice and Associated Factors among Medical Students in Ethiopia: A Cross-Sectional Study. Sleep disorders, 2021, 6611338. https://doi.org/10.1155/2021/6611338 and irregular 10 Yazdi, Z., Loukzadeh, Z., Moghaddam, P., & Jalilolghadr, S. (2016). Sleep Hygiene Practices and Their Relation to Sleep Quality in Medical Students of Qazvin University of Medical Sciences. Journal of caring sciences, 5(2), 153–160. https://doi.org/10.15171/jcs.2016.016 sleep habits that can lead to chronic or acute sleep disorders..
5. Physical illness and pain
According to a 2008 study 11 Tang N. K. (2008). Insomnia Co-Occurring with Chronic Pain: Clinical Features, Interaction, Assessments and Possible Interventions. Reviews in pain, 2(1), 2–7. https://doi.org/10.1177/204946370800200102 , people with a high prevalence of sleep complaints mostly suffer from physical ailments 12 Institute of Medicine (US) Committee on Sleep Medicine and Research; Colten HR, Altevogt BM, editors. Sleep Disorders and Sleep Deprivation: An Unmet Public Health Problem. Washington (DC): National Academies Press (US); 2006. 3, Extent and Health Consequences of Chronic Sleep Loss and Sleep Disorders. Available from: https://www.ncbi.nlm.nih.gov/books/NBK19961/ and chronic pain conditions, including arthritis, back/neck pain, headaches etc..
6. Medications and substance use
The use of medication or substances (like recreational drugs 13 Shibley, H. L., Malcolm, R. J., & Veatch, L. M. (2008). Adolescents with insomnia and substance abuse: consequences and comorbidities. Journal of psychiatric practice, 14(3), 146–153. https://doi.org/10.1097/01.pra.0000320113.30811.46 , alcohol 14 Fortuna, L. R., Cook, B., Porche, M. V., Wang, Y., Amaris, A. M., & Alegria, M. (2018). Sleep disturbance as a predictor of time to drug and alcohol use treatment in primary care. Sleep medicine, 42, 31–37. https://doi.org/10.1016/j.sleep.2017.12.009 , tobacco, narcotics, etc.) can interfere with your ability to fall or remain asleep, and can even alter your sleep cycles 15 Roehrs, T. A., & Roth, T. (2015). Sleep Disturbance in Substance Use Disorders. The Psychiatric clinics of North America, 38(4), 793–803. https://doi.org/10.1016/j.psc.2015.07.008 .
7. Neurological disorders (like stroke, dementia, epilepsy, etc.)
Degenerative and vascular diseases and neurological conditions involving the central nervous system (CNS) hinder your ability to fall asleep and/or continue to have a good sleep 16 Provini, F., Lombardi, C., & Lugaresi, E. (2005). Insomnia in neurological diseases. Seminars in neurology, 25(1), 81–89. https://doi.org/10.1055/s-2005-867074 .
Read More About Dementia Here
8. Sleep disorders (like sleep apnea, insomnia, narcolepsy, etc.)
The causes and effects 17 Abad, V. C., & Guilleminault, C. (2003). Diagnosis and treatment of sleep disorders: a brief review for clinicians. Dialogues in clinical neuroscience, 5(4), 371–388. https://doi.org/10.31887/DCNS.2003.5.4/vabad of sleeplessness are associated with different sleep disorders, such as sleep apnea, narcolepsy etc. 18 Karna B, Gupta V. Sleep Disorder. [Updated 2021 Nov 20]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK560720/ and are related to difficulty falling asleep, frequent arousals, breaks in sleep, and decrease in your total sleep time.
9. Other psychological disorders
Sleep problems are common among people with anxiety, depression, mood disorders, etc 19 Krystal A. D. (2012). Psychiatric disorders and sleep. Neurologic clinics, 30(4), 1389–1413. https://doi.org/10.1016/j.ncl.2012.08.018 .
Read More About Mood Disorders Here
Types
Based on the International Classification of Sleep Disorders (ICSD 20 Thorpy M. J. (2012). Classification of sleep disorders. Neurotherapeutics : the journal of the American Society for Experimental NeuroTherapeutics, 9(4), 687–701. https://doi.org/10.1007/s13311-012-0145-6 ) the different types of sleep disorders are:
1. Insomnia
Read More About Insomnia Here
2. Sleep-related breathing disorders
I. Obstructive sleep apnea (OSA)
II. Cheyne-Stokes respiration
III. Sleep-related hypoventilation disorders (like obesity hypoventilation syndrome, etc.)
IV. S-leeprelated hypoxia
V. Isolated symptoms
3. Central disorders of hypersomnolence
I. Narcolepsy
II. Idiopathic hypersomnia (IH)
III. Kleine-Levin syndrome (KLS)
IV. Insufficient sleep syndrome
V. Isolated symptoms
4. Circadian rhythm sleep-wake disorders
I. Delayed sleep-wake phase disorder (DSWPD)
II. Advanced sleep phase disorder (ASPD)
III. Irregular sleep-wake rhythm
IV. Non-24-hour sleep-wake rhythm disorder (N24)
V. Shift work disorder
VI. Jet lag disorder
Impact Of Sleep Deprivation
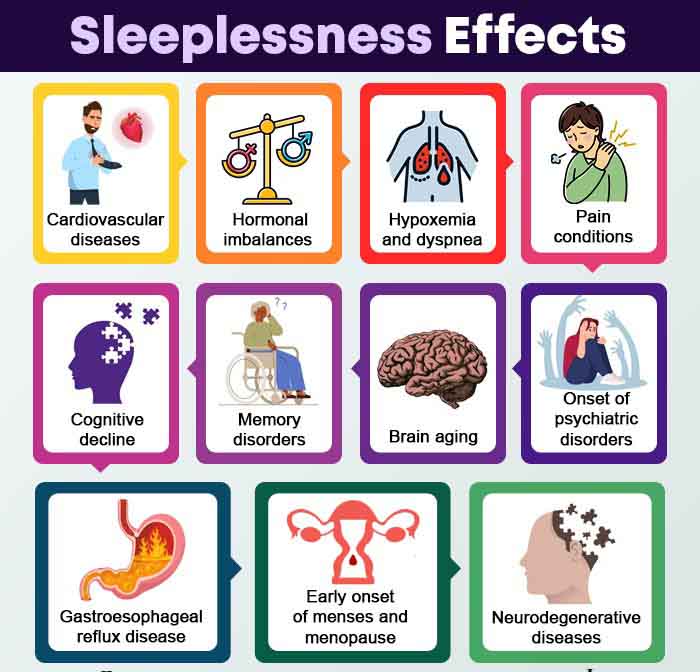
Sleeplessness can impact several areas of your life 21 Roth T. (2007). Insomnia: definition, prevalence, etiology, and consequences. Journal of clinical sleep medicine : JCSM : official publication of the American Academy of Sleep Medicine, 3(5 Suppl), S7–S10. such as:
- Your physical functioning
- Limitation in your ability to carry out different tasks due to physical and emotional problems
- Bodily pain
- Vitality
- Social functioning
- Other mental health problems
Further research 22 Roth T. (2007). Insomnia: definition, prevalence, etiology, and consequences. Journal of clinical sleep medicine : JCSM : official publication of the American Academy of Sleep Medicine, 3(5 Suppl), S7–S10. specifies the following comorbid medical disorders and psychiatric conditions that are induced by sleeplessness:
- Cardiovascular and coronary diseases
- Hormonal imbalances leading to diabetes, etc.
- Pain conditions
- Cognitive decline
- Memory disorders like dementia, Alzheimer’s disease (AD), etc.
- Early onset of menses and menopause
- Brain aging
- Onset of psychiatric disorders like depression, anxiety, stress disorders, etc.
Diagnosis
The diagnostic criteria for sleeplessness has been laid down by psychiatric manuals like the Diagnostic and Statistical Manual of Mental Disorders (DSM), the International Classification of Sleep Disorders (ICSD), etc. 23 Krystal, A. D., Prather, A. A., & Ashbrook, L. H. (2019). The assessment and management of insomnia: an update. World psychiatry : official journal of the World Psychiatric Association (WPA), 18(3), 337–352. https://doi.org/10.1002/wps.20674 , You might be due for a diagnosis of insomnia or other disorders relating to the lack of sleep, if you find yourself:
- Not being able to fall asleep or stay asleep
- Not sleeping despite having enough opportunity to
- Unable to function properly during the day
If you experience the above symptoms, it is recommended that you visit a psychiatrist as soon as possible.
Treatment
With prolonged wakefulness being a widespread phenomenon, research 24 Irish, L. A., Kline, C. E., Gunn, H. E., Buysse, D. J., & Hall, M. H. (2015). The role of sleep hygiene in promoting public health: A review of empirical evidence. Sleep Medicine Reviews, 22, 23-36. https://doi.org/10.1016/j.smrv.2014.10.001 suggests individual sleep hygiene recommendations 25 Buysse, D. J. (2014). Sleep health: Can we define it? Does it matter? Sleep, 37(1), 9-17. https://doi.org/10.5665/sleep.3298 along with medical aid to improve your sleep. While acute and transient sleep disorders go away with time, chronic sleeplessness requires serious medical attention, including hospitalization in serious cases.
To address chronic sleep disorders, a number of medical sleeplessness treatment options are available, including:
1. Therapy
A number of psychotherapies are available that address issues related to sleep restrictiveness, sleep disturbances, somatic arousal, and stimulus control. These include relaxation therapies such as progressive muscle relaxation, biofeedback, etc., cognitive behavioral therapies and multicomponent therapy.
2. Medication
Pharmacotherapy is often used to cure chronic and acute sleeplessness. According to a 2015 study 26 Lie, J. D., Tu, K. N., Shen, D. D., & Wong, B. M. (2015). Pharmacological Treatment of Insomnia. P & T : a peer-reviewed journal for formulary management, 40(11), 759–771. , the choice of drug used 27 Lippmann, S., Mazour, I., & Shahab, H. (2001). Insomnia: therapeutic approach. Southern medical journal, 94(9), 866–873. to address sleep disorders depends on a number of factors, namely, symptom pattern, treatment goals, patient preference, cost and availability of other treatments, comorbid conditions, etc.
3. Non-medical interventions
To address sleep problems, try availing non-medical interventions such as:
a. Stress management strategies
Stress management strategies, including both avoidant and coping techniques 28 Jesús Gázquez Linares, J., Pérez-Fuentes, M., Del Mar Molero Jurado, M., Fátima Oropesa Ruiz, N., Del Mar Simón Márquez, M., & Saracostti, M. (2019). Sleep Quality and the Mediating Role of Stress Management on Eating by Nursing Personnel. Nutrients, 11(8), 1731. https://doi.org/10.3390/nu11081731 , are useful in reducing stress and related sleep-onset problems.
Read More About Stress Management Here
b. ASMR techniques
Autonomous Sensory Meridian Response (ASMR) is a feeling of tingling sensations in the crown of the head, as a result of various audio-visual triggers such as whispering, tapping, and hand movements. According to experts, ASMR techniques in videos, podcasts, etc. can induce calm and mindfulness and reduce sleep problems 29 Poerio, G. L., Blakey, E., Hostler, T. J., & Veltri, T. (2018). More than a feeling: Autonomous sensory meridian response (ASMR) is characterized by reliable changes in affect and physiology. PloS one, 13(6), e0196645. https://doi.org/10.1371/journal.pone.0196645 .
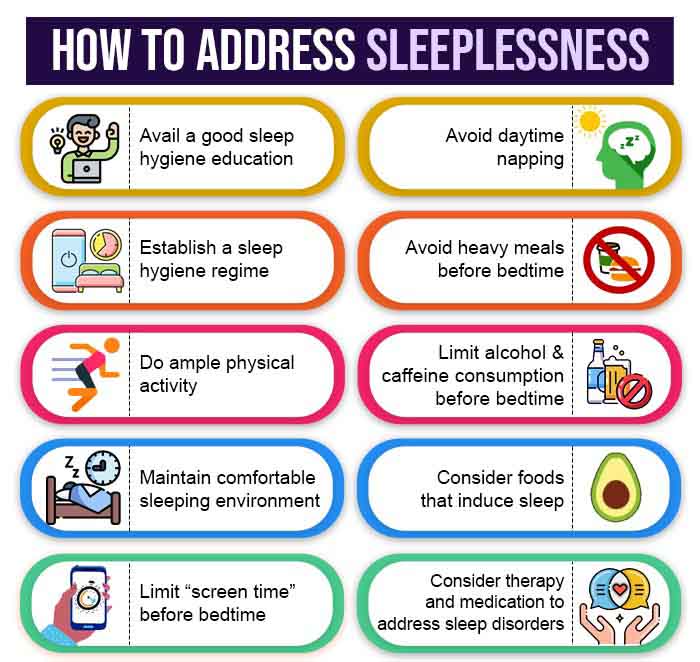
Self-Help Tips
Consider the following tips to sleep better at night:
1. A well–formulated sleep hygiene schedule
The most upfront and healthy cure for sleeplessness lie in formulating a healthy sleep hygiene schedule. This includes:
- Educating yourself about good sleep hygiene
- Establishing a realistic sleep schedule and maintaining this sleep timing with regularity every night
- Maintaining low light levels and comfortable temperature settings in the bedroom
- Creating a comfortable sleeping environment with mattresses, pillows, curtains, rugs, etc.
- Maintaining a data sheet for body type, sleep preferences, and the best sleep positions
- Limiting “screen time” before bedtime
- Considering activities like sex, cold shower, massages, etc. that enhance sleep
- Abstaining from daytime napping and resort to “power naps”, if necessary
2. Self-help tips
Consider the following self-help tips to reduce sleeplessness at night:
- Get adequate physical exercise throughout the day
- Consider mindfulness activities like meditation, yoga, massage, etc.
- Abstain from large meals and consumption of alcohol or caffeine in the hours leading to bedtime
- Avoid consumption of tobacco, nicotine, etc.
- Try home remedies for sleeplessness like food items that enhance sleep, such as nuts, white rice, milk products, fatty fish, lavender oil, chamomile tea, etc.
Takeaway
Sleeplessness and sleep disorders are health hazards that can impact your quality of life, financial prospects, social functioning, and physical and mental health. However, if treated timely with the right diagnosis, it can be managed. You can even overcome this condition by maintaining a disciplined lifestyle with a healthy sleep hygiene regime.
At A Glance
- Sleeplessness is the inability to fall asleep or enjoy a good quality or quantity of sleep.
- It is caused by a number of factors, including a stressful lifestyle, poor sleep hygiene routine, chronic illness, substance use, mental disorders, etc.
- There are 6 types of sleep disorders.
- If untreated, sleeplessness causes physical and mental disabilities, cognitive problems, etc.
- Sleeplessness can be easily cured by a number of therapies, medication, and self-help strategies.
Frequently Asked Questions (FAQs)
1. Can insomnia go away?
Acute or transient insomnia can go away on its own or with effective self-help strategies. But chronic insomnia is a more serious sleep disorder that requires medical attention.
2. What are the 5 sleep disorders?
The 5 types of sleep disorders include insomnia, sleep-related breathing disorders, central disorders of hypersomnolence, circadian rhythm sleep-wake disorders, and sleep related movement disorders.
3. What food can help you sleep?
Almonds and walnuts, chamomile tea, kiwi, tart cherry juice, fatty fish, and white rice are foods that induce sleep.
4. Does sleeping actually help sickness?
During sleep, our body regenerates the infection-fighting antibodies and immune cells and boosts the immune system. Therefore, adequate and good quality sleep can help reduce the risks of and prevent diseases like infectious diseases, obesity, diabetes, cardiovascular diseases, etc.















